Abstract
Preoperative anemia is associated with increased postoperative morbidity and mortality and with increased risk of perioperative transfusion. It is an important and modifiable risk factor for surgical patients. For high-blood-loss surgery, preoperative anemia is defined as hemoglobin <13 g/dL for both male and female patients. Preoperative anemia is common, ranging from 25% to 40% in large observational studies. The most common treatable cause of preoperative anemia is iron-deficiency anemia; the initial laboratory tests should focus on making this diagnosis. Management of iron-deficiency anemia includes iron supplementation with IV iron therapy when oral iron is ineffective or not tolerated, there is severe anemia, and there is insufficient time to surgery (<4 weeks). In other situations, erythropoiesis-stimulating agents may be considered, particularly for those patients with multiple alloantibodies or religious objections to transfusion. To facilitate the diagnosis and management of preoperative anemia, establishment of preoperative anemia-screening clinics is essential. The goals of management of preoperative anemia are to treat anemia, reduce the need for transfusion, and improve patient outcomes.
Learning Objectives
Understand the importance of preoperative anemia management
Manage preoperative anemia according to current guidelines
Identify key steps in setting up a preoperative anemia management clinic
Clinical case
A 73-year-old man presents to the orthopedic surgeon’s office for assessment for left total hip replacement. He has had significant hip pain over the past 6 months. His past medical history is significant for type 2 diabetes, hypertension, osteoarthritis, and obesity. On assessment, the surgeon, who recently attended grand rounds on patient blood management (PBM), notes that the patient’s hemoglobin is 10.3 g/dL. She wonders how this will impact her patient and whether management of the patient’s anemia will improve his outcome.
Why is preoperative anemia so important?
There has been a long tradition of accepting anemia as a relatively harmless problem that can be corrected easily with transfusion; for many, this remains the default management strategy. However, multiple studies have found an association between preoperative anemia and increased postoperative mortality and morbidity.1,2 The most recent meta-analysis from an international consensus conference on PBM demonstrated that preoperative anemia was strongly associated with increased in-hospital mortality (odds ratio [OR], 2.09; 95% confidence interval [CI], 1.48-2.95) and increased morbidity.2 In 227 425 patients undergoing major noncardiac surgery in the National Surgical Quality Improvement Program (NSQIP) database in the United States, preoperative anemia was independently associated with increased 30-day mortality (OR, 1.42; 95% CI, 1.31-1.54) after adjustment for other risk factors.3 In 39 309 patients from the European Surgical Outcomes Study of patients undergoing noncardiac and nonneurological surgery, preoperative anemia, particularly moderate to severe anemia (hemoglobin <11 g/dL), was associated with higher in-hospital mortality, longer hospital length of stay, and postoperative intensive care admission compared with those with normal preoperative hemoglobin (male patients, ≥13 g/dL; female patients, ≥12 g/dL).4 Not only has preoperative anemia been associated with worse outcomes in and of itself, it has also been associated with an increased risk of perioperative transfusion,1,5,6 with the inherent risks of transfusion.7
Unfortunately, it does not appear that transfusion compensates for the poor outcomes conferred by preoperative anemia. Transfusion, independent of preoperative anemia, has been associated with increased risks of postoperative complications and mortality.8,9 The risk appears to be dose-dependent; even a single-unit transfusion increased the risk of adverse outcomes.8 These findings may appear to be difficult to reconcile with those of randomized controlled studies, which have not shown the benefit of transfusion but have also not clearly shown a detrimental effect of liberal transfusion on patient outcomes.10 An analysis of the NSQIP database offers a possible explanation.9 Using the NSQIP database of over 450 000 patients, patients were divided into deciles of predicted increasing mortality and morbidity. When the risk of transfusion was added to this regression analysis, patients at lowest predicted risk of mortality and morbidity had an eightfold to 10-fold excess risk of complications when transfused. Those at highest predicted risk of mortality and complications had a nonsignificant risk of harm from transfusion. Overall, this supports not only the current standard of restrictive transfusion but also the concept that transfusion cannot compensate for the risk of preoperative anemia. Even though there have not yet been randomized controlled trials to show that treating preoperative anemia will definitively improve postoperative patient outcomes, the benefit of decreasing transfusion, in terms of the risks outlined above and the known risks of transfusion,7 is justification enough to proceed with preoperative anemia screening and management, particularly when simple and less expensive treatments for reversible causes are available.
What is preoperative anemia?
Recent advocates argue for a renewed definition of preoperative anemia in the setting of high-blood-loss surgery.11-13 Although the World Health Organization’s definitions of anemia have distinguished anemia for male patients as hemoglobin <13 g/dL and female patients as hemoglobin <12 g/dL,14 these definitions may not accurately address the risk of preoperative anemia. Female patients have lower circulating blood volume and, because the amount of blood loss is similar by procedure, are at risk of losing a greater proportion of their red cell mass. As a result, accepting a lower hemoglobin target puts female patients at higher risk of perioperative transfusions and, potentially, postoperative complications of both anemia and transfusion. In addition, preoperative hemoglobin below 13 g/dL increases the risk of morbidity, mortality, and transfusion regardless of sex.5,6,15 Thus, in the setting of high-blood-loss surgery, hemoglobin of 13 g/dL should be used to define preoperative anemia in both men and women.
Regarding the clinical case patient, his orthopedic surgeon, recognizing the importance of preoperative anemia, contacts the local preoperative anemia clinic. The clinic advises bloodwork to screen for causes of anemia and agrees to see the patient. The anticipated time to surgery is 6 weeks.
Preoperative anemia: prevalence, detection, and causes
Preoperative anemia is common, ranging from 25% to 40% in large observational studies depending on the population and the definition used.1,3,4,16 As in the general population,17 there are multiple causes of anemia in the preoperative patient. PBM guidelines offer pathways in the diagnosis of preoperative anemia.12,13,18-20 Screening should occur for patients undergoing high-blood-loss surgery (>500 mL) and those with a >10% risk of receiving a red cell transfusion. Targeted surgeries include cardiac, orthopedic, and cancer surgeries. Screening should occur with sufficient time for investigation and correction of anemia, typically 4 to 8 weeks before surgery. Laboratory testing to evaluate anemia should focus on the most common causes including nutritional deficiencies, specifically iron-deficiency anemia, chronic renal insufficiency, and/or anemia of inflammation/chronic disease. In practice, this translates to the following laboratory tests: hemoglobin, serum ferritin, transferrin saturation, serum vitamin B12, and creatinine, with some guidelines suggesting a measure of inflammation such as C-reactive protein. Although some guidelines recommend screening for folic acid deficiency, this is extremely uncommon in areas with nutritional fortification, and should not be routinely performed in these jurisdictions.21
Iron-deficiency anemia deserves special attention as it is the most common cause of anemia worldwide17 and has available treatments. Iron-deficiency anemia is defined variably in the literature depending on the condition.19,22,23 Serum ferritin is the most predictive test for iron-deficiency anemia.24 Absolute iron-deficiency anemia is defined by a serum ferritin <30 μg/L.13,18,19 This cutoff has a sensitivity of 92% and specificity of 98% for iron-deficiency anemia as compared with a bone marrow biopsy or response to iron therapy.25 However, ferritin is an acute-phase reactant and may be elevated in states of inflammation. In these cases, transferrin saturation <20% with ferritin of 100 μg/L is also used. In the 2017 international consensus conference on perioperative anemia and iron-deficiency anemia,13 absolute iron deficiency was defined as serum ferritin <30 μg/L, or, in the presence of inflammation, serum ferritin 30 to 100 μg/L with transferrin saturation <20% and/or C-reactive protein >5 mg/L. Low iron stores were defined as ferritin <100 μg/L and transferrin saturation >20% for surgery with moderate to high blood loss. Using these criteria, a multicenter cohort of 3342 patients undergoing major elective surgery (orthopedic, cardiac, colorectal cancer, gynecologic, liver metastases surgery, and prostatectomy) was assessed.16 In anemic patients (hemoglobin <13 g/dL for both sexes), 62% had absolute iron-deficiency anemia and 15% had low iron stores. Even in nonanemic patients, 33% had absolute iron deficiency and 27% had low iron stores. Thus, iron deficiency was very common and easily detectable.
It should be noted that additional tests for iron status have been described and may be particularly helpful in distinguishing iron deficiency in anemia of inflammation or functional iron deficiency or in predicting response to IV iron.26 The percentage of hypochromic red cells (defined as red cells with hemoglobin <280 g/L) of ≥6% may indicate iron deficiency in patients with chronic kidney disease receiving erythropoiesis-stimulating agents (ESAs). Reticulocyte hemoglobin content, a measure of reticulocyte mean corpuscular hemoglobin, <29 pg may predict a response to IV iron. Reticulocyte hemoglobin equivalent, a measure of reticulocyte hemoglobin content, <25 pg may be indicative of iron deficiency rather than anemia of inflammation (>25 pg) in patients receiving ESAs. A reticulocyte hemoglobin equivalent of <30.6 pg has been found to be the best predictor of a response to IV iron therapy in patients on hemodialysis. Soluble transferrin receptor increases in iron deficiency and states of active erythropoiesis and may help to distinguish from inflammatory states; however, this test is expensive and is not standardized or widely available. For an in-depth review, please refer to “New diagnostic tools for delineating iron status” (see Ginzburg, in this book27 ).
Finally, even in the preoperative setting, it is critical to identify the etiology of iron-deficiency anemia. Anemia is a symptom, not a diagnosis! The most common cause of iron deficiency is bleeding. The prevalence of gastrointestinal lesions may be as high as 1% to 5% for upper lesions and 5% to 10% for colonic lesions.28 In a study of 639 patients referred for investigation of iron-deficiency anemia to a gastroenterology clinic, 42% were found to have pathology.29 Thus, it is recommended that postmenopausal women and all male patients with confirmed iron-deficiency anemia should have upper and lower gastrointestinal investigations unless there is another clear explanation of blood loss. Other causes of iron-deficiency anemia are listed in Table 1.
Causes of iron-deficiency anemia in the preoperative setting
| Causes of preoperative iron-deficiency anemia . |
|---|
| Too much iron OUT |
| Increased loss |
| • Blood loss, eg, gastrointestinal, gynecological bleeding |
| • Blood donation |
| Increased requirements |
| • Rapid growth in infants and children |
| • Pregnancy |
| • Use of ESAs |
| Too little iron IN |
| Decreased iron intake |
| • Iron-poor diet |
| • Vegetarian or vegan |
| Decreased absorption |
| • Celiac disease |
| • Gastrectomy, gastric bypass, gut resection |
| • Helicobacter pylori |
| • Inflammatory bowel disease |
| • Drugs: antacids, proton pump inhibitors |
| • Foods: calcium, tannins (tea, coffee), phytates |
| Causes of preoperative iron-deficiency anemia . |
|---|
| Too much iron OUT |
| Increased loss |
| • Blood loss, eg, gastrointestinal, gynecological bleeding |
| • Blood donation |
| Increased requirements |
| • Rapid growth in infants and children |
| • Pregnancy |
| • Use of ESAs |
| Too little iron IN |
| Decreased iron intake |
| • Iron-poor diet |
| • Vegetarian or vegan |
| Decreased absorption |
| • Celiac disease |
| • Gastrectomy, gastric bypass, gut resection |
| • Helicobacter pylori |
| • Inflammatory bowel disease |
| • Drugs: antacids, proton pump inhibitors |
| • Foods: calcium, tannins (tea, coffee), phytates |
With regard to the clinical case patient, his laboratory tests are as follows: hemoglobin, 10.3 g/dL; mean corpuscular volume, 75 fL; ferritin, 25 μg/L; transferrin saturation, 8%; vitamin B12, 312 pmol/L; creatinine, 1.70 mg/dL. Six months ago, the patient had an esophagogastroduodenoscopy and a colonoscopy that were unremarkable; it was noted that he has had persistent chronic anemia over the past 5 years. He has been vegan for 10 years and this has been the presumed cause. His creatinine has been elevated but stable over the past 2 years and is thought to be due to longstanding hypertension.
Managing preoperative anemia
Iron-deficiency anemia should be treated with iron supplementation. Oral iron should be first-line therapy if there is sufficient time to obtain effect prior to surgery (>6 weeks).13 There are few randomized studies on the role of oral iron in preoperative anemia.30 One small study showed increases in hemoglobin and decreases in transfusion rates with oral iron but the number of patients enrolled was small. There does not appear to be any benefit when oral iron is given postoperatively,31 which may be due to decreased absorption in the setting of the acute inflammatory postoperative response. Oral iron salts are the mainstay of therapy: ferrous gluconate, sulfate, and fumarate (35, 60, and 100 mg of elemental iron per 300-mg tablet, respectively). These should be taken on an empty stomach with vitamin C to maximize absorption.32 Gastrointestinal side effects are common, leading to poor adherence, and include constipation, nausea, diarrhea, abdominal pain, vomiting, heartburn, flatulence, and dark stools. Newer iron formulations are available; however, these do not appear to be more effective in improving hemoglobin and ferritin levels and may potentially be inferior.33,34 Finally, there are early data suggesting that more efficient absorption of oral iron may occur with 40 to 80 mg of elemental iron and every-other-day dosing because of an increase in hepcidin after oral intake35,36 ; this forms the basis of current ongoing clinical trials (clinicaltrials.gov NCT03562143, NCT037006638, and NCT03725384).
In cases where oral iron is not tolerated or effective, there is a short time to surgery (<4-6 weeks), or there is severe anemia (eg, hemoglobin <10 g/dL), IV iron should be considered.13,19,37 In some guidelines, IV iron may be preferred to oral iron as initial therapy depending on the etiology of iron-deficiency anemia.20,37 In a systematic review of perioperative IV iron, an increase in hemoglobin was noted in 11 of 17 studies included and a decrease in transfusion was noted in 8 of 13 studies with the strongest evidence for preoperative use.38 IV iron is generally well tolerated.39 Available formulations are detailed in Table 2. The dose of IV iron can be calculated using the Ganzoni formula, where total iron dose (mg iron) = body weight (kg) × [target − initial hemoglobin g/dL] × 2.4, with the addition of 500 mg for iron stores. This typically translates into doses of 1000 to 1500 mg depending on the body weight and degree of anemia.13,40 The optimal timing of IV iron is 2 to 4 weeks preoperatively although even when given the day before surgery, there may be an improvement of postoperative hemoglobin recovery.16 Side effects include (rarely) anaphylactic reactions (24 per 100 000),41 hypotension, muscle cramps, arthralgias, back pain, and headache. Recommendations exist to improve the safety of IV iron administration with focus on managing the rare reactions should they occur.42
IV iron formulations
| Characteristic . | Ferric carboxymaltose (Ferinject, Injectafer) . | Ferumoxytol (Feraheme, Rienso) . | Iron isomaltoside 1000 (Monofer, Monoferric) . | Iron sucrose (Venofer) . | LMW iron dextran (CosmoFer, DexIron, INFeD) . | Sodium ferric gluconate (Ferrlecit) . |
|---|---|---|---|---|---|---|
| Availability | Europe, USA | Europe, USA | Canada, Europe | Canada, Europe, USA | Canada, Europe, USA | Canada, USA |
| Indication* | Iron deficiency when oral iron cannot be used | Iron-deficiency anemia in adults with CKD | Iron-deficiency anemia when oral iron cannot be used (or rapid iron supply required [Europe only]) | Iron deficiency in CKD (or when oral iron cannot be used or rapid iron supply required [Europe only]) | Iron deficiency when oral iron cannot be used (or rapid iron supply required [Europe only]) | Iron deficiency in hemodialysis patients receiving erythropoietin therapy |
| Carbohydrate shell | Carboxymaltose | Polyglucose sorbitol | Isomaltoside | Sucrose | Dextran | Gluconate |
| Molecular weight, kDa | 150 | 750 | 150 | 43 | 400 | 289–440 |
| Volume distribution, L | 3 | 3.16 | N/A | ∼3 | N/A | 6 |
| Test dose required | No | No | No | No | In Canada/USA only | No |
| Maximum single dose | 750 mg (USA) | 510 mg | 1500 mg | 500 mg | 100 mg | 125 mg |
| 1000 mg (Europe) | ||||||
| Infusion rate or time† | ≥15 min | Injection at ≤1 mL/s (≤30 mg/s) | ≥15 min (≤1000 mg, Europe); ≥20 min (≤1000 mg, Canada); ≥30 min (>1000 mg) | 8 min (50 mg); 15 min (100 mg); 30 min (200 mg); 1.5 h (300 mg); 2.5 h (400 mg) | First 25 mg over 15 min, remaining dose at <100 mL/30 min; total dose infusion over 4-6 h | 1 h |
| Characteristic . | Ferric carboxymaltose (Ferinject, Injectafer) . | Ferumoxytol (Feraheme, Rienso) . | Iron isomaltoside 1000 (Monofer, Monoferric) . | Iron sucrose (Venofer) . | LMW iron dextran (CosmoFer, DexIron, INFeD) . | Sodium ferric gluconate (Ferrlecit) . |
|---|---|---|---|---|---|---|
| Availability | Europe, USA | Europe, USA | Canada, Europe | Canada, Europe, USA | Canada, Europe, USA | Canada, USA |
| Indication* | Iron deficiency when oral iron cannot be used | Iron-deficiency anemia in adults with CKD | Iron-deficiency anemia when oral iron cannot be used (or rapid iron supply required [Europe only]) | Iron deficiency in CKD (or when oral iron cannot be used or rapid iron supply required [Europe only]) | Iron deficiency when oral iron cannot be used (or rapid iron supply required [Europe only]) | Iron deficiency in hemodialysis patients receiving erythropoietin therapy |
| Carbohydrate shell | Carboxymaltose | Polyglucose sorbitol | Isomaltoside | Sucrose | Dextran | Gluconate |
| Molecular weight, kDa | 150 | 750 | 150 | 43 | 400 | 289–440 |
| Volume distribution, L | 3 | 3.16 | N/A | ∼3 | N/A | 6 |
| Test dose required | No | No | No | No | In Canada/USA only | No |
| Maximum single dose | 750 mg (USA) | 510 mg | 1500 mg | 500 mg | 100 mg | 125 mg |
| 1000 mg (Europe) | ||||||
| Infusion rate or time† | ≥15 min | Injection at ≤1 mL/s (≤30 mg/s) | ≥15 min (≤1000 mg, Europe); ≥20 min (≤1000 mg, Canada); ≥30 min (>1000 mg) | 8 min (50 mg); 15 min (100 mg); 30 min (200 mg); 1.5 h (300 mg); 2.5 h (400 mg) | First 25 mg over 15 min, remaining dose at <100 mL/30 min; total dose infusion over 4-6 h | 1 h |
Reproduced from Lim et al42 with permission.
CKD, chronic kidney disease; LMW, low molecular weight; N/A, information not available in product monograph; USA, United States of America.
Specific indications vary across jurisdictions; refer to relevant product information. Off-label use of certain products is not uncommon, but should be done in the context of full disclosure to the patient.
Minimum infusion time as per product information, which may vary across jurisdictions.
Although the management of iron-deficiency anemia has not been definitively shown to improve clinical outcomes, large trials are under way. The PREVENTT study is assessing the role of preoperative IV iron to treat patients undergoing major abdominal surgery with a primary outcome of blood transfusion or death at 30 days (N = 500) (clinicaltrials.gov NCT01692418). The ITACS study is assessing the role of IV iron for patients with anemia undergoing cardiac surgery with the primary outcome of days alive and out of hospital to 30 days postsurgery (N = 1000) (clinicaltrials.gov NCT02632760).
The role of ESAs in preoperative anemia management is not clear with some guidelines stating that it is not routinely recommended (unless the patient has religious objections to blood, or appropriate blood is not available due to red cell antibodies),37 other guidelines making no specific recommendation,19 and others suggesting or supporting its use when nutritional anemias are not the cause of anemia.18,20 Concerns have centered on increased cardiovascular risk described with ESA use in chronic kidney disease and in the setting of cancer, with respect to controversial effects of tumor progression and increased mortality.43 In these trials, the use of ESAs was prolonged for at least >16 months in chronic kidney disease and >8 weeks in cancer use. Two recent systematic reviews provide guidance specifically in preoperative surgical patients and give some reassurance as to the effectiveness and safety of ESAs. In 32 trials of 4750 patients, preoperative ESA decreased the risk of transfusion (OR, 0.59; 95% CI, 0.47-0.73) with no associated increase in thrombosis (OR, 1.07; 95% CI, 0.79-1.44).44 The second systematic review specifically examined the role of ESAs with iron compared with iron therapy alone. In 25 studies of 4739 patients, the combination of ESA with iron therapy decreased the risk of transfusion (relative risk [RR], 0.57; 95% CI, 0.46-0.71). There were no statistical differences in serious adverse events (mortality RR, 1.31; 95% CI, 0.80-2.16; deep vein thrombosis RR, 1.48, 95% CI, 0.95-2.31).45 Thus, ESAs are likely safe in the preoperative setting where ESAs are administered for a short period of time, <2 to 4 weeks. The question of cost effectiveness and overall effect on patient outcomes is, however, less clear.
In patients who refuse blood transfusions or those with multiple alloantibodies for whom compatible blood cannot be adequately sourced, managing preoperative anemia is essential along with a multidisciplinary approach to minimizing blood loss. The use of ESAs in these cases is often more liberal and higher hemoglobin thresholds may be required depending on the surgical procedure. Preoperative planning is essential to ensure that the patient’s choices of transfusion alternatives are clearly stated.46
The patient from the clinical case returns at 4 weeks prior to surgery after a 2-week trial of oral ferrous sulfate and has not been able to tolerate oral iron due to constipation and gastrointestinal upset. A repeat hemoglobin is 10.3 g/dL. The preoperative anemia clinic schedules weekly appointments for IV iron but there are no available appointments until 3 weeks prior to surgery.
Challenges and key considerations in setting up a preoperative anemia clinic
There is no doubt that PBM programs have been successful in reducing blood utilization and have been associated with improved patient outcomes.47,48 One example of a program with an emphasis on preoperative anemia management is the Ontario Transfusion Coordinators (ONTraC) PBM program in Ontario, Canada.5,49 The ONTraC program was established in 2002 with the support of the Ontario Ministry of Health and Longterm Care. Funding was provided for the placement of nurse coordinators in 25 hospitals in the province. Their role is to assess and manage preoperative anemia, manage data for central reporting, and participate in local institutional activities related to blood management. The program specifically targets key, high risk for transfusion, surgical procedures (eg, coronary artery bypass surgery, cardiac valve surgery, knee arthroplasty, hip arthroplasty, and benign open hysterectomy and myomectomies). The coordinators focus not only on anemia diagnosis and treatment of preoperative patients but also on collection of data on perioperative hemoglobins, transfusions, and outcomes. Over time, there has been a significant decrease in transfusion: for example, for isolated elective coronary artery bypass graft surgery, the mean provincial transfusion rate decreased from 60.1% in 2002 to 24.4% in 2018; and for primary total knee arthroplasty from 24.5% in 2002 to 0.57% in 2018 (J. Freedman, ONTraC program, written communication, 28 April 2019). There are many steps that must be considered when setting up a preoperative anemia clinic and these have been reviewed in detail elsewhere: institutional rationalization of the clinic, determination of a target pilot population, creation of a business case, mobilization of resources in terms of space and staff, development of anemia diagnosis and treatment algorithms, clinical workflow design and clinical and laboratory data integration into the electronic health record.50 A few practical key ingredients that should be highlighted include:
People. A PBM coordinator is required to assess patients and coordinate the preoperative anemia management. In addition, a physician champion is essential to help establish anemia management algorithms and support the preoperative anemia clinic especially when patients present with complex histories, potential contraindications to therapy, or need referral for further investigation or management of anemia.
Early detection of anemia. Although this seems simple, getting a complete blood count done early in the preoperative phase can be quite challenging. There may be a long delay between the visit with the surgeon to surgery and a very short window from the preoperative assessment clinic and surgery. For some procedures, the preoperative assessment visit may occur within 1 to 2 weeks of surgery, which is a suboptimal time period for appropriate anemia management. Meeting with surgical services to understand how patients flow through the system and where best to introduce baseline bloodwork is key. For example, at our institution, for orthopedic surgery, we introduced a process to involve primary care providers in assessing and treating anemia early on at the time of physiotherapy assessment, typically starting 3 to 6 months prior to surgery and often before the patient meets the surgeon. In cases of iron-deficiency anemia, patients can be appropriately investigated for the underlying cause, and treatment with oral iron can be initiated with sufficient time for response, abrogating the need for IV iron. When patients are assessed at 4 weeks prior to surgery, patients who have not improved can move on to IV iron and/or consideration of ESAs.
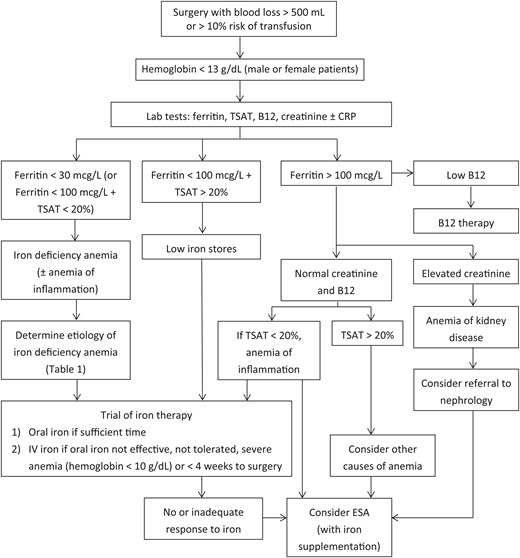
Anemia management algorithms. Preoperative anemia algorithms have been developed to guide and streamline the approach to its investigation and management (Figure 1).12,19,51 These may vary, particularly with respect to target hemoglobins based on the surgery, especially when resources are limited. They may also be tailored to the specific institution and specific pharmacologic therapies (eg, type of iron or ESA) available. Establishing treatment algorithms also encourages the involvement of the frontline clinical team (clinic nurses, physicians, preoperative assessment clinic nurses) who are often the first to assess the patient.
Access to IV iron. Clinic space for administration of IV iron can be challenging (given the administration time [Table 2] and monitoring for 30 minutes postinfusion42 ) and business cases may need to be developed to support this activity within one’s institution. Although costs vary and oral iron therapy is generally inexpensive, IV iron preparations can be costly. However, these must be compared with the activity-based cost of a blood transfusion, estimated to be $761 (US) dollars per red blood cell unit,52 and the gains of improving patient safety.
Quality improvement measures. Finally, it is key to track measures to demonstrate the local benefit of preoperative anemia management. Transfusion rates should be monitored over time and additional outcomes such as improvement in preoperative hemoglobin, length of stay, readmissions, infections, and patient satisfaction may also be desired indicators.12 These data are not only important to feed back to clinical teams but should also be used for ongoing quality improvement efforts and to justify the ongoing costs of the preoperative anemia clinic.
Preoperative anemia management algorithm.12,19,51 CRP, C reactive protein; ESA, erythropoiesis stimulating agent; TSAT, transferrin saturation.
Preoperative anemia management algorithm.12,19,51 CRP, C reactive protein; ESA, erythropoiesis stimulating agent; TSAT, transferrin saturation.
In summary, preoperative anemia is an important and modifiable risk for surgical patients. Its treatment reduces the need for transfusion and improves patient outcomes. Approaches to the early detection, diagnosis, and management of preoperative anemia are key elements of PBM. Establishment of focused anemia clinics can advance these goals. The paradigm has changed: no longer can we regard anemia as generally “benign” and easily correctable with blood transfusion.
Finally, regarding the clinical case patient, he initiates IV iron at 3 weeks prior to surgery and received 1 g IV iron. His hemoglobin is checked 1 week later to ensure an adequate response in the setting of anemia of kidney disease: hemoglobin is 11.2 g/dL and reticulocyte count is 134 × 109/L. As he is responding to iron alone, he does not receive additional erythropoietin. On the day of surgery, his hemoglobin is 12.8 g/dL. He proceeds with knee surgery and receives tranexamic acid intraoperatively. His nadir hemoglobin is 9.5 g/dL and he does not require a transfusion. His postoperative course is smooth and he is discharged to a rehabilitation facility.
Acknowledgment
The author thanks John Freedman and Jeannie Callum for their review of the manuscript.
Correspondence
Yulia Lin, Department of Laboratory Medicine and Molecular Diagnostics, Sunnybrook Health Sciences Centre, Room B2-04, 2075 Bayview Ave, Toronto, ON M4N 3M5, Canada; e-mail: yulia.lin@sunnybrook.ca.
References
Competing Interests
Conflict-of-interest disclosure: Y.L. has received research funding from Novartis and Octapharma and consulting fees from Amgen and Pfizer.
Author notes
Off-label drug use: None disclosed.