Abstract
The transfusion of red blood cells (RBCs) is a crucial treatment for sickle cell disease (SCD). While often beneficial, the frequent use of transfusions is associated with numerous complications. Transfusions should be offered with specific guidelines in mind. Here we present updates to the indications for transfusion of RBCs in SCD. We review recent publications and include expert perspectives from hematology and transfusion medicine. For some clinical indications, such as ischemic stroke, the role of transfusion has been well studied and can be applied almost universally. For many other clinical scenarios, the use of transfusion therapy has less conclusive data and therefore must be tailored to individual needs. We highlight the roles of RBC transfusions in preventing or mitigating neurological disease, in reducing perioperative complications, in managing acute chest syndrome, and in optimizing pregnancy outcomes in SCD. We further highlight various transfusion techniques and when each might be considered. Potential complications of transfusion are also briefly discussed.
Learning Objectives
Understand how transfusion therapy is used for neurological disease in adults and children with SCD
Understand the role of transfusion therapy for ACS in adults and children with SCD
Understand how to evaluate transfusion therapy in pregnant women with SCD
Introduction
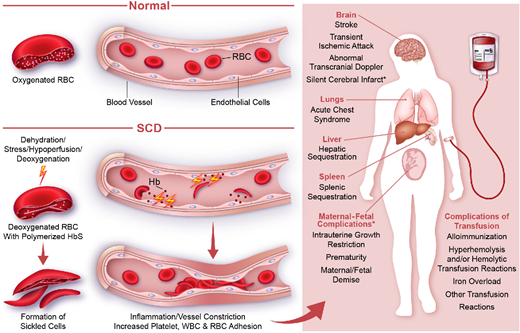
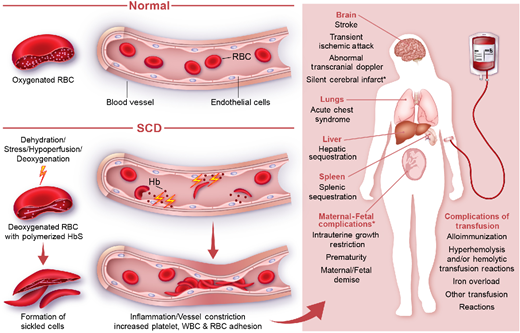
Sickle cell disease (SCD) is a red blood cell (RBC) disorder caused by a single nucleotide substitution in the β-globin allele on chromosome 6 that results in sickle hemoglobin (HbS).1,2 At low oxygen concentrations, HbS polymerizes, causing RBCs to distort into a crescent or sickle shape (Figure 1). These fragile, sickled RBCs lead to recurrent, severe pain and to progressive damage in nearly every organ system. Transfusion of RBCs mitigates, treats, or prevents a variety of complications of SCD (Table 1). Through RBC transfusion therapy, the burden of sickled cells is reduced, allowing for improved oxygen-carrying capacity and perfusion throughout the vascular system.1-3 RBCs can be delivered via simple transfusion or exchange transfusion (Table 2).1,4 In this article we review the indications for RBC transfusion in patients with SCD, discuss blood transfusion techniques, and briefly review the complications of RBC transfusion.
Indications for transfusion of RBCs in SCD. The pathophysiology of SCD renders transfusions useful for many complications. Consideration of the clinical scenario for an individual patient is always important, especially for some (*) indications for transfusion.
Indications for transfusion of RBCs in SCD. The pathophysiology of SCD renders transfusions useful for many complications. Consideration of the clinical scenario for an individual patient is always important, especially for some (*) indications for transfusion.
Indications for transfusion in SCD
| Indication . | Type of transfusion . |
|---|---|
| Acute transfusion indication | |
| Symptomatic anemia: aplastic crisis, acute splenic sequestration | Simple transfusion |
| Acute clinical stroke or TIA | Exchange transfusion |
| Acute hepatic sequestration/intrahepatic cholestasis | Simple or exchange transfusion |
| ACS | Simple or exchange transfusion |
| Acute multiorgan failure | Simple or exchange transfusion |
| Preoperative (surgeries lasting > 1 hour and require general anesthesia) | Simple or exchange transfusion |
| Pregnancy* | Simple or exchange transfusion |
| Chronic transfusion indication | |
| Primary stroke prevention | Simple or exchange transfusion |
| Secondary stroke prevention | Simple or exchange transfusion |
| Recurrent VOC | Simple or exchange transfusion |
| Indication . | Type of transfusion . |
|---|---|
| Acute transfusion indication | |
| Symptomatic anemia: aplastic crisis, acute splenic sequestration | Simple transfusion |
| Acute clinical stroke or TIA | Exchange transfusion |
| Acute hepatic sequestration/intrahepatic cholestasis | Simple or exchange transfusion |
| ACS | Simple or exchange transfusion |
| Acute multiorgan failure | Simple or exchange transfusion |
| Preoperative (surgeries lasting > 1 hour and require general anesthesia) | Simple or exchange transfusion |
| Pregnancy* | Simple or exchange transfusion |
| Chronic transfusion indication | |
| Primary stroke prevention | Simple or exchange transfusion |
| Secondary stroke prevention | Simple or exchange transfusion |
| Recurrent VOC | Simple or exchange transfusion |
Pregnant women with severe or frequent SCD-related complications or high-risk pregnancy.
Comparison between simple and exchange transfusion
| . | Simple transfusion . | Exchange transfusion . |
|---|---|---|
| Description | • Infuse donor blood without removing patient's blood | • Remove patient's blood during or shortly before infusing donor blood • May be partial or total exchange • May be performed manually or via apheresis |
| Indication/recommendation | • Acute anemia • Acute complications (ie, ACS) with Hb | • Severe ACS failing to respond to simple transfusion • Acute complications with Hb ≥9 g/dL • Conditions requiring reduced HbS percentage (ie, stroke/stroke prevention |
| Potential risks and/or limitations | • Hyperviscosity • Iron overload | • Iron overload (less frequent than simple transfusion) • May require central venous catheter • Requires specialized equipment and trained staff • Costly (compared to simple transfusion |
| . | Simple transfusion . | Exchange transfusion . |
|---|---|---|
| Description | • Infuse donor blood without removing patient's blood | • Remove patient's blood during or shortly before infusing donor blood • May be partial or total exchange • May be performed manually or via apheresis |
| Indication/recommendation | • Acute anemia • Acute complications (ie, ACS) with Hb | • Severe ACS failing to respond to simple transfusion • Acute complications with Hb ≥9 g/dL • Conditions requiring reduced HbS percentage (ie, stroke/stroke prevention |
| Potential risks and/or limitations | • Hyperviscosity • Iron overload | • Iron overload (less frequent than simple transfusion) • May require central venous catheter • Requires specialized equipment and trained staff • Costly (compared to simple transfusion |
CLINICAL CASE
Jane was 4 years old, with sickle cell disease (HbSS) diagnosed shortly after birth, when she first visited the pediatric hematology clinic. Routine pediatric hematology care had not been easily accessible to the family near their home, so the family had moved to initiate care at the clinic. Jane had been hospitalized once for vaso-occlusive crisis (VOC) as a toddler. She had received penicillin prophylaxis but had not previously been prescribed hydroxyurea or screening for stroke with transcranial doppler ultrasound (TCD). At the hematology clinic, hydroxyurea was initiated and escalated to maximum-tolerated dosing. Nonetheless, her 5-year-old TCD revealed abnormal velocities. The family was advised to begin chronic transfusion therapy to reduce her risk of stroke.
VOC
VOCs are a frequent manifestation of SCD. Transfusion therapy is not recommended for uncomplicated VOCs because multiple small studies have failed to show its effect on the course of hospitalization.5 However, in studies of stroke, subjects receiving chronic transfusions experienced fewer pain events during the period of transfusion therapy. In the Stroke Prevention Trial in Sickle Cell Anemia (STOP), patients receiving the standard of care reported nearly 3-fold more pain events per 100 patient-years than patients receiving transfusions (P = .014).6 In the Silent Cerebral Infarct Transfusion Multi-Center Clinical Trial, VOC pain occurred significantly more frequently in the observation group compared to the transfusion group (incidence rate ratio, 0.41; P = .04).7 Therefore, for recurrent VOC that is refractory to disease-modifying therapies, chronic transfusion may be considered as an adjunct or second-line therapy.1,3,5,8
Transfusion for stroke
Stroke accounts for significant morbidity and mortality among persons with SCD.3,9,10 Prior to the introduction of screening, approximately 11% of individuals with SCD would experience stroke before 20 years of age.11 The risk of recurrent stroke was approximately 70% within 2 years of the first stroke.3 Stroke-risk screening using TCD should begin around 2 years of age and is administered annually through age 16. Abnormal TCD, defined by a time-averaged mean velocity ≥200 cm/s in the internal carotid or middle cerebral artery, predicts a 40% risk of stroke within 3 years.8,12 The role of transfusion therapy in primary and secondary clinical stroke prevention and for management of acute ischemic stroke is well studied in pediatric populations with SCD and is strongly recommended (Table 3).2,8 There are no standard tools to assess stroke risk in adults with SCD. The data on stroke prevention in adults with SCD are limited, but current guidelines recommend chronic transfusion therapy for adults who have suffered ischemic stroke due to SCD.8 Very limited data are available to inform the use of transfusion therapy in hemorrhagic stroke.8
Clinical trials on treatment and prevention of ischemic stroke in SCD patients
| Clinical trial . | Description/outcome . |
|---|---|
| STOP 1 (Stroke Prevention Trial in Sickle Cell Anemia)52 | Children with abnormal TCD velocities who received long-term chronic transfusion to maintain HbS. |
| STOP 2 Trial 53 | Discontinuing chronic transfusion in children with normalized TCD led to increased rate of abnormal TCD conversion and stroke. Therefore, the trial recommends continuing transfusion therapy even after TCD velocities are normal. |
| TWiTCH (TCD With Transfusions Changing to Hydroxyurea)9 | Hydroxyurea is noninferior to transfusion for primary stroke prevention in children without cerebral vasculopathy or prior history of TIA who have received transfusion for at least 1 year. The optimal duration of transfusion prior to switching to hydroxyurea has not been established. |
| SWiTCH (Stroke With Transfusion Changing to Hydroxyurea)54 | Transfusion therapy is more effective than hydroxyurea in reducing secondary stroke in children. The trial closed early because approximately 10% of the patients treated with hydroxyurea/phlebotomy experienced a second stroke vs patients receiving chronic transfusion therapy. |
| SIT (Silent Cerebral Infarct Transfusion Multi-Center Clinical Trial)7 | Children with silent cerebral infarcts and normal or conditional TCD velocities who received chronic transfusion and maintained HbS. |
| Clinical trial . | Description/outcome . |
|---|---|
| STOP 1 (Stroke Prevention Trial in Sickle Cell Anemia)52 | Children with abnormal TCD velocities who received long-term chronic transfusion to maintain HbS. |
| STOP 2 Trial 53 | Discontinuing chronic transfusion in children with normalized TCD led to increased rate of abnormal TCD conversion and stroke. Therefore, the trial recommends continuing transfusion therapy even after TCD velocities are normal. |
| TWiTCH (TCD With Transfusions Changing to Hydroxyurea)9 | Hydroxyurea is noninferior to transfusion for primary stroke prevention in children without cerebral vasculopathy or prior history of TIA who have received transfusion for at least 1 year. The optimal duration of transfusion prior to switching to hydroxyurea has not been established. |
| SWiTCH (Stroke With Transfusion Changing to Hydroxyurea)54 | Transfusion therapy is more effective than hydroxyurea in reducing secondary stroke in children. The trial closed early because approximately 10% of the patients treated with hydroxyurea/phlebotomy experienced a second stroke vs patients receiving chronic transfusion therapy. |
| SIT (Silent Cerebral Infarct Transfusion Multi-Center Clinical Trial)7 | Children with silent cerebral infarcts and normal or conditional TCD velocities who received chronic transfusion and maintained HbS. |
The current practice for primary stroke prevention is to provide chronic transfusion to maintain HbS levels <30% for patients at high risk for stroke. Chronic transfusion therapy for primary stroke prevention should continue for at least 1 year. After 1 year, if TCD velocities have normalized and no silent strokes are identified, a gradual transition to hydroxyurea in patients without cerebral vasculopathy can be considered with careful monitoring.13 For prevention of recurrent stroke, indefinite chronic transfusion therapy to keep HbS <30% is recommended. Where chronic transfusion therapy is not available, especially in low- and middle-income countries, hydroxyurea should be provided for stroke prevention to children with an abnormal TCD.14
When children and adults with SCD present with signs or symptoms concerning for acute ischemic stroke or transient ischemic attack (TIA), transfusion should be performed to achieve HbS <30%.1,8,15 Transfusion should be provided as soon as possible and no more than 2 hours after presentation. There have been no prospective randomized trials comparing simple transfusion and exchange transfusion in the treatment of acute ischemic stroke. Exchange transfusion is often used because it can promptly reduce HbS to <30% while maintaining a stable blood volume (Table 1).4,8 A retrospective cohort study by Hulbert and colleagues demonstrated that using exchange transfusion at stroke presentation was associated with a lower risk of subsequent stroke compared to simple transfusion.16 However, a simple transfusion can be given while preparations are being made for exchange transfusion. Once ischemic stroke is confirmed, chronic transfusion should be continued long-term to prevent recurrent stroke.
Silent cerebral infarction (silent stroke) is the most common neurological injury in persons with SCD, occurring in 39% of children with HbSS disease,15,17 and is associated with significant morbidity. A recent meta-analysis examined 5 trials, comparing interventions to prevent silent stroke, and determined that in patients with abnormal TCD, chronic transfusion therapy may reduce the incidence of silent stroke.18 Chronic transfusion therapy is not expected to have an impact on the incidence of silent stroke in children with prior silent strokes or with normal/conditional TCDs.18 When silent stroke is identified by magnetic resonance imaging, transfusion therapy should be discussed with the patient and family.15
CLINICAL CASE (continued)
Jane remained in hematology care throughout her childhood. After 6 years of chronic transfusion therapy, she developed numerous auto- and alloantibodies. Her TCD velocities normalized, and she was successfully transitioned to hydroxyurea therapy. She was preparing to head to college at the end of the summer. Following a summer send-off party, she presented to the hospital with severe right upper quadrant pain. Jane described sharp, stabbing pain that developed a few hours after eating a cheeseburger, potato salad, and ice cream. In the hospital, an ultrasound was obtained and confirmed cholelithiasis. She was admitted to the hospital with a plan for a laparoscopic cholecystectomy. On admission, her complete blood count included the following: white blood cell count, 15.3 × 103/µL; Hb, 9.5 g/dL; mean corpuscular volume, 105 fL; absolute reticulocyte count, 358 × 103/µL. Amylase and lipase were within normal limits. Remembering her history of antibodies, Jane inquired about the need for preoperative transfusion. Because her Hb was above 9 g/dL, her medical team elected to forego preoperative transfusion and to ensure adequate hydration instead.
Preoperative transfusion
Patients with SCD often require cholecystectomy, splenectomy, and/or orthopedic procedures due to complications of SCD. Unfortunately, these patients are at increased risk for postoperative complications related to SCD. Acute chest syndrome (ACS) developed in 15.2% of pediatric patients with SCD undergoing splenectomy in 1 study and occurred in 5% of patients with SCD having a laparoscopic cholecystectomy in another. 19,20 Children who developed ACS following splenectomy had higher postoperative pain scores than those who did not.19 Planning for surgery in this population should involve communication between anesthesia, surgery, hematology, and transfusion medicine.21 Care should be taken to avoid triggers for crises, which include physiological stress, emotional stress, acidemia, hypoxia, and high blood viscosity. Perioperative fluid balance also needs to be carefully managed to avoid intracellular dehydration or volume overload.22
In the preoperative setting, the risks of transfusion need to be balanced against the benefits of lower HbS and improved oxygen-carrying capacity. The Transfusion Alternatives Preoperatively in Sickle Cell Disease (TAPS) study aimed to assess the benefits of prophylactic preoperative transfusion with a goal Hb 10g/dL versus no transfusion in patients with HbSS or HbSβ⁰-thalassemia scheduled for low- to medium-risk procedures.23 TAPS demonstrated that 39% of those who were not transfused had complications versus 15% in the transfused group (odds ratio, 3.8).23 Only 1 transfused person had alloimmunization as a result.23 When evaluating aggressive (HbS <30%) compared to conservative (Hb >10g/dL) target transfusions in the preoperative setting, a recent Cochrane review found no differences in perioperative or transfusion-related complications but did find low-quality evidence that preoperative transfusion could reduce the risk of ACS.24 The National Heart, Lung, and Blood Institute, American Society of Hematology (ASH), and British guidelines concur that persons with SCD undergoing high-risk procedures should be transfused preoperatively but offer caveats for various clinical scenarios (Table 4).8,25,26
Details of indications for transfusion from recent guidelines
| . | NHLBI (2014)22 . | BSH (2017)7 and BJH (2018)37 . | ASH (2020)21 . |
|---|---|---|---|
| Perioperative transfusion | • In HbSS disease, goal Hb 10 g/dL prior to undergoing a surgical procedure with general anesthesia. • In HbSS patients who require surgery and have an Hb >8.5 g/dL without transfusion, are on hydroxyurea, or need high-risk surgery (eg, neurosurgery, prolonged anesthesia, cardiac bypass), consult a sickle cell expert. • In HbSC or HbSβ +-thalassemia disease that requires a surgical procedure with general anesthesia, consult a sickle cell expert. | • In HbSS disease, goal Hb 10 g/dL prior to undergoing a surgical procedure with general anesthesia for low- or moderate-risk surgery. • In HbSS disease, full exchange transfusion, with a target HbS of <30%, for high-risk surgery (major neurosurgery, cardiothoracic) and for those with a high risk of perioperative complications (eg, severe organ damage or a history of complications). • In HbSC disease, give preoperative transfusion prior to moderate- and high-risk surgery. • All other patients undergoing surgery should be individually assessed. • Consider simple transfusion for patients with Hb <9 g/dL. • If Hb >9 g/dL and exchange transfusion would delay the surgery, it may be appropriate to proceed with surgery but to plan a postoperative transfusion if needed. | • For all SCD, recommend preoperative transfusion over no preoperative transfusion in patients undergoing surgeries requiring general anesthesia and lasting more than 1 hour. |
| Symptomatic ACS with Hb 1 g/dL below baseline | • Exchange or simple transfusion | • Exchange or simple transfusion | • Automated RCE, manual RCE, or simple transfusion |
| Symptomatic severe ACS (i.e., O2 saturation <90% with supplemental oxygen) | • Exchange transfusion | • Exchange transfusion | • Automated RCE or manual RCE over simple transfusion |
| . | NHLBI (2014)22 . | BSH (2017)7 and BJH (2018)37 . | ASH (2020)21 . |
|---|---|---|---|
| Perioperative transfusion | • In HbSS disease, goal Hb 10 g/dL prior to undergoing a surgical procedure with general anesthesia. • In HbSS patients who require surgery and have an Hb >8.5 g/dL without transfusion, are on hydroxyurea, or need high-risk surgery (eg, neurosurgery, prolonged anesthesia, cardiac bypass), consult a sickle cell expert. • In HbSC or HbSβ +-thalassemia disease that requires a surgical procedure with general anesthesia, consult a sickle cell expert. | • In HbSS disease, goal Hb 10 g/dL prior to undergoing a surgical procedure with general anesthesia for low- or moderate-risk surgery. • In HbSS disease, full exchange transfusion, with a target HbS of <30%, for high-risk surgery (major neurosurgery, cardiothoracic) and for those with a high risk of perioperative complications (eg, severe organ damage or a history of complications). • In HbSC disease, give preoperative transfusion prior to moderate- and high-risk surgery. • All other patients undergoing surgery should be individually assessed. • Consider simple transfusion for patients with Hb <9 g/dL. • If Hb >9 g/dL and exchange transfusion would delay the surgery, it may be appropriate to proceed with surgery but to plan a postoperative transfusion if needed. | • For all SCD, recommend preoperative transfusion over no preoperative transfusion in patients undergoing surgeries requiring general anesthesia and lasting more than 1 hour. |
| Symptomatic ACS with Hb 1 g/dL below baseline | • Exchange or simple transfusion | • Exchange or simple transfusion | • Automated RCE, manual RCE, or simple transfusion |
| Symptomatic severe ACS (i.e., O2 saturation <90% with supplemental oxygen) | • Exchange transfusion | • Exchange transfusion | • Automated RCE or manual RCE over simple transfusion |
BJH, British Journal of Haematology; BSH, British Society of Haematology; NHLBI, National Heart, Lung, and Blood Institute; RCE, red cell exchange.
CLINICAL CASE (continued)
Jane remained hospitalized for observation following a successful cholecystectomy. Unfortunately, she developed significant postoperative pain. On postoperative day 2, she developed a fever to 102.5 °F and a new oxygen requirement. A chest radiograph revealed a new right-lower-lobe consolidation. Her oxygen requirement rapidly increased from 2 to 5 L/min by nasal cannula. Laboratory evaluation continued to show an Hb 8.9 g/dL. Given her rapidly changing clinical status, her medical team recommended exchange transfusion.
Acute chest syndrome
ACS is the most common cause of death in persons with SCD. ACS occurs most frequently in the pediatric population but has highest mortality among adults.27 ACS is defined as a new respiratory symptom accompanied by fever and a new infiltrate on chest radiograph. The physiology is usually multifactorial and may involve infection, ventilation/perfusion mismatch due to fat embolism or the presence of sickled cells in the pulmonary microvasculature, and/or atelectasis. Although the cause of ACS is often unclear in all age groups, infectious causes are likely more common in children, whereas noninfectious causes are more common in adults.28
Transfusion can be an important component of treatment for ACS (Figure 1). The infusion of nonsickling cells has the potential to improve tissue oxygenation. In a retrospective cohort study reviewing data from the Pediatric Health Information System database, the use of transfusion was associated with a shorter hospital stay and with reduced 30-day ACS-related readmission (odds ratio, 0.60).29 Although multiple Cochrane reviews and a Cochrane meta-analysis have failed to find sufficient clinical trial evidence to support the use of transfusions for ACS, multiple guidelines and expert consensus statements support the practice.24,30,31
The decision to use transfusion therapy for ACS should be made on clinical grounds (Table 4). Transfusion is recommended for severe ACS or for patients with mild ACS and anemia beyond their baseline. Whereas children are more likely to have an infectious component, Rees and colleagues speculate that children may be more likely to recover without transfusion support than adults.5 Transfusion therapy given early in the course of ACS is associated with a shorter clinical course and decreased morbidity.29 Several case reports and cohort studies suggest that transfusions are useful in improving ACS associated with SARS-CoV-2 infection.32-35 Indeed, Strouse and colleagues found that during the novel H1N1 virus pandemic in the US, children with SCD who developed ACS required transfusion support more frequently than during seasonal influenza outbreaks.36 This likely reflects the severity of ACS associated with H1N1 and now with SARS-CoV-2.
In low- and middle-income countries where regular transfusion support may not be readily available, ACS remains a leading indication for transfusion. In a retrospective assessment of transfusion practices at a single institution in Yemen, ACS was the indication for transfusion for 11.3% of cases reviewed.37 Chamba and colleagues reported their success with manual partial exchange in managing severe ACS in Tanzania.38 In Brazil, a review of 3 years of transfusion practices in the Recipient Epidemiology and Donor Evaluation Study cohort revealed ACS as the second most common indication for transfusion following central nervous system events.39
Transfusions for ACS in the acute setting can be given as simple or exchange transfusion, depending upon the clinical context (Table 1). In patients with ACS and severe anemia, 1 or more simple transfusions can be given prior to attempting exchange transfusion. In pediatrics, given the complexity of placing catheters in sometimes small patients, patients are more likely to receive multiple simple transfusions. Exchange transfusions are more commonly given for critically ill patients or clinically worsening patients who have a high Hb level.4 Although some providers also use transfusions for the chronic management of patients with recurrent, severe ACS, the evidence to support this practice is weak.40
CLINICAL CASE (continued)
Following her complicated admission, Jane recovered well and continued to use hydroxyurea. She thrived as an outpatient and in college. She returned for a final visit to her pediatric hematologist as she prepared to transition to adult care. Jane asked about artificial blood substitutes, given her multiple alloantibodies, and the necessity of transfusion when she became pregnant in the future.
Transfusion therapy in pregnant women
Pregnancy in women with SCD is associated with an increased risk of maternal and fetal complications, including mortality, preeclampsia/eclampsia, infection, maternal thrombosis, maternal VOC/ACS, preterm labor, fetal intrauterine growth restriction, and small for gestational age neonates.41 Care coordination and frequent surveillance for complications are important parts of management, particularly where resources are limited. A recent study demonstrated an 89.1% reduction in maternal mortality and a 62.2% reduction in perinatal mortality after implementing joint inpatient and outpatient reviews by an obstetrician and hematologist, a multidisciplinary care team, protocols for the management of ACS and VOC, and close fetal/maternal surveillance in a low-resource setting.42 A systematic review and meta-analysis of the available studies in 2015 suggested that maternal and neonatal morbidity and mortality may be reduced by a prophylactic transfusion strategy; however, this was based on a small number of studies.43 A retrospective review of 46 pregnancies in 18 women with SCD suggested that early prophylactic RBC exchange may have beneficial effects on reducing maternal morbidity and improving neonatal gestational weight (>50th percentile) with low rates of alloimmunization (5.6%).44 Nonetheless, there is insufficient evidence at this time to recommend routine prophylactic simple or exchange RBC transfusion and practice varies widely. The ASH guidelines suggest that prophylactic transfusion be considered for women with a history of severe SCD-related complications prior to pregnancy (or during a prior pregnancy) or those with additional high-risk pregnancy features.25 The guidelines also suggest initiating regular transfusion if SCD-related complications develop.25 The TAPS-2 study investigating the utilization of serial prophylactic exchange transfusion in pregnant women with SCD is currently ongoing and will hopefully provide much-needed answers in this area.45
Complications of transfusion
Alloimmunization occurs when antibodies against donor RBC antigens develop, resulting in acute and delayed hemolytic transfusion reactions.2 Persons with SCD develop alloimmunization following blood transfusion at a higher rate than persons without SCD. The causes are multifactorial but include antigenic differences between persons with SCD and blood donors.25,46 In addition, persons with SCD often require multiple transfusions throughout a lifetime, increasing their exposure to various donors.9 To decrease both the rate of alloimmunization and the risk of subsequent delayed hemolytic transfusion reactions, persons with SCD must be transfused with appropriately matched products. Multiple guidelines exist regarding the utilization of RBC transfusion in this population.8,25,26 At a minimum, persons with SCD should receive Rh- (D, C/c, and E/e) and K-matched products due to the immunogenicity of these antigens.25 It should be noted that conventional serologic phenotyping may fail to correctly classify individuals with partial antigens. Thus, genotyping, particularly for the identification of Rh system variants and GATA1 mutations, is suggested in some guidelines.9,25 Unfortunately, despite matching for Rh and K, some patients will still form alloantibodies. This occurrence was demonstrated in approximately 30% of chronically transfused children with SCD.47 When this happens, the practice at our institution is to match for additional antigens (Duffy, Kidd, S/s) in an effort to prevent further alloantibody formation. The appropriate selection of RBCs for transfusion will reduce the likelihood of forming alloantibodies, which can limit the effectiveness and availability of future transfusions.
On rare occasions, hyperhemolysis syndrome can occur due to alloimmunization. It can also occur in persons without a history of alloimmunization.2,9 Hyperhemolysis syndrome can be potentially lethal because both the patient's native RBCs and transfused RBCs are simultaneously destroyed, leading to severe anemia.2,9 Hyperhemolysis syndrome is characterized by Hb below baseline after transfusion with elevated markers of hemolysis.48 Transfusion is avoided in patients with hyperhemolysis syndrome unless absolutely necessary because additional transfusion may exacerbate hemolysis and worsen anemia, potentially resulting in death.2,9 Other transfusion-related complications include allergic reactions, transfusion-transmitted infections, and febrile nonhemolytic transfusion reactions.
For individuals receiving chronic transfusion, iron overload is a common complication. It is often seen in individuals receiving chronic simple transfusion. The approximate net iron load for patients with SCD receiving 10 to 15 mL/kg of RBC every 4 weeks is 0.25 to 0.42 mg/kg/d.49 To reduce the iron load, partial manual exchange, or phlebotomy of whole blood before transfusion, may be performed. Partial manual exchange reduces the net iron load by 15% to 20% when compared to simple transfusion.49 Exchange transfusion can reduce the net iron by approximately 85% when compared to simple transfusion.49
Despite exchange transfusion significantly reducing the net iron load, monitoring for iron overload with serum ferritin and/or liver iron content (LIC) remains crucial. A retrospective study by Fasano and colleagues observed that SCD patients receiving exchange transfusion had elevated serum ferritin levels and LIC.49 On stable iron chelation therapy, these patients had stable to decreased serum ferritin levels and LIC that were significantly lower than SCD patients receiving simple transfusion with iron chelation therapy.49
Hemoglobin-based oxygen carriers
Transfusion therapy may not be an option for all persons with SCD. This may be due to the formation of single or multiple alloantibodies that limit the availability of compatible RBCs, the development of hyperhemolysis, or patient refusal. Over 20 years ago, a hemoglobin-based oxygen carrier (HBOC) was evaluated and demonstrated improved exercise tolerance in persons with SCD not in crisis.50 To date, no HBOC has received US Food and Drug Administration approval. Associated adverse events include hypertension, cardiac arrhythmias, myocardial infarction, renal damage, and mortality.51 Currently, HBOC-201 (Hemopure, HbO2 Therapeutics, Souderton, PA), a glutaraldehyde-polymerized bovine Hb, is only available in the US through clinical trial or expanded access.52 In recent years, case reports have described the successful use of HBOC-201 in the settings of hyperhemolysis and alloimmunization as well as for Jehovah's Witnesses, though there were reports of hypertension, elevated liver enzymes, and methemoglobinemia.52-54 While HBOCs can help to avoid or replace transfusion, without further studies of safety and efficacy and US Food and Drug Administration approval these agents will have limited availability.
Conclusion
SCD manifests with a variety of clinical signs and symptoms, many of which may be alleviated by the transfusion of RBCs. While RBC transfusion is a critical part of SCD management, transfusion therapy can have significant consequences. It is vital to carefully weigh the indications for transfusion prior to transfusing any person with SCD. Several guidelines are available to assist the clinical team in decision-making in the settings of stroke, ACS, and pregnancy and in the perioperative setting. Even so, many of these guidelines note that evidence remains limited, and additional studies are ongoing to determine best practices.
Acknowledgments
The authors would like to thank Karen Prince for her artistic contribution to this article.
Conflict-of-interest disclosure
Hyojeong Han: no competing financial interests to declare.
Lisa Hensch: no competing financial interests to declare.
Venée N. Tubman: research funding: National Institutes of Health K23-HL148548-01A1, Novartis Pharmaceuticals, Global Blood Therapeutics; honoraria: Perkin Elmer; consultancy: Forma Therapeutics.
Off-label drug use
Hyojeong Han: The author does not discuss the off-label use of any commercial product in this presentation.
Lisa Hensch: The author does not discuss the off-label use of any commercial product in this presentation.
Venée N. Tubman: The author does not discuss the off-label use of any commercial product in this presentation.