Abstract
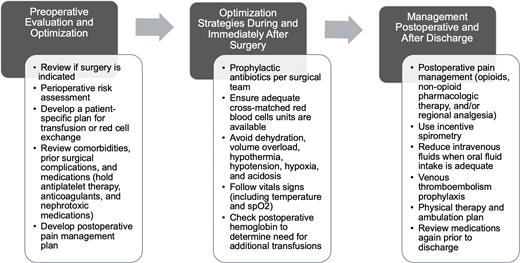
Individuals with sickle cell disease (SCD) are likely to be referred for surgery at some point in their lifetime due to a high incidence of musculoskeletal and intrabdominal complications such as avascular necrosis and gallbladder disease. Preoperative optimization is a multidisciplinary process that involves a hematologist with SCD expertise, an anesthesiologist, and the surgical team. The type and risk classification of the surgery, disease severity, medications, baseline hemoglobin, transfusion history, and history of prior surgical complications are often documented. Clinicians should consider perioperative risk assessment that includes determining the patient's functional status and cardiovascular risk and screening for obstructive sleep apnea. Many patients will require preoperative transfusion to reduce the risk of postoperative complications such as acute chest syndrome and vaso-occlusive pain crises. The hematologist should consider the patient's preoperative transfusion requirements and ensure that the surgical team has an appropriate plan for postoperative observation and management. This often includes follow-up laboratory studies, a postoperative pain management plan, and venous thromboembolism prophylaxis. The transfusion plan should be patient-specific and take into account the SCD genotype, baseline hemoglobin, disease severity, risk classification of the surgery, and history of prior surgical complications. In the intraoperative and postoperative period, dehydration, hypothermia, hypotension, hypoxia, and acidosis should be avoided, and incentive spirometry should be utilized to minimize complications such as acute chest syndrome. In this review we discuss preoperative, intraoperative, and postoperative strategies to optimize patients with SCD undergoing surgery.
Learning Objectives
Understand strategies for optimizing patients with sickle cell disease undergoing surgery
Review indications for preoperative transfusion for patients with sickle cell disease
Understand options for postoperative pain management and venous thromboembolism prophylaxis in patients with sickle cell disease
CLINICAL CASE
A 46-year-old African American woman with hemoglobin (Hb) sickle-beta plus thalassemia (HbSβ+) and right hip avascular necrosis (AVN) was referred to a sickle cell clinic for optimization prior to right total hip replacement.
She reported progressive bilateral hip pain that had been worse on the right for the past 10 years. She denied having a precipitating injury. The pain worsened with prolonged sitting and standing or walking short distances. She was most concerned that the hip pain made it difficult for her to play with her grandchildren. Three years earlier, magnetic resonance imaging (MRI) of the right hip had shown a small area of AVN of the femoral head. She was referred to orthopedics and was managed with conservative therapies including nonsteroidal anti-inflammatory drugs, a corticosteroid injection, and physical therapy. Her pain and mobility continued to worsen. A repeat MRI of the hips 2 years later showed bilateral AVN that was worse in the right hip than the left. Due to the failure of conservative management, orthopedics recommended a right total hip replacement.
Her medical history included sickle cell disease (SCD) retinopathy, anxiety, depression, hypersomnia, and gastroesophageal reflux. She had no history of stroke, venous thromboembolism (VTE), or chronic cardiopulmonary complications. She had contracted pneumonia 8 years prior, and her last transfusion had been 30 years earlier. Her medications included methadone, oxycodone, pantoprazole, aripiprazole, buspirone, folic acid, and dronabinol. She was not on hydroxyurea due to an intolerance. She had no prior surgeries and no allergies to medications. She lived alone but had 2 supportive adult children. She smoked 1 cigarette per day, drank alcohol occasionally, and had no illicit drug use.
On physical exam, her blood pressure was 117/78 mmHg; heart rate, 102/min; respiration rate, 18/min; temperature, 36.7 °C; pain score, 8/10; and weight, 73 kg. The musculoskeletal exam showed difficulty mounting the exam table and pain on internal and external hip rotation, with the right hip worse than the left. Her Hb level was 8.7 g/dL; hematocrit level, 34.6%; white blood cell count, 5.7 × 109/L; platelet count; 198 000; and absolute reticulocyte count, 93.3 × 109/L, with 2.68% reticulocytes. Her Hb electrophoresis showed a sickle hemoglobin [HbS] level of 67.0%; HbA2, 4.6%; HbA, 17.7%; fetal hemoglobin [HbF], 10.7%. Her complete metabolic profile, lactate dehydrogenase, ferritin, and urine microalbumin were all within normal. Coronavirus was not detected on SARS-CoV-2 polymerase chain reaction.
Introduction
SCD is one of the most common inherited disorders in the world.1 Patients with SCD experience red blood cell sickling, leading to microvascular occlusion that results in complications such as acute vaso-occlusive pain crises, acute chest syndrome, chronic organ damage, and musculoskeletal complications.2 Surgical complications are more common in patients with SCD compared to the general population due to their increased risk of postoperative acute chest syndrome, infections, vaso-occlusive pain crises, and 30-day surgical mortality of 1.1%.3,4 Failure to appropriately optimize a patient with SCD perioperatively can lead to complications such as acute chest syndrome, which is associated with an increased risk of death.5,6 With appropriate planning, management, and postoperative monitoring, health care providers can increase the likelihood of optimal surgical outcomes.
Determine if the surgery is really necessary
Given the high risk of both surgical and postoperative complications in patients with SCD, it is imperative to first determine whether conservative management strategies have truly failed. Consider the risks associated with surgery vs continuing with conservative management, including referral to a specialist center offering less invasive options. Ascertain a patient's personal motivations for and expected outcomes of having surgery to determine whether surgery will allow them to achieve their personal goals. This process should be a shared decision between the patient and health care providers.
Preoperative management
Once the team has planned to proceed with surgery, the next step is to evaluate the patient's risk of perioperative complications. This is typically performed by an anesthesiologist and a hematologist with expertise in SCD either in separate or multidisciplinary outpatient visits or by virtual meeting. Consider the surgical indication and the type of surgical procedure the patient is undergoing and any special considerations (Table 1). For children, ensure they are up to date on their SCD-specific health screening, which includes transcranial Doppler to assess their stroke risk. Document the risk of the surgery; SCD severity based on their genotype; complications such as stroke, renal disease, or pulmonary hypertension; non-SCD comorbidities; recent hospitalizations; recent infections; baseline Hb; transfusion history with a history of transfusion reactions and ease of crossmatch; and prior surgical complications.7,8 The hematologist should consider transfusion requirements and target sickle Hb percent (%HbS) based on the patient's genotype, phenotype, and Hb. Medications must be reviewed to avoid drug-drug interactions and nephrotoxic medications in the setting of perioperative fluid shifts. The perioperative team should consider an appropriate acuity of postoperative monitoring, including laboratory testing, a pain management plan, and VTE prophylaxis.
Common indications for surgery in sickle cell disease and considerations
| Surgical indication . | Surgery . | Surgical considerations . |
|---|---|---|
| Severe avascular necrosis | Total hip replacement27,28 | - High risk of periprosthetic and wound infection and respiratory complications - Monitor temperature, fluid balance, and Hb - Postoperative prophylactic anticoagulation for a minimum of 10-14 days and up to 35 days; LMWH is recommended - Early mobilization - Chest physiotherapy with incentive spirometry |
| Tonsillar hypertrophy, pediatric OSA, and/or recurrent tonsillitis | ENT surgery such as tonsillectomy and adenoidectomy14,29 | - At increased risk of nocturnal hypoxia pre- and postoperatively - Monitor for dehydration and postoperative oral fluid intake |
| Cholelithiasis | Cholecystectomy30 | - Use least invasive technique (laparoscopic) - Monitor for pulmonary complications (atelectasis, acute chest syndrome) and vaso-occlusive crisis of the liver |
| Splenic sequestration | Splenectomy31,32 | - Use least invasive technique (laparoscopic) - At risk for postsplenectomy infection; immunize with pneumococcal, meningococcal, Haemophilus influenza at least 10-14 days before surgery or postoperatively if emergency surgery is required - Consider prophylactic anticoagulation to prevent postsplenectomy portal vein system thrombosis |
| Priapism | Surgical shunt or penile prosthesis33 | - At risk for postoperative erectile dysfunction, penile gangrene, and perineal abscess |
| Pregnancy complications (eg, preeclampsia) | Caesarian section26,34 | - Hydrate and maintain spO2 > 94% - Consider transfusion to Hb 10 g/dL - Monitor fluid balance to avoid volume overload - Postpartum prophylactic anticoagulation for both vaginal and Caesarean deliveries for 6 weeks starting 6-12 hours after all delivery (no sooner than 4 hours after epidural catheter removal). LMWH and warfarin are not contraindicated with breastfeeding. |
| Moyamoya disease | Cerebral revascularization35 | - At risk for reduced cerebral blood flow due to general anesthesia - Aggressive fluid hydration prior to surgery - Utilize intraoperative EEG |
| Valvular disease | Cardiac surgery36 | - At risk for hemorrhage, stroke, renal failure, and acute chest syndrome - For valve replacement, at risk of hemolysis, thrombosis, and infection - Use incentive spirometry, anticoagulation, and prophylactic antibiotics - Maintain normothermia to minimize vasoconstriction and sickling |
| Surgical indication . | Surgery . | Surgical considerations . |
|---|---|---|
| Severe avascular necrosis | Total hip replacement27,28 | - High risk of periprosthetic and wound infection and respiratory complications - Monitor temperature, fluid balance, and Hb - Postoperative prophylactic anticoagulation for a minimum of 10-14 days and up to 35 days; LMWH is recommended - Early mobilization - Chest physiotherapy with incentive spirometry |
| Tonsillar hypertrophy, pediatric OSA, and/or recurrent tonsillitis | ENT surgery such as tonsillectomy and adenoidectomy14,29 | - At increased risk of nocturnal hypoxia pre- and postoperatively - Monitor for dehydration and postoperative oral fluid intake |
| Cholelithiasis | Cholecystectomy30 | - Use least invasive technique (laparoscopic) - Monitor for pulmonary complications (atelectasis, acute chest syndrome) and vaso-occlusive crisis of the liver |
| Splenic sequestration | Splenectomy31,32 | - Use least invasive technique (laparoscopic) - At risk for postsplenectomy infection; immunize with pneumococcal, meningococcal, Haemophilus influenza at least 10-14 days before surgery or postoperatively if emergency surgery is required - Consider prophylactic anticoagulation to prevent postsplenectomy portal vein system thrombosis |
| Priapism | Surgical shunt or penile prosthesis33 | - At risk for postoperative erectile dysfunction, penile gangrene, and perineal abscess |
| Pregnancy complications (eg, preeclampsia) | Caesarian section26,34 | - Hydrate and maintain spO2 > 94% - Consider transfusion to Hb 10 g/dL - Monitor fluid balance to avoid volume overload - Postpartum prophylactic anticoagulation for both vaginal and Caesarean deliveries for 6 weeks starting 6-12 hours after all delivery (no sooner than 4 hours after epidural catheter removal). LMWH and warfarin are not contraindicated with breastfeeding. |
| Moyamoya disease | Cerebral revascularization35 | - At risk for reduced cerebral blood flow due to general anesthesia - Aggressive fluid hydration prior to surgery - Utilize intraoperative EEG |
| Valvular disease | Cardiac surgery36 | - At risk for hemorrhage, stroke, renal failure, and acute chest syndrome - For valve replacement, at risk of hemolysis, thrombosis, and infection - Use incentive spirometry, anticoagulation, and prophylactic antibiotics - Maintain normothermia to minimize vasoconstriction and sickling |
EEG, electroencephalogram; ENT, ear, nose, and throat; spO2, oxygen saturation.
Preoperative risk assessment
The anesthesiologist typically assesses the patient's perioperative risk and fitness for surgery and plans anesthesia accordingly. Surgeries are stratified into risk categories based on their potential for intraoperative blood loss and postoperative complications (ie, low, moderate, or high risk; Table 2). The patient's history of strokes, acute chest syndrome, obstructive sleep apnea (OSA), adverse reactions to sedation, or recurrent VTE is documented since these increase the patient's risk of perioperative complications.
Surgical risk classification
| Low risk . | Moderate risk . | High risk . |
|---|---|---|
| Dental extractions | Head and neck surgery | Cardiac surgery (eg, valve replacement) |
| Ophthalmologic procedures (ie, laser surgery, cataract surgery) | Orthopedic surgery (eg, total hip replacement) | Intrathoracic surgery |
| Hernia repair | Urologic surgery | Brain surgery |
| Dilation and curettage | Cholecystectomy | Transplant surgery (heart, lung, liver, kidney) |
| Wound debridement | Splenectomy | Major vascular surgery (eg, aorta repair) |
| Endoscopy | Hysterectomy | Major spine surgery |
| Superficial tissue biopsy (eg, breast biopsy) | Uterine ablation | Surgeries requiring prolonged general anesthesia >4 hours (eg, Whipple procedure) |
| Caesarian section | ||
| Appendectomy |
| Low risk . | Moderate risk . | High risk . |
|---|---|---|
| Dental extractions | Head and neck surgery | Cardiac surgery (eg, valve replacement) |
| Ophthalmologic procedures (ie, laser surgery, cataract surgery) | Orthopedic surgery (eg, total hip replacement) | Intrathoracic surgery |
| Hernia repair | Urologic surgery | Brain surgery |
| Dilation and curettage | Cholecystectomy | Transplant surgery (heart, lung, liver, kidney) |
| Wound debridement | Splenectomy | Major vascular surgery (eg, aorta repair) |
| Endoscopy | Hysterectomy | Major spine surgery |
| Superficial tissue biopsy (eg, breast biopsy) | Uterine ablation | Surgeries requiring prolonged general anesthesia >4 hours (eg, Whipple procedure) |
| Caesarian section | ||
| Appendectomy |
Functional capacity is often measured by the ability to perform metabolic equivalent tasks.9 Patients unable to perform ≥4 metabolic equivalent tasks (ie, climbing a flight of stairs) have an increased risk of cardiac events.9,10 Consider OSA screening since the condition increases a patient's risk of perioperative hypoxemia.11,12 The risk of cardiovascular events is often assessed using validated models such as the revised cardiac risk index. Patients at high risk for cardiac events and with a known history of cardiopulmonary disease such as pulmonary hypertension, cardiac symptoms, or poor functional status should consider additional testing with echocardiogram, stress testing, and/or a cardiology consultation.10
Preoperative transfusion
Preoperative optimization for patients with SCD often includes simple transfusion or red cell exchange (RCE). The primary goal of preoperative transfusion is to reduce the risk of postoperative complications by increasing the Hb and reducing the %HbS.13 Patients with SCD are at increased risk of postoperative morbidity primarily related to acute chest syndrome and pain crises and have a higher risk of mortality compared to the general population. The evidence on preoperative transfusion in both pediatric and adult populations shows variable outcomes in preventing adverse outcomes and mortality.13,14
The Transfusion Alternatives Preoperatively in Sickle Cell Disease (TAPS) study, which was a multicenter randomized controlled trial (RCT) comparing no transfusion with transfusion within 10 days of low- or moderate-risk surgery for patients with genotype hemoglobin SS disease (HbSS) or sickle-beta zero thalassemia (HbSβ0), showed that patients who received preoperative transfusion had a lower risk of postoperative acute chest syndrome and other clinically important complications (15% vs 39%; P = .023).15 Despite this, there was no difference in postoperative pain crisis, hospital length of stay, or readmission rates between patients who received preoperative transfusion compared with no transfusion.13,15 A multicenter RCT comparing preoperative conservative transfusion (increasing Hb to 10 g/dL) to aggressive transfusion (using RCE to decrease %HbS to <30%) found no significant difference in the frequency of serious complications.5 Ten percent of patients in each group developed acute chest syndrome.5 Based on available evidence, some experts have concluded that the benefit of preoperative transfusion is mostly related to increasing Hb rather than reducing %HbS.13 Although the current evidence supporting preoperative transfusion is low quality, the benefits outweigh the harms; therefore, preoperative transfusion is still recommended.13
There is a lack of consensus on the best practices for preoperative and peripartum transfusions. High-quality data are needed in the era of hydroxyurea and other new disease-modifying therapies. We advise that clinicians follow national and local guidelines. According to the American Society of Hematology transfusion guidelines, in some situations RCE may reduce the risk of acute chest syndrome and pain crisis in patients with genotype HbSS/HbSβ0, Hb <9 g/dL, or a severe phenotype (characterized as having a history of stroke, recurrent acute chest syndrome, or prior severe postoperative complications) or any person with SCD undergoing high-risk surgery. Patients with a severe phenotype are most likely to benefit from achieving a post-RCE goal of %HbS <30%. For patients with Hb <9 g/dL without a severe phenotype undergoing moderate-risk surgery, simple transfusion is recommended with a posttransfusion goal of a Hb level no greater than 11 g/dL in order to avoid hyperviscosity. For patients with Hb >9 g/dL undergoing moderate-risk surgery, RCE is recommended. For patients with Hb >9g/dL without a severe phenotype undergoing low-risk surgery, consider proceeding without transfusion.13 Patients undergoing emergency surgery may receive simple transfusion to increase Hb to 10 g/dL, if indicated. Sometimes, preoperative transfusion may not be acceptable due to the potential for delaying a life-saving surgery; therefore, intraoperative or postoperative transfusion may be considered.13 See the summary of transfusion recommendations in Table 3.
Transfusion recommendations based on sickle cell genotype, hemoglobin, and surgical risk classification
| Sickle cell genotype . | Hemoglobin (g/dL) . | Surgical risk . | Transfusion recommendation . |
|---|---|---|---|
| HbSS or HbSβ0- thalassemia | <9 | Low or moderate | Simple transfusion, partial exchange, or RCE |
| HbSS or HbSβ0- thalassemia | >9 | Low or moderate | Partial exchange or RCE |
| HbSC, HbSβ+-thalassemia, and HbSS on hydroxyurea and elevated HbF without severe phenotype* | >9 | Low | No transfusion |
| HbSC or HbSβ+- thalassemia | >9 | Moderate | Partial exchange or RCE |
| All genotypes | — | High | RCE |
| Sickle cell genotype . | Hemoglobin (g/dL) . | Surgical risk . | Transfusion recommendation . |
|---|---|---|---|
| HbSS or HbSβ0- thalassemia | <9 | Low or moderate | Simple transfusion, partial exchange, or RCE |
| HbSS or HbSβ0- thalassemia | >9 | Low or moderate | Partial exchange or RCE |
| HbSC, HbSβ+-thalassemia, and HbSS on hydroxyurea and elevated HbF without severe phenotype* | >9 | Low | No transfusion |
| HbSC or HbSβ+- thalassemia | >9 | Moderate | Partial exchange or RCE |
| All genotypes | — | High | RCE |
Severe phenotype is defined as having a history of stroke, recurrent acute chest syndrome, or prior severe surgical complications.
HbSC, hemoglobin SC disease.
Alloimmunization
The incidence of alloimmunization in SCD ranges from 7% to 58% depending on age, number of previous transfusions, and use of red cell phenotypic matching.16,17 The TAPS study noted no difference in alloimmunization between patients receiving preoperative transfusion compared to no transfusion likely due to the use of extended red cell phenotypic matching, and participants had previously received fewer transfusions compared to other studies.15 When comparing aggressive transfusion to conservative transfusion, an RCT showed an increased risk of alloimmunization with aggressive transfusion; therefore, many centers prefer simple transfusion over RCE when appropriate.5 Patients with a history of multiple alloantibodies, delayed hemolytic transfusion reaction (DHTR), and/or hyperhemolysis have an increased risk of adverse outcomes related to transfusion; therefore, careful consideration should be given prior to transfusion. The risk of transfusion-related complications should be discussed and documented, and in some situations, transfusion is not possible. In the event an emergent transfusion is required, consider having crossmatched blood available on-site even if there is no plan for transfusion. The blood should be antigen-negative for any positive antibodies and previous antibodies even if those antibodies are no longer detectable in order to minimize the risk of DHTR. For life-threatening anemia, consider immunosuppressive therapy if transfusion is absolutely required.8,13,18 In patients with religious objections to transfusion or if transfusion is not possible due to severe alloimmunization/previous DHTR, it is important to optimize the Hb in advance with medications such as hydroxyurea, voxelotor, and erythroid-stimulating agents.
Pain management plan
The patient's current pain regimen should be reviewed, and a postoperative pain management plan should be developed, often similar to a patient's usual inpatient acute pain plan and including patient-controlled analgesia (PCA).7 The decision to include continuous basal opioid infusion vs on-demand dosing only should be patient-specific and determined by the patient's level of postoperative pain and opioid tolerance.19 Referral to the local acute pain team is advised to ensure appropriate opiate dosing and nonopiate adjuncts, such as a short course of nonsteroidal anti-inflammatory drugs (5-7 days if no renal risk), intravenous (IV) ketamine or lidocaine, regional blocks, and acetaminophen.19
Intraoperative period and immediately after surgery
The most important factor to consider intraoperatively is to avoid imbalances in volume status, temperature, acid-base balance, blood pressure, and oxygenation since derangements increase red blood cell sickling, which can result in acute organ injury. It can also manifest as a vaso-occlusive pain crisis, as acute chest syndrome, as an acute kidney injury, or even as an ischemic stroke. Practical strategies to maintain euvolemia include avoiding prolonged fasting prior to surgery without IV fluids, monitoring fluid intake and output, and decreasing IV fluids as soon as patients are able to maintain adequate oral fluid intake. Avoid extremely cold or hot ambient temperatures preoperatively, in the operating room, and in the recovery space while using fluid and convective warming technology aggressively.
Postoperative period
All patients with SCD should use an incentive spirometer postoperatively since this has been shown to reduce the incidence of atelectasis and acute chest syndrome in hospitalized patients with SCD.20,21 Monitor for postoperative infection, and if a patient's temperature is ≥38 °C, investigate for a source of the fever with blood and urine cultures, wound inspection, and chest x-ray, as indicated.8 Minimize the risk of hypoxia with the judicious use of analgesics to avoid respiratory depression. If oxygen saturation falls by ≥2% below the patient's baseline or is ≤94%, provide supplemental oxygen and evaluate the patient with consideration for postoperative complications such as acute chest syndrome and pulmonary embolism. The evaluation often includes physical examination, arterial blood gas, and chest imaging. Consider checking the metabolic profile after surgery to assess for acute kidney injury and electrolyte derangements.
Anticoagulation management
SCD causes hypercoagulability due to multiple alterations in hemostasis, including increased platelet activation, activation of the clotting cascade, impaired fibrinolysis, and intravascular hemolysis.22,23 The incidence of VTE in individuals with SCD is as high as 12% before the age of 40.24 Hospitalized adults with SCD should receive VTE prophylaxis if there is no contraindication since VTE in SCD is associated with increased mortality.25 There is insufficient evidence on postoperative VTE prophylaxis in children. For both pediatric and adult populations, we suggest prescribing VTE prophylaxis based on national or local guidelines. Most inpatient teams use low-molecular-weight heparin (LMWH) or low-dose unfractionated heparin. Patients undergoing surgeries that require prolonged immobilization, such as hip surgery, require extended VTE prophylaxis (Table 1). Perioperative teams should consider the use of intermittent pneumatic compression during the hospital stay and encourage early mobilization. LMWH or warfarin is recommended for postpartum VTE prophylaxis in all individuals with SCD who plan to breastfeed since DOACs are contraindicated (Table 1).26
CLINICAL CASE (Continued)
Our patient's perioperative risk scores were documented by the anesthesiologist as low risk, with physical status consistent with mild systemic disease without substantial limitations and a low risk of having OSA. She received RCE 4 days before surgery. Post-RCE Hb improved to 11.4 g/dL and HbS was 24.8%. She underwent total right hip replacement under spinal anesthesia without complications. Her postoperative Hb was 9.6 g/dL.
An anesthesia acute pain service managed her postoperative pain. A continuous infusion of ropivicane via a catheter inserted under ultrasound guidance into the adductor canal was supplemented by IV hydromorphone PCA and a low-dose ketamine infusion. Her home methadone was started once she was tolerating a diet, and the PCA and ketamine were discontinued on postoperative day (POD) 1. Cyclobenzaprine and ketorolac were started once renal function was determined to be stable.
For postoperative prophylaxis for deep vein thrombosis, she received 30 mg of LMWH twice a day for 30 days, which started on POD 1. She was discharged on POD 2 with outpatient rehabilitation 3 days a week. On follow-up in the hematology clinic, she reported significant improvements in mobility, range of motion, and pain. She no longer required the use of an assist device to ambulate and was able to meet her goal of being able to play with her grandchildren.
Conclusion
Preoperative optimization is an essential part of care for individuals with SCD undergoing surgery. People with SCD are more likely to have surgical complications compared to the general population, so it is imperative that consultation with an SCD specialist be included in the optimization plan. Appropriate optimization and management prior to, during, and after surgery can reduce the risk of adverse outcomes in individuals with SCD. More research is needed to improve perioperative management guidelines for SCD.
Acknowledgments
Charity I. Oyedeji recognizes support from the American Society of Hematology Research Training Award for Fellows and the Duke Center for Research to Advance Healthcare Equity, which is supported by the National Institute on Minority Health and Health Disparities under award number U54MD012530.
Conflict-of-interest disclosure
Charity I. Oyedeji: no competing financial interests to declare.
Ian J. Welsby: no competing financial interests to declare.
Off-label drug use
Charity I. Oyedeji: nothing to disclose.
Ian J. Welsby: nothing to disclose.