Abstract
Case 1: A 23-year-old female third-year medical student who has no medical history seeks treatment for abdominal distention. She takes an estrogen-containing birth control pill and does not smoke or consume alcohol. Family history is unremarkable. Physical examination is significant for abdominal distention, and an abdominal fluid wave is detected. Complete blood count is normal. Imaging confirms occlusive thrombosis of the main portal vein. On endoscopy, grade 1 to 2 esophageal varices are noted and banded. Unfractionated heparin is begun. Subsequent workup reveals a homozygous factor V Leiden mutation. Long-term anticoagulation is planned, and she asks if warfarin can be avoided given her hectic ward rotations, erratic diet, and need for monitoring. Case 2: A 35-year-old woman who has no medical history seeks treatment for progressively worsening posterior headaches for 1 week. Magnetic resonance imaging of the brain shows dural sinus thrombosis with associated small areas of petechial cerebral hemorrhage. She is started on a continuous unfractionated heparin infusion and admitted to the hospital for further observation. Her grandmother is on warfarin for atrial fibrillation, and the patient would prefer to avoid warfarin because she does not think she can comply with the frequent monitoring that will be required. She inquires about other oral anticoagulant options for her condition.
Learning Objectives
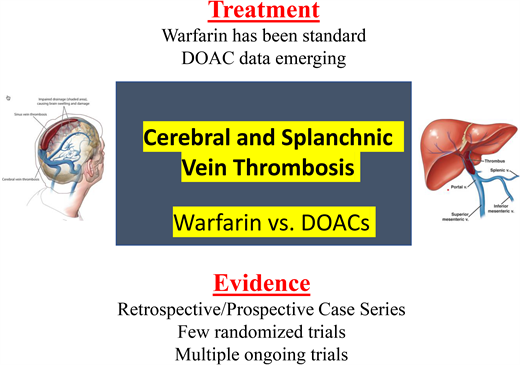
Discuss the relative risks, benefits, and unique characteristics of the DOACs vs warfarin in patients with thrombosis in the splanchnic or cerebral veins
Choose an oral anticoagulant in a patient with thrombosis in the splanchnic or cerebral veins
Introduction
When not otherwise contraindicated, most experts and societal guidelines recommend early anticoagulation in patients with splanchnic or cerebral vein thrombosis (CVT).1-6 However, many of these recommendations are based primarily on small case series, as only a few randomized trials exist.4-8 Whether anticoagulation is recommended for a limited time period or indefinitely depends on whether the clot was provoked and if the provocation was transient or will be longstanding.1-6 Most of the studies referenced in this article do not clearly identify whether outcomes differed between provoked and unprovoked splanchnic or CVT. Most experts recommend 3 to 12 months of anticoagulation for a provoked splanchnic or CVT. Long-term anticoagulation is often recommended for persistent (severe thrombophilia, cancer, myeloproliferative disorder, etc) risk factors, recurrent thrombosis, or hepatic vein thrombosis.9 Historically, warfarin has been the only oral anticoagulant available for use in patients with chronic splanchnic or CVT.
Since 2010, 4 direct oral anticoagulants (DOACs) have been approved by the US Food and Drug Administration for the treatment of venous thromboembolism (VTE) Based on large, randomized trials, both the CHEST and ASH guidelines recommend DOACs as the treatment of choice for oral anticoagulation in patients with deep vein thrombosis or pulmonary embolism.9-11 Patients with atypical site thrombosis were generally excluded from these trials, and therefore recommendations concerning the use of DOACs in splanchnic vein thrombosis (SVT) or CVT remain challenging. The DOACs have several advantages over warfarin, including fewer drug-drug interactions, fixed dosing, shorter half-life, lack of need for monitoring, quick onset and offset, and less major bleeding in large randomized clinical trials. In the past several years, small case series and a few randomized trials have been published reporting on the efficacy and bleeding risk of the DOACs in splanchnic and CVT.7,8,12 Table 1 summarizes our interpretation of this literature.
DOAC use in SVT and CVT
| • Evidence is limited but growing. Few randomized trials have been completed. |
| • Most retrospective and prospective data show the DOACs are at least as effective as VKAs, and bleeding risk is not higher. |
| • Multiple trials are currently accruing patients. |
| • Despite being off label, in a recent survey, DOACs were used in 28% of low bleeding risk patients. |
| • For patients with SVT, DOACs are contraindicated in Child-Pugh class C liver disease and for rivaroxaban in class B and C liver disease. |
| • For patients with CVT, consider interactions with antiepileptic drugs, and if concomitant intracranial hemorrhage, consider initial use of a short-acting anticoagulant. |
| • Evidence is limited but growing. Few randomized trials have been completed. |
| • Most retrospective and prospective data show the DOACs are at least as effective as VKAs, and bleeding risk is not higher. |
| • Multiple trials are currently accruing patients. |
| • Despite being off label, in a recent survey, DOACs were used in 28% of low bleeding risk patients. |
| • For patients with SVT, DOACs are contraindicated in Child-Pugh class C liver disease and for rivaroxaban in class B and C liver disease. |
| • For patients with CVT, consider interactions with antiepileptic drugs, and if concomitant intracranial hemorrhage, consider initial use of a short-acting anticoagulant. |
CASE 1
A 23-year-old female third-year medical student who has no medical history seeks treatment for abdominal distention. She takes an estrogen-containing birth control pill and does not smoke or consume alcohol. Family history is unremarkable. Physical examination is significant for abdominal distention, and an abdominal fluid wave is detected. Complete blood count is normal. Imaging confirms occlusive thrombosis of the main portal vein. On endoscopy, grade 1 to 2 esophageal varices are noted and banded. Unfractionated heparin is begun. Subsequent workup reveals a homozygous factor V Leiden mutation. Long-term anticoagulation is planned, and she asks if warfarin can be avoided given her hectic ward rotations, erratic diet, and need for monitoring.
Only a single randomized clinical trial comparing a DOAC to warfarin has been reported in patients with SVT.12 Hanafy et al12 studied 80 patients with acute nonmalignant portal vein thrombosis (PVT) with hepatitis C–related compensated liver disease. After initial treatment with enoxaparin at therapeutic doses for 3 days, patients at 2 Egyptian centers were randomized between warfarin with a target international normalized ratio (INR) of 2 to 2.5 and rivaroxaban 10 mg bid. Recanalization of the portal vein was found in 100% of patients in the rivaroxaban group compared with 45% in the warfarin group (P = .001). Major gastrointestinal (GI) bleeding was not seen in the rivaroxaban group but occurred in 43% of patients in the warfarin group (P = .001).12 No deaths occurred in the rivaroxaban group compared with 36% in the warfarin group (P = .001).12
Riva and Ageno9 summarize most of the remaining evidence reporting on the use DOACs in SVT, which consists mostly of small observational trials, the majority retrospective in nature. Serrao et al13 describe a recent prospective study of 28 patients with SVT and ongoing risk factors maintained on chronic treatment with warfarin who were switched to DOACs and compared outcomes to 42 patients remaining on warfarin. There was no difference in thrombotic events between the groups. No major bleeding events occurred in either group, while minor bleeding did not occur in the DOAC group but was documented in 26% of warfarin-treated patients (P = .09).13
In the largest of the retrospective trials, Naymagon et al14 in Blood Advances reported on 93 patients with noncirrhotic portal vein treated with apixaban (n = 20), rivaroxaban (n = 65), and dabigatran (n = 8) compared with low molecular weight heparin (LMWH) (n = 70) and warfarin (n = 108).14 Seventy-three percent of patients had predisposing factors for PVT. Complete resolution of thrombosis was seen in 66% of DOAC-treated patients compared with 57% with LMWH and 31% with warfarin (hazard ratio, 2.91; 95% CI, 1.87-4.52 for DOAC vs warfarin).14 There was less major bleeding with the DOACs compared with warfarin (hazard ratio for DOACs: warfarin, 0.20; 95% CI, 0.05-0.86; P = .0307).14
A recent systematic review and meta-analysis published in Blood by Valeriani et al4 reported on 79 patients with SVT in 5 studies who were treated with DOACs. SVT was unprovoked in 25% of cases. The rates of SVT recanalization, thrombosis progression, major bleeding, and overall mortality did not significantly differ between type of anticoagulant used.4 A 2021 study by Kawata et al15 also showed no difference in clot recanalization between patients with SVT treated with LMWH/warfarin or with any of the DOACs. Local risk factors were present in 118 (76.1%) patients (secondary SVT), whereas 7 (4.5%) patients had no risk factors and 30 (19.4%) patients had only systemic or thrombophilia (primary SVT).15
Limited data exist concerning the use of DOACs in Budd-Chiari syndrome and mesenteric vein thrombosis (MVT). In a retrospective analysis, patients with Budd-Chiari syndrome treated after endovascular intervention with dabigatran (n = 36) were compared with those taking warfarin (n = 62).16 Baseline data on hypercoagulable states were available in 45 (45.9%) of 98 patients.16 At 12 months, stent patency rates (91% vs 93%), major bleeding (3.5% vs 6.5%), and the composite end point of mortality and major bleeding (4% vs 8%) did not differ between the dabigatran- and warfarin-treated groups.16 In a retrospective study of 102 patients with MVT, no difference was seen between patients treated with a DOAC or warfarin in terms of recanalization (69% vs 71%, P = .88) or major bleeding (9.1% vs 14.3%, P = .54).16 No recurrences of MVT were seen in either group.17
ADAM VTE, compared with the HOKUSAI VTE, SELECT-D, and CARAVAGGIO studies, is the only large, randomized treatment trial of DOACs in patients with cancer to include patients with SVT.18-21 Of the enrolled patients, 8% of those receiving apixaban had a SVT as the qualifying event, as opposed to 18% in the dalteparin group. In the group treated with apixaban, there was a single recurrent event (lower extremity thrombosis) and no major bleeding.18
CASE 2
A 35-year-old woman who has no medical history seeks treatment for progressively worsening posterior headaches for 1 week. Magnetic resonance imaging of the brain shows dural sinus thrombosis with associated small areas of petechial cerebral hemorrhage. She is started on a continuous unfractionated heparin infusion and admitted to the hospital for further observation. Her grandmother is taking warfarin for atrial fibrillation, and the patient would prefer to avoid warfarin because she does not think she can comply with the frequent monitoring that will be required. She inquires about other oral anticoagulant options.
Data supporting the use of DOACs in CVT are emerging. High-quality evidence is still limited, as there has been only 1 randomized controlled trial reported.22 The RE-SPECT CVT trial, published in 2019, is a multicenter, open-label study that randomized 120 patients with CVT to either dabigatran 150 mg twice daily or warfarin with a goal INR of 2 to 3 for 24 weeks. Approximately 50% of the patients in each group had identifiable provoking factors. All patients received initial treatment with parenteral heparin or LMWH (5-15 days). The primary end point of the study was new venous thromboembolism—new CVT, pulmonary embolism, limb DVT, SVT, or major bleeding.22 Major bleeding was defined according to the International Society of Thrombosis and Haemostasis (ISTH) criteria.23 Mean treatment duration was 5.1 months in the dabigatran arm and 5.3 months in the warfarin group, with a mean time in therapeutic range of 66.1% for warfarin-treated patients.22 There were no recurrent venous thromboembolic events in either treatment group, and the incidence of major bleeding was low in this study. Two patients treated with warfarin experienced major intracranial bleeding (3.3%; 95% CI, 0.4%-11.5%), 1 patient had major GI bleeding (1.7%; 95% CI, 0.0%-8.9%), and another patient experienced clinically relevant nonmajor genitourinary bleeding.22 The secondary end point of cerebral vein recanalization occurred in 33 patients (60.0%; 95% CI, 45.9%-73.0%) in the dabigatran group and 35 patients (67.3%; 95% CI, 52.9%-79.7%) in the warfarin group.18 An excellent functional outcome (modified Rankin scale 0-1 points) was seen in 91.5% and 91.4% in the warfarin and dabigatran groups, respectively.22 Based on the results of the above trial, dabigatran and warfarin appear to have a similar efficacy and safety profile in the treatment of patients with CVT after brief, initial therapy with unfractionated heparin or LMWH.
A systematic review and meta-analysis of 6 studies (5 observational and 1 randomized) examining the safety and efficacy of DOACs vs vitamin K antagonists (VKAs) was published in 2020.24 There were 412 patients in total, and 151 were treated with DOACs and 261 with VKAs.20 Provoking factors that were reported in the studies included oral contraceptive use (24.2%, n = 100/412) and pregnancy (6.3%, n = 26/412). DOAC efficacy was comparable to VKA for cerebral vein recanalization (relative risk [RR], 1.02; 95% CI, 0.89-1.16) and excellent functional outcomes as measured by a modified Rankin scale less than 2 (RR, 1.02; 95% CI, 0.93-1.13).24 There was a trend toward less major bleeding in the DOAC treatment group, but this did not reach statistical significance (RR, 0.44; 95% CI, 0.12-1.59).24 Another systematic review that included 33 studies (1 randomized controlled trial, 5 observational, 27 case series/studies) reported on patients with CVT who were treated with DOACs (n = 279) vs VKAs (n = 315).25 The most common DOAC was rivaroxaban (47%), followed by dabigatran (41%), apixaban (10%), and edoxaban (2%).25 Results showed a similar risk of death in the DOAC and VKA arms (RR, 2.12; 95% CI, 0.29-15.59).25 Rates of new intracranial hemorrhage (0.7%) and recurrent CVT (1.5%) were very low in patients treated with DOACs.25 Excellent functional outcomes were observed in 94% of patients in the DOAC arm with an RR of 1.13 (95% CI, 1.02-1.25).25
The largest prospective observational study was performed by Wasay et al26 and published in the Journal of Stroke. This study reported on patients from Saudi Arabia, Pakistan, Egypt, and United Arab Emirates.26 They included 111 patients—45 on DOACs and 66 on warfarin. The most common DOAC used was rivaroxaban (n = 36), followed by dabigatran (n = 9). The warfarin dose was adjusted to maintain an INR range of 2 to 3.26 Initiation of warfarin or a DOAC happened at a median time of 1 week from the time of CVT diagnosis, and the median duration of follow-up was 8 months (range, 6-13 months).26 Most patients had provoking factors, including pregnancy/puerperium (23.1%), systemic infections (32.4%), drugs/oral contraceptive pills (9.9%), and other medical conditions (6.3%).26 No recurrent VTE events were seen in either group. One patient in each group had major bleeding as classified by ISTH criteria. Four patients (6.1%) and 2 patients (4.4%) in the warfarin and DOAC group, respectively, had any bleeding.26 Rusin et al27 prospectively recruited 36 patients with CVT who were treated with DOACs, including dabigatran (n = 18), rivaroxaban (n = 10), and apixaban (n = 8), for a median duration of 8.5 months. Of the patients, 94.4% (n = 34) were noted to have complete or partial recanalization of the cerebral veins.23 CVT recurrence was observed in 5.6% (n = 2) after anticoagulation was discontinued.27 Major bleeding occurred in 8.3% (n = 3; 2 rivaroxaban [menorrhagia], 1 dabigatran [GI bleeding]), which was relatively high compared with other studies.27 DOACs as the upfront treatment of acute phase CVT without heparin were examined in a prospective study by Shankar Iyer et al.28 The study was small (n = 20), and critically ill patients were excluded.28 All patients were treated with rivaroxaban only, without heparin or LMWH therapy.28 Cerebral vein recanalization was seen in all patients (60% complete and 40% partial), and excellent functional outcome was noted in 95% (n = 19) of the patients.28 Patients were treated for a median of 6 months with no major bleeding noted.28
At least 5 retrospective observational studies were published between 2014 and 2019.29-33 Sample sizes were small (range n = 6-15 patients). Dabigatran was the most commonly prescribed DOAC, followed by rivaroxaban and apixaban, respectively. Treatment duration ranged from 6 to 12 months. Recurrent VTE was not observed in any of the patients reported in these retrospective studies. Cerebral vein recanalization rates ranged from 55.6% to 100%.29-33 Bleeding was minimal, with no major bleeding observed. Minor bleeding ranged from 0% to 28.6%.29-33
The aforementioned ADAM VTE trial of apixaban in patients with cancer included only a single patient with CVT.18 In a retrospective MD Anderson study of 45 patients with cancer and CVT, 33 were treated with anticoagulants (LMWH, 23 cases; warfarin, 10 cases).34 The specific recurrent rates of not anticoagulated, LMWH-treated, and warfarin-treated patients were 25.0%, 13.0%, and 10.0%, respectively, which did not reach statistical significance. The incidence of intracranial hemorrhage after CVT diagnosis was higher in the group receiving anticoagulation (30.3%; 95% CI, 16.8%-47.1%) vs no anticoagulation (25.0%; 95% CI, 7.6%-52.9%), with no significant statistical difference (P = 1.000). The choice of anticoagulant was associated with bleeding events (LMWH, 34.8%; warfarin, 80.0%; odds ratio, 7.50; 95% CI, 1.05-54.3; P = .048). No patients were treated with DOACs in this cancer trial. The authors concluded that a narrow therapeutic index of anticoagulation may exist in cancer-associated CVT.34
Despite being off label, the DOACs are being prescribed in an increasing number of patients with SVT and CVT. A 2020 cross-sectional survey of members of 3 different hemostasis and thrombosis societies explored choices of anticoagulant therapy in 4 different clinical vignettes.35 Across the 4 vignettes, great variability existed, but VKAs were the most common choice (44%-63%), followed by the DOACs (23%-27%) in low bleeding risk patients.35 In high bleeding risk scenarios, parenteral agents were the second most common choice.35
Most of the studies presented in this article have many limitations, making definitive recommendations difficult; few were randomized, sites of thrombosis differed, type of DOAC use differed, and length of therapy was heterogeneous. Future studies should be randomized, include well-defined sites of thrombosis (portal, mesenteric, hepatic, or cerebral), choose a single DOAC to compare with warfarin, and treat for a consistent length of time. Multiple trials testing DOACs in clots in unusual places are ongoing, as summarized by Riva et al.36
Current society guidelines/expert opinion
Riva and Ageno,9 in a state-of-the-art ISTH 2020 report, conclude that the current evidence suggests that DOACs can be used in select patients with unusual-site thrombosis given comparable efficacy and a trend toward lower bleeding compared with VKAs. The authors stress that caution should be taken in high-risk populations such as those with cirrhosis, varices, central nervous system infection, or trauma. In addition, they note that individualized decisions need to be considered in patients with Child-Pugh class B to C liver disease, moderate to severe renal dysfunction, luminal GI malignancy (SVT), and those taking antiseizure medication (CVT).9
In 2016, recommendations by the European Association for the Study of the Liver included LMWH followed by VKAs for nonmalignant, noncirrhotic PVT.2
The European Society for Vascular Surgery recommended LMWH or unfractionated heparin followed by either VKA or DOAC in patients with MVT.36,37
The most recent guidelines for CVT treatment from the European Stroke Organization and endorsed by the European Academy of Neurology do not recommend DOAC use in the acute phase of CVT treatment but suggest a preference for LMWH.38 These guidelines were published before the results of the RE-SPECT CVT trial and most of the prospective trial data mentioned above. With the new information, upcoming guidelines would likely include use of DOACs in CVT as secondary prophylaxis.
Ongoing trials should allow further recommendations in the near future (Table 2).
Ongoing trials evaluating DOACs in the treatment of thrombosis in unusual sites
| Title . | Identifier . | Study design . | Intervention . | Site of thrombosis . | Primary outcome . | No. of patients . | Sponsor . |
|---|---|---|---|---|---|---|---|
| The efficacy and safety of dabigatran etexilate compared with warfarin for the anticoagulation treatment of cerebral venous thrombosis: a pilot study | NCT03217448 | Phase 3 (interventional), randomized, parallel assignment, open label, single (outcomes assessor) | Dabigatran vs warfarin for 6 months | CVT | Recanalization after 6 months | 80 | Capital Medical University, Beijing, China |
| Multicenter, prospective randomized open label, blinded endpoint (PROBE) controlled trial of early anticoagulation with rivaroxaban versus standard of care in determining safety at 365 days in symptomatic cerebral venous thrombosis (SECRET) | NCT03178864 | Interventional, randomized, parallel assignment, single (outcomes assessor) | Rivaroxaban vs standard of care | CVT | Safety of rivaroxaban | 100 | University of British Columbia, Canada |
| Comparing treatment outcomes in CVT patients who were treated with warfarin and rivaroxaban in Isfahan, Iran | NCT03747081 | Interventional, randomized, parallel assignment | Rivaroxaban vs warfarin | CVT | Efficacy of rivaroxaban vs warfarin | 50 | Isfahan University of Medical Sciences, Iran |
| Rivaroxaban compared to warfarin for treatment of cerebral venous thrombosis: a randomized controlled trial | NCT04569279 | Interventional, parallel assignment, open label | Rivaroxaban vs warfarin 6 months | CVT | Change of sinus venous thrombosis severity scale | 71 | Damascus University, Syria |
| Comparison of the efficacy of rivaroxaban to coumadin (warfarin) in cerebral venous thrombosis | NCT03191305 | Interventional, nonrandomized, parallel assignment | Rivaroxaban vs coumadin | CVT | Efficacy of rivaroxaban and comparison to warfarin | 50 | Foundation University Islamabad, Pakistan |
| Treatment of portal, mesenteric, and splenic vein thrombosis with rivaroxaban. A pilot, prospective cohort study | NCT02627053 | Interventional, single group assignment, prospective, cohort study | Rivaroxaban | PVT, MVT, SVT | Safety and efficacy of rivaroxaban at 3 months | 100 | Università degli Studi dell'Insubria, Italy |
| Direct oral anticoagulants for the treatment of cerebral venous thrombosis: an international phase IV study | NCT04660747 | Observational, comparative cohort study, prospective | 3:2 ratio DOAC/VKA | CVT | Composite of major bleeding and symptomatic recurrent venous thrombosis after 6 months | 500 | Academisch Medisch Centrum—Universiteit van Amsterdam (AMC-UvA), The Netherlands |
| International registry on the use of the direct oral anticoagulants for the treatment of unusual site venous thromboembolism | NCT03778502 | Observational, patient registry, prospective, cohort study | Any DOAC | All sites | Evaluate the use of DOACs in unusual-site VTE and to assess safety and effectiveness | 100 | University of Malta, Malta |
| Title . | Identifier . | Study design . | Intervention . | Site of thrombosis . | Primary outcome . | No. of patients . | Sponsor . |
|---|---|---|---|---|---|---|---|
| The efficacy and safety of dabigatran etexilate compared with warfarin for the anticoagulation treatment of cerebral venous thrombosis: a pilot study | NCT03217448 | Phase 3 (interventional), randomized, parallel assignment, open label, single (outcomes assessor) | Dabigatran vs warfarin for 6 months | CVT | Recanalization after 6 months | 80 | Capital Medical University, Beijing, China |
| Multicenter, prospective randomized open label, blinded endpoint (PROBE) controlled trial of early anticoagulation with rivaroxaban versus standard of care in determining safety at 365 days in symptomatic cerebral venous thrombosis (SECRET) | NCT03178864 | Interventional, randomized, parallel assignment, single (outcomes assessor) | Rivaroxaban vs standard of care | CVT | Safety of rivaroxaban | 100 | University of British Columbia, Canada |
| Comparing treatment outcomes in CVT patients who were treated with warfarin and rivaroxaban in Isfahan, Iran | NCT03747081 | Interventional, randomized, parallel assignment | Rivaroxaban vs warfarin | CVT | Efficacy of rivaroxaban vs warfarin | 50 | Isfahan University of Medical Sciences, Iran |
| Rivaroxaban compared to warfarin for treatment of cerebral venous thrombosis: a randomized controlled trial | NCT04569279 | Interventional, parallel assignment, open label | Rivaroxaban vs warfarin 6 months | CVT | Change of sinus venous thrombosis severity scale | 71 | Damascus University, Syria |
| Comparison of the efficacy of rivaroxaban to coumadin (warfarin) in cerebral venous thrombosis | NCT03191305 | Interventional, nonrandomized, parallel assignment | Rivaroxaban vs coumadin | CVT | Efficacy of rivaroxaban and comparison to warfarin | 50 | Foundation University Islamabad, Pakistan |
| Treatment of portal, mesenteric, and splenic vein thrombosis with rivaroxaban. A pilot, prospective cohort study | NCT02627053 | Interventional, single group assignment, prospective, cohort study | Rivaroxaban | PVT, MVT, SVT | Safety and efficacy of rivaroxaban at 3 months | 100 | Università degli Studi dell'Insubria, Italy |
| Direct oral anticoagulants for the treatment of cerebral venous thrombosis: an international phase IV study | NCT04660747 | Observational, comparative cohort study, prospective | 3:2 ratio DOAC/VKA | CVT | Composite of major bleeding and symptomatic recurrent venous thrombosis after 6 months | 500 | Academisch Medisch Centrum—Universiteit van Amsterdam (AMC-UvA), The Netherlands |
| International registry on the use of the direct oral anticoagulants for the treatment of unusual site venous thromboembolism | NCT03778502 | Observational, patient registry, prospective, cohort study | Any DOAC | All sites | Evaluate the use of DOACs in unusual-site VTE and to assess safety and effectiveness | 100 | University of Malta, Malta |
Author recommendations
SVT: Based on the available data, we recommend use of either warfarin or a DOAC in patients with SVT. In patients with Child-Pugh B liver disease, rivaroxaban should be avoided, and in Child-Pugh C liver disease, all of the DOACs are contraindicated. We recommend treatment for incidentally detected SVT, unless it is confirmed to be chronic compared with prior scans. In patients with advanced liver disease in whom the DOACs are contraindicated and warfarin would be difficult, given the elevated baseline prothrombin time, we recommend use of LMWH and consideration of dose reduction based on the degree of thrombocytopenia and coagulopathy. In SVT, we recommend treatment of at least 3 to 6 months. Extended-duration anticoagulation should be considered in patients with ongoing risk factors for thrombosis.
CVT: Based on the available data, we recommend use of either warfarin or dabigatran for treatment of an initial episode of CVT for a duration of at least 3 to 6 months. Extended-duration anticoagulation should be considered in patients with ongoing risk factors for thrombosis. In patients who cannot receive warfarin or dabigatran, use of rivaroxaban and apixaban can be considered based on prospective and retrospective studies.
Conflict-of-interest disclosure
Carol Mathew: no relevant conflicts to disclose.
Marc Zumberg: member, ABIM Hematology Board, ASH speaker reimbursement, law case review.
Off-label drug use
Carol Mathew: DOAC use in splanchnic and cerebral vein thrombosis is discussed.
Marc Zumberg: DOAC use in splanchnic and cerebral vein thrombosis is discussed.