Abstract
The direct oral anticoagulants (DOACs) have transformed the management of thrombotic disorders. Large clinical trials have demonstrated that DOACs can replace vitamin K antagonists (VKAs) in the 2 existing major indications for anticoagulation: the prevention of stroke in atrial fibrillation and the acute treatment and secondary prevention of venous thromboembolism (VTE); this literature is widely known. In this article, we will concentrate on the less well-discussed benefits of the use of DOACs—using low doses as primary and secondary prophylaxis in both venous and arterial thromboprophylaxis. The attractiveness of using a low-dose DOAC is that the bleeding risk seems to be slightly lower than with the standard dose and significantly lower than with VKAs so that they can be used safely for long periods, where previously, VKAs had risk/benefit ratios that did not permit this. We discuss in detail the extended use of low-dose DOACs in secondary VTE prevention. We also cover the utility of low-dose DOACs in the evolving fields of prevention of hospital-associated VTE in acutely ill medical patients, after total hip and knee replacement, and in cancer patients. To complete the indications, we briefly discuss the role of low-dose DOACs in the secondary prevention of arterial vascular events.
Learning Objectives
Understand the place of low-dose direct oral anticoagulants (DOACs) in the prevention of hospital-associated venous thromboembolism in acutely ill medical patients, cancer patients, and after total hip replacement and total knee replacement
Understand the utility of low-dose DOACs in the secondary prevention of venous thromboembolism
Understand the utility of low-dose DOACs in the primary and secondary prevention of arterial thrombosis
Case 1
A 46-year-old man has an unprovoked pulmonary embolism (PE) and received treatment at his local hospital with rivaroxaban 15 mg twice daily for 3 weeks and then, 20 mg daily. He returns for review 3 months after the event. He has no ongoing risk factors for venous thromboembolism (VTE) apart from a body mass index of 34.7. Investigations for thrombophilia and cancer reveal no abnormality. After discussion with his physician as to the increased risks of recurrent VTE events after an unprovoked PE and being male and obese, he elects to continue anticoagulation with rivaroxaban 10 mg daily. Over the next 3 years, he has no additional VTE events or adverse effects from his medication.
Introduction
The arrival of the direct oral anticoagulants (DOACs) has transformed the management of thrombotic disorders. Large clinical trials have demonstrated that DOACs can replace vitamin K antagonists (VKAs) in the 2 existing major indications for anticoagulation: the prevention of stroke in atrial fibrillation and the acute treatment and secondary prevention of VTE; this literature is widely known.
The DOACs exist in 2 forms, either directly acting as a direct anti-Xa agent (apixaban, betrixaban, edoxaban, and rivaroxaban) or acting as a direct antithrombin agent (dabigatran). In contrast to the other oral anticoagulants, the VKAs, they are characterized by their reliable pharmacokinetics, short half-life, the reassurance that they as a group are not affected by diet or alcohol, and lower rate of interactions with other pharmacological agents,
Sixty percent of VTE occur as result of hospital admission,1-3 causing an estimated 10 million cases a year.4 Hospital-associated VTE (VTE occurring during admission or in the 90 days postdischarge) is the number 1 preventable consequence of hospital admission in low- and middle-income countries, and it is the primary cause of disability adjusted life years in high-, middle-, and low-income countries.4 Primary prevention of hospital-acquired VTE with low-dose anticoagulation is an important area of prevention and when applied systematically as is practiced by National Health Service England, has led to a 9% fall in death owing to PE annually.5 The current standard of care is the use of low-molecular weight heparin (LMWH); however, trials of DOACs have shown benefit.
Secondary prevention of VTE is important in those with a high risk of recurrence. There is international agreement that those with unprovoked events, especially if the events are pulmonary emboli, or occurring in men, or had other comorbid risk factors, such as obesity or a high-risk thrombophilia, require long-term anticoagulation. In all of these groups, the benefits of prevention of thrombosis must be balanced against the safety of these agents (ie, the risk of bleeding).6 The attractiveness of using a low-dose DOAC is that the bleeding risk seems to be slightly lower than with the standard dose and significantly lower than with VKAs so that they can be used safely for long periods, where previously, VKAs had risk/benefit ratios that did not permit this.7-9 In this paper, we will discuss in detail the extended use of low-dose DOACs in secondary VTE prevention. To complete the indications, we briefly discuss the role of low-dose DOACs in the secondary prevention of arterial vascular events.
Orthopedic surgery: case 2
A 69-year-old man who was previously fit and active with a history of regular running had developed severe pain in the left knee, which was not well controlled by medication. This pain had curtailed his activity, and he was walking with an antalgic gait and walking stick. His knee imaging showed extensive osteoarthritis, and an elective knee replacement was planned.
In the absence of pharmacological prophylaxis, the incidence of deep venous thrombosis (DVT) among patients undergoing total hip arthroplasty (THA) is 40% to 60%, of which 2% to 5% are symptomatic.10,11 Similarly, the incidence of VTE among patients undergoing total knee arthroplasty (TKA) without prophylactic anticoagulation is as high as 85%.10,11 With contemporary VTE prophylaxis, 1.1% of patients undergoing TKA and 0.5% of patients undergoing THA will suffer symptomatic VTE before hospital discharge.12
Three DOACs—apixaban, dabigatran, and rivaroxaban—have been licensed for use in thromboprophylaxis in hip and knee replacement across the world, and edoxaban is used in Japan in this setting. The 2012 American College of chest Physicians guidelines for the prevention of VTE in orthopedic patients recommend the DOACs on an equal footing with LMWH, unfractionated heparin (UFH), fondaparinux, aspirin, and intermittent pneumatic compression.13
Rivaroxaban
Rivaroxaban is a DOAC, and it is approved for the prevention of VTE after THA and TKA. The dose of 10 mg started 6 to 8 hours postoperatively has been evaluated against enoxaparin, which was usually started before surgery and given in a dose of 40 or 30 mg twice daily in 7 randomized controlled trials (RCTs) enrolling >10 000 patients. The outcome data are summarized in Table 1. Rivaroxaban was given for 10 to 15 days; earlier trials in THR had similarly short duration, but 1 later trial treated for 31 to 39 days. Of note, compared with the other DOACs, there was a trend toward increased major bleeding and bleeding requiring reoperation (Table 1). Thus, based on moderate-quality evidence, fewer VTE events would be expected than LMWH, but because of concerns about the bleeding rate, there is uncertainty as to whether the benefits in efficacy of rivaroxaban are offset by the higher bleeding rates seen.
Summary of the randomized trials of DOACs vs LMWHs in total hip and knee replacement and the effect of nonfatal PE, symptomatic DVT, bleeding requiring reoperation, and major nonfatal bleeding (data adapted from the ACCP guidelines)13
| DOAC . | No. in trials . | RR (95% CI) of nonfatal PE . | RR (95% CI) of symptomatic DVT . | RR (95% CI) of bleeding requiring reoperation . | RR (95% CI) of major nonfatal bleeding . |
|---|---|---|---|---|---|
| Rivaroxaban | 10 869 (7 studies) | RR, 1.34 (0.39-4.6) | RR, 0.41 (0.2-0.83) | RR, 2.03 (0.86-4.83) | RR, 1.58 (0.84-2.97) |
| Dabigatran | 7 377 (4 studies) | RR, 1.22 (0.52-2,85) | RR, 0.70 (0.12-3.91) | RR, 0.98 (0.27-3.54) | RR, 1.06 (0.66-1.72) |
| Apixaban | 11 964 (4 studies) | RR, 1.09 (0.31-3.88) | RR, 0.41 (0.18-0.95) | RR, 0.82 (0.15-4.58) | RR, 0.76 (0.44-1.32) |
| DOAC . | No. in trials . | RR (95% CI) of nonfatal PE . | RR (95% CI) of symptomatic DVT . | RR (95% CI) of bleeding requiring reoperation . | RR (95% CI) of major nonfatal bleeding . |
|---|---|---|---|---|---|
| Rivaroxaban | 10 869 (7 studies) | RR, 1.34 (0.39-4.6) | RR, 0.41 (0.2-0.83) | RR, 2.03 (0.86-4.83) | RR, 1.58 (0.84-2.97) |
| Dabigatran | 7 377 (4 studies) | RR, 1.22 (0.52-2,85) | RR, 0.70 (0.12-3.91) | RR, 0.98 (0.27-3.54) | RR, 1.06 (0.66-1.72) |
| Apixaban | 11 964 (4 studies) | RR, 1.09 (0.31-3.88) | RR, 0.41 (0.18-0.95) | RR, 0.82 (0.15-4.58) | RR, 0.76 (0.44-1.32) |
95% CI, 95% confidence interval; RR, relative risk.
More recently, a nonindustry, randomized, controlled trial was led by Anderson et al.14 It studied a population of 3423 patients undergoing hip or knee replacement who were given 5 days of rivaroxaban 10 mg and then, randomized to receive rivaroxaban 10 mg or aspirin 100 mg for 9 days after knee replacement or 30 days after hip replacement; they were followed for 90 days to look at the rate of VTE. Interestingly, there were no significant differences in VTE rates between aspirin (0.46%) and rivaroxaban (0.7%) or major bleeding in aspirin (0.47%) vs rivaroxaban (0.29%).14
Dabigatran
Dabigatran is the only licensed oral direct thrombin inhibitor available. Four RCTs examined the use of dabigatran in >10 000 patients undergoing THA and TKA at doses of 220 and 150 mg taken orally once daily, although usually started within 4 hours postoperatively at half the dose. The comparisons were made with either 40 or 30 mg enoxaparin twice daily given 10 to 15 days after TKA or 28 to 35 days for THA. The studies using 220 mg dabigatran showed no difference between rates of VTE or major bleeding (Table 1). There was a smaller reduced symptomatic DVT rate when 150 mg dabigatran was used compared with LMWH (PE: RR, 0.31; 95% confidence interval [95% CI], 0.04-2.28; symptomatic DVT: RR, 1.52; 95% CI, 0.45-5.05). Overall, dabigatran showed a similar profile to LMWH, and the dose of 110 mg was licensed. However, the ACCP argue that, because of the longer experience of the use of LMWH, it should be used in preference to dabigatran.
Apixaban
Apixaban is an oral direct FXa inhibitor that has been evaluated in 4 RCTs including nearly 12 000 patients. Apixaban 2.5 mg twice daily was given starting 12 to 24 hours postoperatively against enoxaparin 40 mg daily, or in 2 studies, 30 mg were given twice daily. After TKA, apixaban was given for 10 to 14 days, and a single trial after THA used 32 to 38 days. Compared with enoxaparin, there was no difference in nonfatal bleeding, bleeding requiring reoperation, or nonfatal PE, but there was a 59% reduction in symptomatic DVT compared with enoxaparin.
In summary, based on moderate-quality evidence, apixaban has similar efficacy and bleeding rates compared with LMWH, but once again, the ACCP recommended LMWH over apixaban because of the long availability of safety data for LMWH.
Summary
Recent health economic analysis of the use of thromboprophylaxis in THA and TKA based on the English health care system using NICE data controversially suggests that LMWH, aspirin, and mechanical methods are more cost effective than using DOACs owing to the uncertainty around bleeding risk with DOACs. In the weighting of costs, it was recognized that a repeat operation to manage a bleeding event is enormously costly.15
Importantly, over last 50 years, there has been a background fall in VTE rates after THA and TKA surgery probably unrelated to just to the use of thromboprophylaxis and likely owing to better anesthesia, surgery with shorter operating times, and “fast-track” surgery (also known as enhanced recovery describing early mobilization and discharge).16 In a systematic review and meta-analysis of trials over the last 50 years, the mortality declined from 1.15% pre-1980 to 0.24% post-2000, a 78.7% relative risk reduction (95% CI, 74.7%-82.1%), in randomized and cohort studies. The data suggested a 74% (95% CI, 69%-79.0%) relative reduction in mortality independent of the methods of prophylaxis. This impressive claim suggests that the change in surgical practice may mean that the need for intensive thromboprophylaxis with the current anticoagulants is past. Of course, there is still an ongoing need in surgical practice for thromboprophylaxis; indeed, better anticoagulants are needed to further reduce the VTE rates (ie, an anticoagulant nearer the ideal of an anticoagulant with maximal efficacy and no bleeding risk); there are several agents on the horizon showing promise in reaching that goal.
According to most international guidelines, our 69-year-old patient undergoing a TKA has an indication for low-dose DOAC, LMWH, or mechanical thromboprophylaxis for at least 10 to 14 days or longer up to 5 weeks.
Acute medical illnesses: case 3
A 77-year-old man is admitted to the ED with persistent cough, dyspnea, and bilateral edema in the legs, and he is diagnosed with an acute heart failure exacerbation. He has past history of a DVT 10 years ago. He has difficulty moving about and was brought to the Emergency Department (ED) by his wife who says that, because of his breathing difficulty, he was experiencing restricted mobility and unable to get out of bed for the past 3 days.
Initial trials in acutely ill medical patients at moderate and high risk for VTE showed that low-dose parenteral anticoagulants, such as heparins, LMWH, and fondaparinux, have efficacy in reducing symptomatic and fatal PE when used for 6 to 14 days.17 Despite the administration of standard duration thromboprophylaxis, there remains an ongoing VTE-related burden of morbidity and mortality in acutely ill medical patients at high risk of VTE that extends for at least 6 weeks after admission to hospital.18 It is to address this ongoing risk that DOACs have been used in this setting. The patient described above should be assessed for an increased risk of hospital-associated thrombosis postdischarge.
Current guidelines and routinely used risk assessment tools identify both moderate- and high-risk patients who benefit from standard duration thromboprophylaxis and do not specifically recognize high-risk patients requiring extended prophylaxis (ACCP 2012).19 A controversial meta-analysis of extended thromboprophylaxis combining unlicensed and licensed doses of DOACs was used in the recent ASH guidelines to recommend against extended prophylaxis in this setting.20 Hence, there is no guidance for risk assessment of high-risk patients. Consequently, there is lack of clarity as to which patients will benefit from extended thromboprophylaxis.
Previous extended pharmacological thromboprophylaxis trials with LMWH, apixaban, and rivaroxaban for patients with acute medical illnesses showed promise in reducing VTE but did not show net benefit because of increased major bleeding.21-24 These studies provided evidence for risk factors associated with an extended risk of VTE, such as immobility, advanced age, a past history of VTE or cancer, and elevated D-dimer, and have guided 2 more recent studies: the The Acute Medically Ill VTE (Venous Thromboembolism) Prevention with Extended Duration Betrixaban (APEX) trial with betrixaban and the A Study of Rivaroxaban (JNJ-39039039) on the Venous Thromboembolic Risk in Post-Hospital Discharge Patients (MARINER) trial with rivaroxaban.21,25 Our case study has a number of these risk factors.
In the APEX trial, the use of risk factors, such as advanced age, a past history of VTE or cancer, and elevated D-dimer, as inclusion criteria was associated with the highest risk of VTE seen in the 5 major studies for both symptomatic VTE and total VTE (symptomatic and asymptomatic; 7% in the standard therapy arm) and a clinically meaningful response to extended thromboprophylaxis with betrixaban. At 2 to 3 months, the symptomatic burden of VTE in acutely ill hospitalized patients can be reduced by up to 45% with extended duration betrixaban (1.02% vs 1.89%; ARR, 0.87%; hazard ratio [HR], 0.55; 95% CI, 0.37-0.83; P = .003) without increasing major bleeding (0.7% vs 0.6%; RR, 1.19; 95% CI, 0.67-2.12; P = .55).26 This reduction in symptomatic VTE (a combination of fatal and nonfatal VTE) was associated with reduction in VTE-related rehospitalizations within 30 days of hospital discharge, and reduction in ischemic strokes.27,28 The efficacy and safety of trials that investigated symptomatic nonfatal and fatal VTE and proximal asymptomatic DVT are shown in Figure 1 (the MARINER trial discussed below is not shown, because this trial only assessed symptomatic nonfatal and fatal VTE).
Clinical events in extended thromboprophylaxis trials investigating both symptomatic and asymptomatic VTE. ADOPT, Apixaban Dosing to Optimize Protection from Thrombosis; APEX, The Acute Medically Ill VTE (Venous Thromboembolism) Prevention with Extended Duration Betrixaban; EXCLAIM, Extended Prophylaxis for Venous Thromboembolism in Acutely Ill Medical Patients with Prolonged Immobilization trial; MAGELLAN, Venous Thromboembolic Event [VTE] Prophylaxis in Medically Ill Patients.
Clinical events in extended thromboprophylaxis trials investigating both symptomatic and asymptomatic VTE. ADOPT, Apixaban Dosing to Optimize Protection from Thrombosis; APEX, The Acute Medically Ill VTE (Venous Thromboembolism) Prevention with Extended Duration Betrixaban; EXCLAIM, Extended Prophylaxis for Venous Thromboembolism in Acutely Ill Medical Patients with Prolonged Immobilization trial; MAGELLAN, Venous Thromboembolic Event [VTE] Prophylaxis in Medically Ill Patients.
The risk of VTE was moderate in the MARINER trial, and there was no difference in the combined outcome of symptomatic VTE or death from VTE (0.83% vs 1.10%; ARR, 0.27%; HR, 0.76; 95% CI, 0.52-1.09; P = .14). However, a subgroup analysis excluding fatal VTE events showed a 56% reduction in nonfatal symptomatic VTE (0.18% vs 0.42%). Major bleeding events were infrequent (0.28% vs 0.15%) for rivaroxaban and placebo, respectively.25
Summary
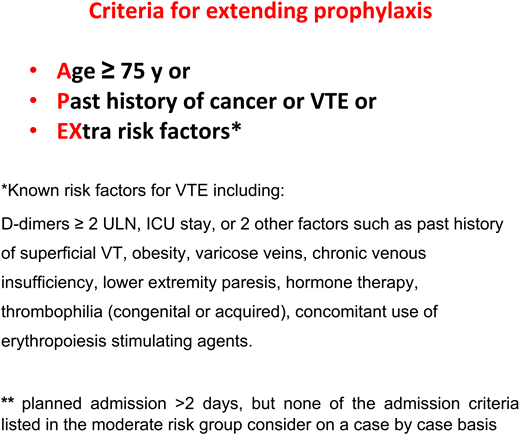
Our case is a patient with age over 75 years old (77) and a history of VTE who requires hospital admission for an acute medical illness. This patient would be considered at high risk for VTE both in the hospital and after hospital discharge and should be assessed for bleeding risk. He has an indication for in-hospital thromboprophylaxis continued for at least 6 days or until discharge, and he should be considered for extended thromboprophylaxis if the risk of bleeding is not elevated (Figure 2).
Criteria for extending prophylaxis. ICU, intensive care unit; ULN, upper limit of normal range.
Criteria for extending prophylaxis. ICU, intensive care unit; ULN, upper limit of normal range.
Primary thromboprophylaxis in ambulatory cancer patients: case 4
A 67-year-old woman with maturity-onset diabetes who is obese presented with jaundice and a “localized” pancreatic cancer. She declines surgery and has a stent inserted. Biopsy reveals adenocarcinoma, and chemotherapy is commenced. Should this patient receive thromboprophylaxis during the active cancer period and chemotherapy?
Mobile patients with active cancer, including those receiving cancer therapies, such as surgery, chemotherapy, and radiotherapy, have an increased risk of VTE over and above the known high risk associated with cancer.3 Guidelines recommend thromboprophylaxis for cancer patients admitted to hospital with acute medical illnesses; however, only some specific high-risk ambulatory active cancer patients are recommended to have prophylaxis.19,29,30 Up until recently, treatment options for thromboprophylaxis for cancer-associated thrombosis (CAT) included low-molecular weight heparin, aspirin, or warfarin dependent on the cancer type and treatment regimen.29 Only in the last year have phase 3 trial data with DOACs been published, and overall, there are still relatively small amounts of data.
One phase 2 trial of apixaban and 2 recent phase 3 trials of rivaroxaban and apixaban for the prevention of CAT demonstrated some evidence of net clinical benefit of DOACs in ambulatory cancer patients receiving chemotherapy.31-33
Apixaban (5, 10, or 15 mg once daily) was compared with placebo in a phase 2 trial of 125 patients with metastatic cancer who were receiving chemotherapy.33 Overall, in the 3 arms, apixaban was associated with a VTE incidence of 1.1% compared with 13.8% in the placebo arm. Two recent clinical trials of DOACs, the Apixaban for the Prevention of Venous Thromboembolism in Cancer Patients (AVERT)31 trial and the A Study to Evaluate the Efficacy and Safety of Rivaroxaban Venous Thromboembolism (VTE) Prophylaxis in Ambulatory Cancer Participants trial,32 assessed patients to be at significant risk or high risk based on a Khorana score of ≥2.34
The AVERT trial was a randomized, phase 3 superiority trial of 574 patients receiving chemotherapy that compared the efficacy and safety of apixaban 2.5 mg twice daily with placebo. The primary outcome was symptomatic or incidental VTE during the 6 months of follow-up. The main safety outcome was major bleeding; other safety outcomes were clinically relevant nonmajor bleeding and survival.31 Gynecological, lymphoma pancreatic, lung, and stomach cancers were the most common tumor types. There was a significant reduction in symptomatic or incidental VTE that occurred in 12 of 288 patients (4.2%) in the apixaban arm and 28 of 275 patients (10.2%) in the placebo arm (Hazard Ration (HR), 0.41; 95% CI, 0.26-0.65; P < .001). The on-treatment analysis showed that VTE occurred in 3 of 288 patients (1.0%) in the apixaban arm and 20 of 275 patients (7.3%) in the placebo arm (HR, 0.14; 95% CI, 0.05-0.42). There was a significant increase in major bleeding, with 10 events (3.5%) in the apixaban arm and 5 events (1.8%) in the placebo arm (HR, 2.00; 95% CI, 1.01-3.95; P = .046). There was no significant increase in clinically relevant nonmajor bleeding, which occurred in 21 of 288 patients (7.3%) and 15 of 275 patients (5.4%; HR, 1.28; 95% CI, 0.89-1.84), respectively. There were no differences in mortality.
The CASSINI trial was a phase 3, randomized, placebo-controlled, superiority study of 841 patients comparing the efficacy and safety of rivaroxaban 10 mg once daily and placebo for primary prophylaxis of VTE in ambulatory cancer due to receive systemic cancer therapy for up to 6 months.32 At screening and during the trial, lower-extremity ultrasounds were performed every 8 weeks. The primary efficacy outcome was VTE defined as the composite of symptomatic or asymptomatic proximal DVT, symptomatic upper-extremity or distal DVT, symptomatic or incidental PE, and VTE-related death. The principal safety end point was major bleeding. VTE occurred in 25 of 420 patients (6.0%) in the rivaroxaban arm compared with 37 of 421 patients (8.8%) in the placebo arm (HR, 0.66; 95% CI, 0.40-1.09; P = .10). In the on-treatment analysis, VTE occurred in 11 of 420 patients (2.6%) in the rivaroxaban arm compared with 27 of 421 patients (6.4%) in the placebo arm (HR, 0.40; 95% CI, 0.20-0.80). Overall, 8 of 405 patients (2.0%) and 4 of 404 patients (1.0%) in the rivaroxaban and placebo groups, respectively, had a major bleeding event (HR, 1.96; 95% CI, 0.59-6.49; P = .26). No differences were seen in nonmajor clinically relevant bleeding and mortality.
The findings of the DOAC trials are in keeping with the earlier trials of LMWH in mixed cancer populations. Important risk reduction was observed in the AVERT trial and the CASSINI trial, and absolute reductions were higher in the DOAC studies (2.8% for the CASSINI trial [NNT 36] and 6.3% for the AVERT trial [NNT 16] compared with 2.2% for SAVE-ONCO [the SAVE-ONCO study investigated semuloparin vs placebo for VTE prevention in cancer patients receiving chemotherapy] and 1.9% for PROTECHT [a modified Khorana risk assessment score for venous thromboembolism in cancer patients receiving chemotherapy: the Protecht score]). The safety profile of apixaban and rivaroxaban in these trials indicates an increase in major bleeding but low absolute rates of bleeding, with numbers needed to treat of 59 and 100, respectively. Hence, the net clinical benefit may favor the use of DOACs in this setting, with an overall reduction in VTE with the DOACs and a small increase in bleeding without the limitations and restrictions imposed by parenteral therapies, such as LMWH. In these 2 recent thromboprophylaxis trials, much of the bleeding was from epithelial sites, such as the gastrointestinal and genitourinary tracts, consistent with the trials where DOACs were compared with LMWH for the acute and long-term treatment of CAT; hence, the recent ISTH guidance recommends caution in these patients. The question then arises of whether these recommendations may be extrapolated to thromboprophylaxis with the lower doses of DOAC therapy.35
Our patient with pancreatic cancer would likely to have been a suitable candidate for the low-dose DOAC trials and depending on the evolution of guidelines and licensing, may benefit from such therapy. Cancer patients with a high incidence of VTE during active cancer therapy would be suitable candidates for thromboprophylaxis (our decisions are guided by cancer type, cancer treatment, or risk assessment score, such as Khorana score).
Secondary prophylaxis in VTE: case 5
A 54-year-old man with a history of a symptomatic provoked distal DVT 2 years ago after a calf muscle tear presented 6 months ago with a PE after a long-haul flight. He is currently being treated with standard dose of a DOAC. He needs to travel long distances for his work. He has had 2 minimally provoked VTEs. How would you manage him long term?
VTE may be considered a chronic disease in some patients as demonstrated in many epidemiological studies.2,3 Secondary prevention with anticoagulants reduces recurrences and may help to prevent or ameliorate other chronic venous and pulmonary complications.
Baglin et al36 demonstrated that the risk of VTE recurrence is not only clinically significant in patients with unprovoked VTE (19.4% at 2 years) but also, is frequent in those with nonsurgical provoking risk factors (8.8% at 2 years). This group of patients with nonsurgical risk factors and those with minor provoked risk factors both surgical and nonsurgical in nature was often considered to be in clinical equipoise with respect to continuing or stopping anticoagulation. These populations made up the majority of patients who were studied in the extended secondary prevention therapy DOAC trials. Some of these studies tested lower doses of DOACs as preventive therapy in the hope of altering the clinical equipoise in favor of continuing anticoagulation. The background of research demonstrating similar efficacy combined with significantly lower major, intracranial, and fatal bleeding rates seen with higher doses of DOACs compared with conventional parenteral therapy overlapped with VKA9 provided a platform to investigate even lower doses of DOACs in these selected populations. These trials were performed on the background of lower-intensity warfarin not proving to be efficacious in preventing VTE recurrences.37
The DOACs that have been developed for the acute treatment and secondary prevention of VTE (DVT or PE) include rivaroxaban, apixaban, dabigatran, and edoxaban. However, only 2 DOACs, apixaban and rivaroxaban, have been investigated for long-term secondary prevention of VTE comparing standard and low doses. The Apixaban after the Initial Management of Pulmonary Embolism and Deep Vein Thrombosis with First-Line Therapy–Extended Treatment (AMPLIFY-EXT) study7 compared 2 doses of apixaban (5 mg twice daily and 2.5 mg twice daily) with placebo, and the Reduced-dosed Rivaroxaban in the Long-term Prevention of Recurrent Symptomatic Venous Thromboembolism (EINSTEIN CHOICE) trial8 compared 2 doses of rivaroxaban (20 mg once daily and 10 mg once daily) vs aspirin 100 mg. Both of these DOACs can be used as single-drug regimens after an intensified dosing regimen for the acute-phase treatment.
Both trials demonstrated significant proportions of patients in the control arm who had recurrent VTE: 8.8% in the placebo arm of the AMPLIFY Extension study and 4.4% in the aspirin arm of the EINSTEIN Choice study. Both also demonstrated significant reductions in VTE recurrences compared with the comparators: apixaban 2.5 mg twice daily vs placebo 0.19 (0.11-0.33), apixaban 5 mg twice daily vs placebo 0.20 (0.11-0.34), rivaroxaban 20 mg once daily (od) vs aspirin 100 mg 0.34 (0.20-0.59), and rivaroxaban 10 mg od vs aspirin 100 mg 0.26 (0.14-0.47). Neither trial showed significantly increased clinically relevant bleeding compared with the comparator: apixaban 2.5 mg twice daily vs placebo 1.20 (0.69-2.10), apixaban 5 mg twice daily vs placebo 1.62 (0.96-2.73), rivaroxaban 20 mg od vs aspirin 100 mg 1.59 (0.94-2.69), and rivaroxaban 10 mg od vs aspirin 100 mg 1.16 (0.67-2.03)
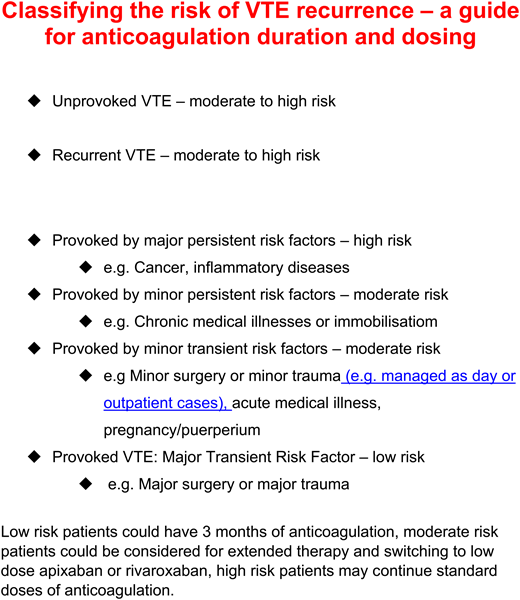
On the basis of these studies and epidemiological data examining risk, the classification of VTE recurrence risk has been updated from the previous crude classification of “provoked or unprovoked” as shown in Figure 3. It is the moderate-risk patients, like the man described in the case above, that are probably most suitable for long-term low-dose DOAC secondary prevention after a period of standard-dose therapy (Figure 3).
Classifying the risk of VTE recurrence—a guide for anticoagulation duration and dosing.
Classifying the risk of VTE recurrence—a guide for anticoagulation duration and dosing.
The duration of anticoagulant therapy should be made after careful assessment of the risks of recurrent VTE and bleeding.6 Decisions regarding dosing for apixaban and rivaroxaban should also consider these factors. For apixaban, the dose is usually reduced at 3 to 6 months; however, this decision can be tempered by the risk profile of the patient. For rivaroxaban, the dose can be maintained or reduced after assessment. The apixaban 2.5 mg twice daily dose was selected based on the findings of the AMPLIFY Extension trial. The dose of rivaroxaban is based on the results from EINSTEIN Choice trial. Patients enrolled in these trials were at clinical equipoise regarding the need for extended therapy, such as the case that we describe.
Patients with an indication for long-term anticoagulants at higher intensity or those with high risk of recurrence, such as those with multiple events of unprovoked VTE, antiphospholipid syndrome and rarer strong thrombophilias, and active cancer, were generally excluded from the AMPLIFY Extension trial and the EINSTEIN Choice trial. Thus, they are not suitable candidates for low-dose anticoagulants. The use of low-dose DOACs should be cautioned in obese patients, because the pharmacokinetics and pharmacodynamics in this population is unknown. Despite the evidence, some patients may opt for other therapies, such as aspirin or continuing VKAs
In summary, lower doses of the DOAC apixaban or rivaroxaban are indicated in many patients except when the risk of recurrent DVT or PE is high: for example, in patients with active prothrombotic diseases or who develop recurrent DVT or PE therapy. Both the opening case and the case described in this section would most likely be considered for long-term low-dose DOAC secondary thromboprophylaxis.
Primary and secondary prophylaxis in arterial disease
Patients with stable cardiovascular disease, those undergoing percutaneous coronary intervention with atrial fibrillation requiring stroke prevention, and those with embolic stroke of undetermined source have been studied with lower doses of DOACs. In this section, we only cover the former indication.
Patients with peripheral artery disease (PAD)38 and coronary artery disease (CAD)39 are at risk of major cardiovascular outcomes throughout their lives. The concept of stable vascular disease has been challenged by the Cardiovascular Outcomes for People Using Anticoagulation Strategies (COMPASS) trial megatrial.40 The polyvascular nature of atherosclerosis results in patients with disease in 1 vascular bed being at risk of new events in other vascular beds. Vascular disease is multifactorial, and both platelets and coagulation play important roles.
Low-dose rivaroxaban 2.5 mg twice daily in combination with aspirin 100 mg and rivaroxaban 5 mg twice daily alone were compared with the standard of care aspirin alone in a population of patients with well-managed vascular disease. In patients with “stable” atherosclerotic vascular disease, those assigned to rivaroxaban 2.5 mg twice daily plus aspirin had better cardiovascular outcomes, reduced all-cause mortality (HR, 0.82; 95% CI, 0.71-0.96), and more major bleeding events than those assigned to aspirin alone. There was no significant difference in intracranial or fatal bleeding between these 2 groups.40 In the PAD and CAD patients, the combination of rivaroxaban plus aspirin compared with aspirin alone reduced the composite end point of cardiovascular death, myocardial infarction, or stroke. The reductions in stroke were a driver of the composite outcome. In the PAD arm, major adverse limb events, including major amputations, were reduced (32 [1%] vs 60 [2%]; HR, 0.54; 95% CI, 0.35-0.82; P = .0037).38,39
Discussion
Improvement in outcomes related to all-cause mortality is the ultimate measure of net clinical benefit. The COMPASS trial demonstrated this outcome in the arm that received low-dose rivaroxaban and aspirin. However, further optimizing the benefit by selecting the patients at the highest risk of cardiovascular events and the lowest risk of bleeding is a current priority for clinicians who manage patients with atherosclerotic arterial disease. The reductions in stroke were particularly clinically important in both PAD and CAD patients in this trial. The introduction of a new regimen to manage PAD patients and reduce major adverse limb events is a welcome addition to an indication that previously had little evidence-based therapeutic options.
Conclusion
Low-dose DOAC therapy as prophylaxis has numerous varied indications for both venous and arterial thrombosis. Patient selection as described above is the key to maximizing benefits and minimizing risks.
Correspondence
Beverley J. Hunt, The Thrombosis & Haemophilia Centre, St. Thomas’ Hospital, Westminster Bridge Rd, London SE1 7EF, United Kingdom; e-mail: beverley.hunt@gstt.nhs.uk.
References
Competing Interests
Conflict-of-interest disclosure: Both A.T.C. and B.J.H. have advised the UK Government Health Select Committee, the all-party working group on thrombosis, the Department of Health, and the National Health Service on the prevention of venous thromboembolism (VTE). A.T.C. is also an advisor to Thrombosis UK and the founder of the European educational charity the Coalition to Prevent Venous Thromboembolism. B.J.H. is Medical Director of Thrombosis UK and Chair of the Steering Committee for World Thrombosis Day. She is also Honorary President of VTE Ireland. She takes no fees in any form from pharmaceutical companies producing currently used anticoagulants. A.T.C. received consulting fees from AbbVie, ACI Clinical, Aspen, Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Boston Scientific, CSL Behring, Daiichi-Sankyo, GlaxoSmithKline, GLG, Guidepoint Global, Johnson and Johnson, Leo Pharma, Medscape, McKinsey, Navigant, ONO, Pfizer, Portola, Sanofi, Takeda, Temasek Capital, and TRN; has advisory board membership with Bayer, Bristol-Myers Squibb, Daiichi-Sankyo, Johnson and Johnson, ONO, Pfizer, Portola, and Sanofi; and received payments for lectures, including speakers bureau services, payments for preparation of reports, and payment for development of educational presentations from Aspen, Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi, GlaxoSmithKline, Johnson and Johnson, Medscape, Pfizer, and Portola.
Author notes
Off-label drug use: None disclosed.

![Clinical events in extended thromboprophylaxis trials investigating both symptomatic and asymptomatic VTE. ADOPT, Apixaban Dosing to Optimize Protection from Thrombosis; APEX, The Acute Medically Ill VTE (Venous Thromboembolism) Prevention with Extended Duration Betrixaban; EXCLAIM, Extended Prophylaxis for Venous Thromboembolism in Acutely Ill Medical Patients with Prolonged Immobilization trial; MAGELLAN, Venous Thromboembolic Event [VTE] Prophylaxis in Medically Ill Patients.](https://ash.silverchair-cdn.com/ash/content_public/journal/hematology/2019/1/10.1182_hematology.2019000026/5/m_hem2019000026cf1.png?Expires=1763556305&Signature=VcKxuV-zRVU2vah2uLhvW2Uwzedvec~Ism86PNRBJT4By2tzZuaYcnpAZQho-Os~DcF0I~S-LOS1C35PW9110GP98UMhtjZsBPPx81e3d3E5-He444VMcdEY5ezKkHY02JN8td1Uv6zRbhDniIp4rpBvUsit9f8MY7Fijx4F-ShfI3ddXLAxTiIPw7lqIufHV3lrd9qyzC4VvTGhcewFJTDlPaS6I1gzfxjuzmG3zwL3b-fM5y4At~vkOA8Ctr5DhfaDgo0S~nm11Q~VCxgIIV~HRdVwlMzpnt3rPHUtuMdJup8ZNh-TLcR878fCEjDoKVa14gg8PfYSBUo6YsKb8Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)