Abstract
Traditionally, the athlete who requires long-term anticoagulation has been told to forgo participation in contact and collision sports. However, a strategy of short-term interruption of anticoagulant therapy may be designed for some athletes, allowing them return to full athletic activity. A personalized pharmacokinetic/pharmacodynamic study of a direct oral anticoagulant (DOAC) may allow athletic participation when plasma drug concentration is minimal and resumption of treatment after the risk of bleeding sufficiently normalizes. Scientific data and uncertainties regarding this approach, as well as practical challenges in the implementation, will be discussed.
Learning Objectives
Appreciate the concept of temporary interruption of anticoagulant therapy for athletes on long-term anticoagulation who want to participate in contact or collision sports
Understand how an individualized pharmacokinetic/pharmacodynamic study of a DOAC can lead to the development of a personalized strategy of temporary anticoagulation interruption
Be cognizant of the many challenges and unresolved issues associated with such an individualized anticoagulant therapy strategy
Background
When athletes develop venous thromboembolism (VTE) and require anticoagulation therapy, they have traditionally been told to refrain from participation in contact and collision sports.1 Although temporary inability to participate in sports may be manageable for the athlete who requires only short-term anticoagulation, indefinite removal from play for the athlete who has an indication for long-term anticoagulation can end an athlete’s career, with potentially impactful psychological and financial consequences. An alternative management approach of short-term intermittent interruption of anticoagulation that takes advantage of the “fast on/fast off” characteristics of the direct oral anticoagulants (DOACs) has, therefore, recently been described for the athlete on long-term anticoagulation.2 The proposed management strategy is time- and resource-intense and, thus, more suitable for the elite or professional athlete engaged in contact and collision sports, rather than the hobby athlete. No definition exists as to what constitutes an “elite athlete,” but for the purpose of this article we define the term as indicating an “athlete who competes at, or trains with realistic aspirations of competing at the highest level of his/her sport and/or for significant monetary or other valuable prizes.”
How long to anticoagulate?
The decision of how long to treat the athlete who has VTE with anticoagulation is based on the same 3 components as in the nonathlete: (1) risk of recurrent VTE, (2) risk for major bleeding, and (3) personal preference. Evidence-based guidelines on length of anticoagulation in patients with VTE exist and are the first starting point for decision-making in athletes as well.3 Three months of full-dose uninterrupted anticoagulation is considered appropriate for the “active treatment” of VTE, as the risk of recurrent VTE is highest during this period of time if no anticoagulation is given.4 The athlete with a VTE due to a major transient risk factor can then discontinue anticoagulation, with a plan for good VTE prophylaxis in future risk situations, such as travel, bone fractures requiring limb immobilization, surgery, etc. The patient with unprovoked proximal deep vein thrombosis (DVT) or pulmonary embolism (PE), with recurrent unprovoked VTE, or with strong persistent VTE risk factors, may be considered for long-term anticoagulation based on the existing general VTE treatment guidelines.3 However, given an athlete’s personal preference, long-term uninterrupted anticoagulant therapy may not be an acceptable, good choice.
Patient values and preferences
Patient values and preferences regarding anticoagulant therapy are highly variable.5-7 This fact is acknowledged in existing anticoagulation guidelines and has become an important part of the decision-making regarding how long and in what manner (ie, continuously or intermittently) to treat a patient with VTE.5,6 Furthermore, patients differ in their acceptance of risk, whether of recurrent VTE or of bleeding. Athletes engaged in contact and collision sports already show a higher acceptance of risk simply by the fact that they engage in such sports. For decision-making in respect to VTE management, the core ethical principle of patient autonomy mandates that patients be afforded input into their management, including their willingness to accept risk, of recurrent VTE or bleeding, when reasonable treatment options exist.
Traditional management
In the patient deemed to be a candidate for long-term anticoagulation, prior reliance on vitamin K antagonists made temporary interruption of anticoagulant therapy for short periods of time impossible, given their long anticoagulant action. Availability of shorter-acting anticoagulants, low-molecular-weight heparins (LMWHs) and DOACs with their “fast on/fast off” characteristics, have opened the possibility of intermittent anticoagulation therapy, with discontinuation of drug some time before the athletic activities that put the athlete at risk for increased bleeding, and resumption immediately afterward if no significant trauma occurred.2
Individualized pharmacokinetic/pharmacodynamic study
Risk of recurrent VTE with anticoagulation interruption
If a management strategy is being considered for intermittently interrupted anticoagulation after the initial 3 months of full-dose uninterrupted treatment, an assessment of risk for recurrent VTE during the time off anticoagulation is helpful for the discussion. As it is typically the patient with a history of unprovoked proximal DVT or PE in whom long-term anticoagulation is considered, the following data and calculations are referring to patients with a history of unprovoked VTE. Patients with unprovoked VTE who discontinue anticoagulation after 3 months have a 10.4% rate of recurrent VTE over the following 6 months.8 Fatal recurrent VTE occurs at a rate of 0.3/100 patient-years for patients who discontinue anticoagulation after the acute treatment.9 From this data, we can estimate a risk of recurrent VTE of <1/3500 per day and risk for fatal VTE of <1/100 000 per day for athletes no longer on anticoagulation after completing initial therapy, indicating that absolute risk for adverse thrombotic outcomes during intermittent interruption is very low.
Definition of “safe” DOAC drug level
When designing an intermittent anticoagulation strategy, a key question is: when prior to athletic participation in collision or contact activity should the DOAC be discontinued so that the risk for bleeding is not significantly higher than for an athlete engaged in the same activities who is not on an anticoagulant? Although it has been shown that trough plasma DOAC levels, at least of dabigatran and edoxaban, correlate with bleeding and thrombotic complications,10-12 it is not known at what DOAC blood level the major bleeding risk is similar to that of a control population, particularly in individuals suffering trauma. Thus, it is not known what an acceptable, “safe” plasma drug level (as measured by mass spectrometry) or drug activity level (as measured by a functional assay, such as anti-factor Xa activity or thrombin generation assays) is. In addition, it is not known whether plasma DOAC drug levels or functional coagulation assays would be better surrogate measures of the safety of a DOAC.
Furthermore, if thrombin inhibition assay results were to be used as measures of bleeding risk, it is not known which of an assays’ parameters (peak thrombin inhibition, area under the curve, or lag time) might be better surrogate measures for clinical bleeding risk.
Given the lack of scientific data as to what drug level or activity is relatively safe and does not significantly increase major bleeding risk, the determination as to what may constitute a safe DOAC drug level is currently empiric and one of expert opinion.
The ongoing PAUSE trial of perioperative DOAC interruption may provide indirect evidence as to what blood DOAC level may be safe in case of (surgical) trauma. The study is not only assessing perioperative bleeding and thrombosis rates, but will also correlate DOAC drug levels with the occurrence of bleeding and thrombotic events.13
Rivaroxaban
The peak (Cmax) rivaroxaban plasma drug level after oral intake of 20 mg once daily in healthy male volunteers is around 173 ng/mL, with wide interindividual differences in drug levels (111- 294 ng/mL); drug half-life (t1/2) is 5.2 to 14.3 hours (Table 1).14 For 10-mg once-daily rivaroxaban, the Cmax has been reported to be ∼141 ng/mL, with a range of 112 to 184 ng/mL and a t1/2 of 4.4 to 32 hours.14 Other pharmacokinetic (PK)/pharmacodynamic (PD) studies of 10-mg rivaroxaban once daily in young healthy men and women have shown Cmax of ∼219 ng/mL and t1/2 of 6.9 to 11.7 hours.15 Trough rivaroxaban levels at 24 hours (Ctrough) in healthy volunteers are difficult to glean from the published literature, as they are often not mentioned in the publications,14,15 but values from patient populations have reported Ctrough at ∼9.1 (1.3-37.6) ng/mL for 10-mg once-daily dosing, and 22.3 (4.3-95.7) ng/mL for 20-mg once-daily dosing.16 All of these data show relatively wide interindividual variability in the various PK values, arguing, as outlined in “The need for an individualized PK/PD study,” for the need of a personalized PK/PD study in an individual rather than the use of published ranges, to be able to work with athlete-specific PK/PD data when developing drug interruption timeline parameters.16
Summary of published PK/PD data of rivaroxaban and apixaban
| Drug and dosing . | Cmax . | Cmin* . | t1/2 hours . | Reference . | “Safe residual level” to engage in contact sports† . | |
|---|---|---|---|---|---|---|
| ng/mL (range) . | ||||||
| Rivaroxaban | 20 mg once daily | 173 (111-294) | 22.3 (4.3-95.7) | 5.2-14.3 | 14 | Unknown; proposal in this manuscript: <30 ng/mL |
| 10 mg once daily | 141 (112-184) | 9.1 (1.3-37.6) | 4.4-32 | 14 | ||
| Apixaban‡ | 5 mg twice daily | 129 | 50 | 11.7 | 18 | Unknown; proposal in this manuscript: <30 ng/mL |
| 2.5 mg twice daily | 62 | 21 | 8.1 | 18 | ||
| Drug and dosing . | Cmax . | Cmin* . | t1/2 hours . | Reference . | “Safe residual level” to engage in contact sports† . | |
|---|---|---|---|---|---|---|
| ng/mL (range) . | ||||||
| Rivaroxaban | 20 mg once daily | 173 (111-294) | 22.3 (4.3-95.7) | 5.2-14.3 | 14 | Unknown; proposal in this manuscript: <30 ng/mL |
| 10 mg once daily | 141 (112-184) | 9.1 (1.3-37.6) | 4.4-32 | 14 | ||
| Apixaban‡ | 5 mg twice daily | 129 | 50 | 11.7 | 18 | Unknown; proposal in this manuscript: <30 ng/mL |
| 2.5 mg twice daily | 62 | 21 | 8.1 | 18 | ||
Data are derived from healthy young volunteers studies, except Cmin values for rivaroxaban.
Cmin values for rivaroxaban are derived from atrial fibrillation patient populations.
Given the lack of scientific data as to what drug level or activity is relatively safe and does not significantly increase major bleeding risk with or without trauma, the determination as to what may constitute a safe DOAC drug level to participate in contact and collision sports is currently empiric and one of expert opinion. The value listed is the authors’ current postulate.
No ranges of values provided in referenced publications; however, wide interindividual ranges for the various PK/PD parameters exist for both apixaban and rivaroxaban.
It is noteworthy that in thrombin-generation assays, various parameters of thrombin generation (endogenous thrombin potential, peak thrombin generation, thrombin-generation lag time) remain abnormal for >24 hours and up to 60 hours after drug intake cessation.17 However, the clinical implication of this finding in respect to bleeding risk is not known.
Given the conglomerate of rivaroxaban’s PK/PD literature that is familiar to us, we put forward that a residual rivaroxaban level of <30 ng/mL may be a potentially safe level to target for the athlete engaged in collision and contact activities. In healthy individuals taking 20-mg once-daily rivaroxaban, plasma drug levels of <50 ng/mL and <30 ng/mL are expected to be reached at ∼13 hours and 17 hours, respectively, after last drug intake,17 but timing, obviously, depends on the drug’s Cmax in an individual person, as well as that person’s t1/2. Drug levels of <50 ng/mL and <30 ng/mL in the person taking 10-mg once daily may be reached 10 hours and 13 hours, respectively, after drug intake.
Apixaban
The typical Cmax plasma drug levels at steady state in healthy volunteers after intake of 5 mg twice daily or 2.5 mg twice daily are 129 ng/mL and 62 ng/mL, respectively; the typical 12-hour trough levels (Cmin) for these doses are 50 ng/mL and 21 ng/mL, respectively, and the typical drug half-life 11.7 hours and 8.1 hours, respectively (Table 1).18 The PD effect of apixaban, as measured by thrombin-inhibition assays, shows less-pronounced thrombin inhibition and a faster return to normal, that is, baseline, after cessation of apixaban intake than observed with rivaroxaban.17 Given that limited PK/PD data on apixaban have been published in the peer-reviewed literature, and that the authors of the current article are less familiar with the PK/PD of apixaban, we do not feel confident at this time to put forward a postulate of a safe apixaban level for the athlete engaged in contact and collision sports, but wonder whether it may be in the order of <30 ng/mL.
The need for an individualized PK/PD study
It is well established that patients taking DOACs have large interindividual differences in plasma drug levels and half-lives.10,19,20 Using published peak and trough plasma drug level or drug half-life ranges will, therefore, only lead to a rough estimate as to when a certain drug level is reached in an individual patient, with little confidence that the values apply to an individual.20 A more accurate assessment can be achieved with an individualized PK/PD study.
Which DOAC drug is most suitable to be used?
Which DOAC drug would be best to use if one pursued an intermittent dosing strategy in the long-term management of an athlete? Given the many unanswered questions, such as which drug level or activity level is a safe level, the best drug to use and investigate for an individual PK/PD study may be the one most familiar to the physicians looking after the athlete. Availability of an intermediate dosing regimen (as with apixaban and rivaroxaban) and availability of reversal agents in case of major bleeding are other considerations. A recent publication shows that 20-mg once-daily rivaroxaban compared with 5-mg twice-daily apixaban leads to more prolonged thrombin inhibition once the DOAC is stopped.17 This may be of relevance for the athlete who plans to use intermittent dosing to minimize the risk for bleeding with contact or collision sports, as it suggests that the shorter-acting apixaban may be a better choice for intermittent anticoagulation dosing. However, at this point, it is not known whether any parameters of thrombin-generation inhibition assays correlate with clinical bleeding, particularly bleeding caused by trauma. In addition, an investigation directly comparing 10-mg once-daily rivaroxaban with 2.5-mg twice-daily apixaban on thrombin inhibition would be helpful, but has, to our knowledge, not been performed.
Timing of blood draws for PK/PD study
What should be the timing of blood draws after oral DOAC intake in the individualized PK/PD study? Given the wide interindividual differences in peak plasma drug levels (Cmax) reached, drug half-lives, and time to reach low DOAC drug levels that could be considered as being safe, blood collection at 8, 12, 16, and 20 hours may be appropriate in a first PK/PD study. Timing of blood tests may have to be adjusted to some degree on availability of phlebotomy and blood-processing services. More focused testing, to determine more exactly when the postulated safe drug level is reached, could then be done based on these initial results in a second abbreviated PK/PD study with testing at only 2 time points. Consideration can also be given to blood collection at specific times simulating the athlete’s anticipated practice and competition schedules, if known. Repeating a PK/PD study to confirm the initially determined safe residual level may be best in any case, as intraindividual DOAC drug fluctuations may occur, as has been reported for dabigatran (but not investigated for the other DOACs).21
Specifics regarding blood draws and DOAC drug-level testing
Before pursuing an individualized PK/PD study, a number of blood collection and testing issues need to be clarified: (1) which laboratory to send the blood to, (2) what tubes to use for the blood collection (citrate, EDTA, or heparin tubes), (3) what method the laboratory uses for determination of blood DOAC activity (mass spectrometry drug-level testing or functional coagulation testing), (4) what lower limit of detection of DOAC drug level or activity the laboratory’s assay has, (5) whether the blood needs to be centrifuged and plasma or serum separated and, if yes, what the time frame for separation/processing is, and (6) whether the blood, plasma, or serum needs to be refrigerated.
Stopping anticoagulation before play
Based on the information gained from the personalized PK/PD study, it can be calculated how many hours after DOAC drug intake the empiric safe (ie, maximally acceptable) blood drug level is reached. A DOAC drug intake schedule can, thus, be created for the individual athlete: the last DOAC intake should be remote enough from the game or practice during which significant contact/collision might occur that the drug level will have decreased below the “safe” blood level. Depending on the athlete’s DOAC PK characteristics (drug levels, drug half-life, and time to reach the “safe” blood drug level) and the athlete’s type of athletic activity and practice and game schedule (frequency and times), the creation of an individualized treatment plan may or may not be feasible for an athlete.
Restarting anticoagulation after play
Restarting anticoagulation after an uncomplicated sporting event within 1 to 2 hours is likely safe. However, if trauma occurred, then a delay in the reinitiation of anticoagulation may be necessary to avoid or minimize posttraumatic bleeding risk. The decision of when to restart anticoagulation needs to be made on a case-by-case basis, with expert guidance after careful consideration of the specific circumstances of the trauma.
Which athlete is suitable for intermittent anticoagulation dosing?
An intermittent anticoagulant treatment strategy is not suitable for every athlete who has a medical indication for long-term anticoagulation. For athletes engaged in sports that require significant, severe contact and risk for trauma with every game and practice several times per week (like American football), an intermittent anticoagulation strategy may not be feasible, as reinitiation of anticoagulation after games and practices would likely frequently be delayed due to incurred trauma. A discussion needs to be had within and between the sports medicine and hematology health care professional communities as to which athlete on long-term anticoagulation may be suitable for an intermittent anticoagulation strategy.
Implementation
The decision to pursue an intermittent anticoagulant strategy with an athlete is not simply a decision that is made within the typical patient-physician relationship. Other entities are involved in the final decision-making and implementation of a treatment strategy, and a variety of issues need to be addressed. What role do the player’s school, employer, and/or union have in the decision process? What is the comfort level of the athletic trainer and team physician having an athlete on such intermittent dosing regimen? How and by whom is the decision best made when to restart the anticoagulant after a game? For which practice drills and scrimmages does the athlete need to be off anticoagulation, and which ones does the athlete need to avoid participating in? How transparent should one be with the public and media about the athlete’s health issue?
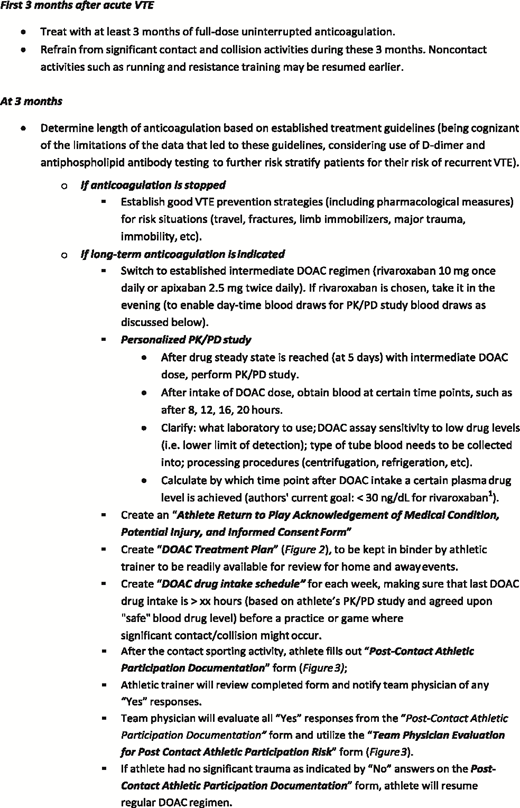
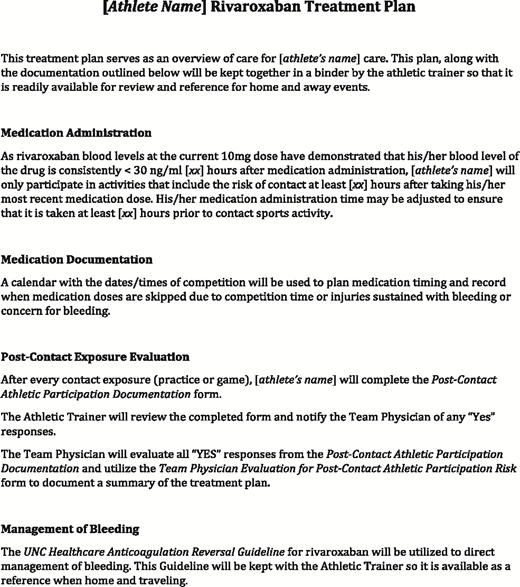
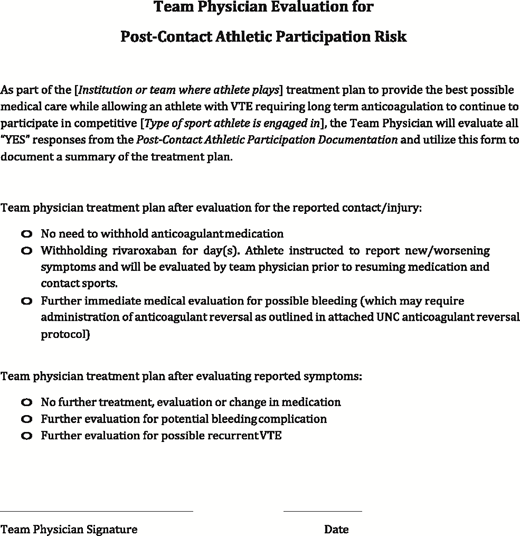
Figure 1 summaries the steps in the management of the athlete with VTE, the performance of a personalized PK/PD study, and the practical implementation steps leading to a structured management strategy. An extensive “Athlete Return to Play Acknowledgment of Medical Condition, Potential Injury, and Informed Consent Form” has not been added to this manuscript given its length, but other forms used in our “return to play” strategy are included as Figures 2-4.
Proposed approach to selected elite athletes with VTE (proximal DVT and/or PE).
Proposed approach to selected elite athletes with VTE (proximal DVT and/or PE).
The public, the media
Facts and details of the circumstances of any thrombotic event are needed to understand risks to a patient. A meaningful discussion about whether an athlete can safely return to sports cannot be had without a full understanding of the athlete’s medical history and current situation. That medical information is rarely available for public consideration. This lack of information can breed hyperbole in the media. Phrases like “life-threatening blood clots” or “playing sports while on blood thinners can be fatal” are attention grabbing, but lead to generalizations about risk and treatment that may not apply to the athlete’s specific circumstances. A fact-based public discussion about VTE, anticoagulation, and risks is needed, so that individualized solutions, such as an intermittent anticoagulation strategy, can be developed, applied to, and used by suitable athletes whose careers would otherwise be terminated by having an indication for long-term anticoagulation.
Unanswered questions, caveats, future research
At this point, a number of questions about the interpretation of individualized PK/PD studies and their application to clinical practice are unanswered. A few of them are as follows:
At this point, it is not known which assays, plasma drug levels, or DOAC activity levels (anti-Xa levels, thrombin-inhibition assays, etc) are best surrogates to assess the safety of residual circulating DOAC levels and effects, and what the threshold value of these values is, below which the risk for bleeding is not significantly increased, should the athlete suffer trauma.
As significant intraindividual drug-level variability has been observed with dabigatran,21 it needs to be determined whether that is also the case with apixaban and rivaroxaban, as well as whether repeat PK/PD testing may be advisable to confirm initially found values.
The influence of strenuous exercise and activity on DOAC PK/PD parameters needs to be investigated to see whether values change depending on an athlete’s activity level.
Different PK/PD results are found depending on whether a PK/PD study is done after the morning or the evening intake of apixaban: PK/PD values obtained after the evening dose show lower peak and higher trough plasma level.17 This is presumably due to circadian variations in gastrointestinal function, hepatic and intestinal enzyme activity, and organ blood flow. This needs to be considered when interpreting PK/PD values.
The proposed individual PK/PD study and dosing strategy is, in our opinion, not suitable to be widely used, given the many questions that remain open and unanswered and the intensity of resources needed to come up with an individualized testing and management strategy. A coordinated effort with development of research studies is needed to create data that will give us more confidence that an individualized treatment strategy is safe and effective.
Summary
Although the proposed strategy is supported by scientific principle and clinical reasoning, a number of open questions remain. Studies will need to be performed that assess safety and feasibility of the proposed strategy and lead to further optimization of this management approach. A prospective registry of athletes treated with the proposed intermittent treatment strategy would be an appropriate next step, assessing clinical outcomes, acceptability of the strategy to the patient and other involved stakeholders, and hurdles in implementation and feasibility. Further discussion and research needs to turn more of the gray, empiric areas in this concept into clear and evidence-based black-and-white areas, so that we have increased confidence when developing and implementing such an intermittent anticoagulation strategy.
Correspondence
Stephan Moll, Division of Hematology-Oncology, University of North Carolina School of Medicine, CB 7035, Chapel Hill, NC 27599; e-mail: smoll@med.unc.edu.
References
Competing Interests
Conflict-of-interest disclosure: S.M. has consulted for Portola, Stago, and Janssen. J.N.B. and C.W.M. declare no competing financial interests.
Author notes
Off-label drug use: None disclosed.