Abstract
This educational review addresses the diagnostic evaluation of patients for autoimmune and other forms of acquired neutropenia, including the futility of deconstructing the overlap of chronic “autoimmune,” “benign,” and “idiopathic” categories. Isolated neutropenias caused by infection, drugs, and immunologic disorders are also addressed. Discussion of management options emphasizes a conservative approach, with largely supportive care for these mostly benign and self-limited disorders.
Learning Objectives
Know how to evaluate patients for autoimmune and other forms of acquired neutropenia
Know how to manage patients with autoimmune and other forms of acquired neutropenia
Neutropenia, in both children and adults, encompasses a range of absolute neutrophil count (ANC) <1500 cells/μL, but is usually not clinically significant unless the ANC is <500.1,2 A high risk of severe or opportunistic infections is associated with ANC <200 (also termed agranulocytosis). However, these principles are most applicable to hypoproductive neutropenias caused by bone marrow suppression or failure; patients with neutropenia caused by peripheral destruction of mature neutrophils generally fare much better, probably because of a better supply of neutrophils at sites of infection. Thus, patients, especially infants and young children, with autoimmune neutropenia may be entirely asymptomatic with ANC numbers that are quite frightening to families and (often) their physicians. The degree of risk is also related to the duration of neutropenia, with chronic neutropenia associated with a higher likelihood of severe infection than transient processes.1,2
Chronic neutropenia
Congenital neutropenias and bone marrow failure syndromes are addressed in educational reviews by Klein3 and Shimamura4 in this issue.
In children, chronic autoimmune neutropenia and chronic benign (or idiopathic) neutropenia are virtually interchangeable terms because of their common excellent outcomes and the difficulty of distinguishing them diagnostically.5-10 Antineutrophil antibody tests have little or no diagnostic value (discussed in Diagnosis and management). Common characteristics are summarized in Table 1. Neutropenia generally presents in the first year of life (range 2-54 months) and resolves by age 2 to 4 years.8-10 This form of neutropenia, the most common form of chronic neutropenia in childhood, is quite rare, occurring in only ∼1 in 100 000 children per year11 ; however, many cases are probably undetected, because asymptomatic children have no clinical indications for blood counts.
Common features of chronic autoimmune/benign/idiopathic neutropenia of childhood
| Clinical features | Median age of diagnosis is 8-11 months of age (range 3-38 mo) |
| Few and minor infections (mostly upper respiratory) | |
| Occasional gingivitis | |
| Rare serious or invasive infections (eg, pneumonia), usually in young infants | |
| Laboratory features | Median ANC at time of diagnosis ≈200 cells/µL (range 0-500) |
| ANC often rises at times of stress or bacterial infection | |
| Hemoglobin, platelet count generally normal | |
| Bone marrow (if performed) shows normal to increased myelopoiesis, sometimes with a decrease in mature neutrophils | |
| Antineutrophil antibodies sometimes detected but not predictive of course | |
| Therapy | Antibiotics for acute bacterial infection |
| Prophylactic antibiotics (eg, trimethoprim/sulfamethoxazole) may be helpful in some patients with recurrent otitis media, but can exacerbate neutropenia | |
| G-CSF only in the event of serious infection (consider alternative diagnoses!) or to improve quality of life in case of very frequent precautionary emergency department visits or admissions | |
| Prognosis | Recovery in almost all patients (median duration 20 mo, range 6-54 mo) |
| No evident risk of recurrence |
| Clinical features | Median age of diagnosis is 8-11 months of age (range 3-38 mo) |
| Few and minor infections (mostly upper respiratory) | |
| Occasional gingivitis | |
| Rare serious or invasive infections (eg, pneumonia), usually in young infants | |
| Laboratory features | Median ANC at time of diagnosis ≈200 cells/µL (range 0-500) |
| ANC often rises at times of stress or bacterial infection | |
| Hemoglobin, platelet count generally normal | |
| Bone marrow (if performed) shows normal to increased myelopoiesis, sometimes with a decrease in mature neutrophils | |
| Antineutrophil antibodies sometimes detected but not predictive of course | |
| Therapy | Antibiotics for acute bacterial infection |
| Prophylactic antibiotics (eg, trimethoprim/sulfamethoxazole) may be helpful in some patients with recurrent otitis media, but can exacerbate neutropenia | |
| G-CSF only in the event of serious infection (consider alternative diagnoses!) or to improve quality of life in case of very frequent precautionary emergency department visits or admissions | |
| Prognosis | Recovery in almost all patients (median duration 20 mo, range 6-54 mo) |
| No evident risk of recurrence |
Adapted from Dinauer et al1 with permission.
The ANC throughout the course is often very low (<200 to 500 cells/μL), usually with relative or absolute monocytosis and relative eosinophilia. Importantly, the neutrophil count generally rises—often into the mildly neutropenic or even normal range—at times of bacterial infection or stress, although not necessarily with viral infection. This response, which almost certainly contributes to the benign clinical course, also serves as an important diagnostic indicator that the child has an adequate number of bone marrow storage pool neutrophils and rules out hypoproductive defects such as severe congenital neutropenia. It can be mimicked by the glucocorticoid stimulation test,12,13 discussed later.
Other peripheral counts are normal for age. Selective IgA deficiency is more common in these children than in the general population, but is still rare (∼3%).10 Concurrent or asynchronous additional autoimmune cytopenias constitute Evans syndrome, which is generally chronic and highly associated with autoimmune lymphoproliferative syndrome, other autoimmune diseases, and primary or acquired immunodeficiency disorders.14 Additional nonimmune cytopenias may indicate an underlying bone marrow process such as a congenital bone marrow failure syndrome, acquired aplastic anemia, myelodysplastic syndrome, or leukemia.
In adults, chronic autoimmune and idiopathic neutropenias are also highly overlapping and difficult to distinguish, similarly in part because of the lack of reliable antineutrophil antibody tests. Unlike the form in infants, the adult disease is more common in women (∼5:1 female:male ratio) and much more likely to be chronic.2 Although most patients do not have severe infections, those with very low ANCs may have recurrent stomatitis and skin or respiratory infections.
Acquired neutropenia, usually mild and often intermittent, may accompany chronic inflammatory and autoimmune diseases (eg, systemic lupus erythematosus, rheumatoid arthritis, Sjögren syndrome, and sarcoidosis).15 Felty syndrome refers specifically to more severe neutropenia with splenomegaly, in the context of rheumatoid arthritis.16
Isolated chronic neutropenia is a common, often presenting complication of large granular lymphocytic (LGL) leukemia in older adults.16-18 Unlike the multilineage loss of bone marrow production in other forms of leukemia, neutropenia in LGL disease is both autoimmune and cytokine-mediated because of the clonal expansion of lymphocytes with characteristics of activated T or natural killer cells.
Vitamin B12, folic acid, copper, or protein-calorie nutritional deficiencies can cause neutropenia, but nutrition is rarely a consideration in the diagnosis of isolated neutropenia, because deficiencies sufficient to cause chronic neutropenia virtually always cause concurrent anemia, and often cause thrombocytopenia.
Transient neutropenia
Neutropenia lasting fewer than 3 months is common and usually unnoticed in the acute and convalescent stages of viral infections.2,19-21 Almost any virus, or the host response to that virus, can cause transient neutropenia. More profound and long-lasting suppression of the ANC may occur with infection by cytomegalovirus, Epstein-Barr virus, human immunodeficiency virus, influenza viruses, and parvovirus B19. Less commonly, neutropenia may be associated with acute bacterial sepsis, indicating a poor prognosis caused by depletion of the bone marrow storage pool, or with less critical infections caused by a variety of bacteria and protozoa (Table 2).
Partial list of the more prominent causes of transient neutropenia
| Drugs | |
| Anticonvulsant | Carbamazepine, valproate |
| Antimicrobial | Sulfonamides, penicillins, trimethoprim/sulfamethoxazole |
| Antipsychotic | Clozapine, olanzapine, phenothiazines |
| Antirheumatic | Gold, levamisole, penicillamine |
| Antithyroid | Methimazole, propylthiouracil |
| Other | Aminopyrine, deferiprone, rituximab, levamisole (adulterated cocaine) |
| Infections | |
| Viral | CMV, EBV, HIV, influenza, parvovirus B19 |
| Bacterial | Overwhelming sepsis (any organism), Anaplasma, Brucella, Ehrlichia, paratyphoid, Mycobacterium tuberculosis, tularemia, typhoid |
| Protozoan | Plasmodium sp. |
| Antibody | |
| Neonatal isoimmune |
| Drugs | |
| Anticonvulsant | Carbamazepine, valproate |
| Antimicrobial | Sulfonamides, penicillins, trimethoprim/sulfamethoxazole |
| Antipsychotic | Clozapine, olanzapine, phenothiazines |
| Antirheumatic | Gold, levamisole, penicillamine |
| Antithyroid | Methimazole, propylthiouracil |
| Other | Aminopyrine, deferiprone, rituximab, levamisole (adulterated cocaine) |
| Infections | |
| Viral | CMV, EBV, HIV, influenza, parvovirus B19 |
| Bacterial | Overwhelming sepsis (any organism), Anaplasma, Brucella, Ehrlichia, paratyphoid, Mycobacterium tuberculosis, tularemia, typhoid |
| Protozoan | Plasmodium sp. |
| Antibody | |
| Neonatal isoimmune |
CMV, Cytomegalovirus; EBV, Epstein-Barr virus; HIV, human immunodeficiency virus.
Transient neutropenia resulting from drugs (excluding the expected bone marrow suppression associated with cancer chemotherapy) can range from mild, well-tolerated neutropenia with ANC >500 cells/μL to life-threatening agranulocytosis (ANC <200 cells/μL), with high morbidity and as high as 5% mortality,22 mostly associated with advanced age and comorbidities. Single lineage idiosyncratic reactions are more frequent in adults, particularly the elderly, and in females.22 Neutropenia can occur at any point in therapy with almost any drug; those most commonly associated with idiosyncratic neutropenia or agranulocytosis are listed in Table 2. The most common drug classes include anti-inflammatories, particularly aminopyrine and sulfasalazine; antimicrobial agents, particularly trimethoprim/sulfamethoxazole; antithyroid drugs; antipsychotics, most notably clozapine but also any phenothiazine; and others used in hematology practice, including deferiprone and rituximab.
Among immune neutropenias, the only consistently transient form is neonatal neutropenia caused by passive transfer of maternal isoimmune or autoimmune antibodies, which decay along with the rest of maternal immunoglobulin G. Depending on the titer of the antibody, neutropenia can last from several weeks to (rarely) as long as 6 months.23,24 Neonatal immune neutropenia may occur as an incidental finding, or go unnoticed in asymptomatic infants, but can lead to sepsis or localized infections such as omphalitis or pneumonia.
Diagnosis and management
Diagnosis
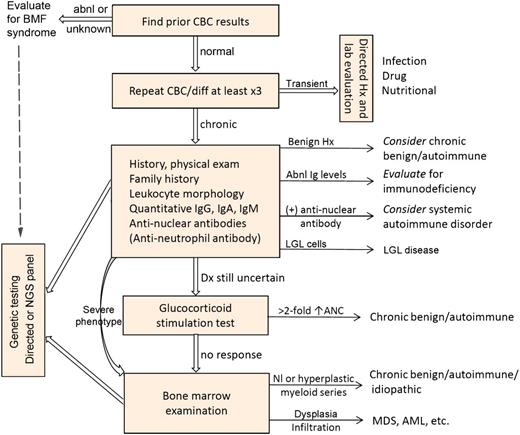
Figure 1 presents an algorithm for diagnosis of acquired neutropenia. Repeated complete blood counts will help rule out laboratory error and allow time for resolution of the most transient and clinically insignificant neutropenia. Other causes of transient neutropenia (which may not be transient until the cause is identified) can be evaluated by directed history and laboratory evaluation. Chronic neutropenia calls for further evaluation as indicated.
Algorithm for the diagnosis of acquired neutropenia. “Anti-neutrophil antibody” is enclosed in parentheses to indicate that the test has limited utility (see text). abnl, abnormal; AML, acute myeloid leukemia; ANC, absolute neutrophil count; BMF, bone marrow failure; CBC, complete blood count; diff, differential count; Dx, diagnosis; Hx, history; Ig, immunoglobulins A, G, and M; LGL, large granular lymphocyte; MDS, myelodysplastic syndrome; NGS, next generation sequencing; Nl, normal; Sx, symptoms. “Severe phenotype” indicates severe, recurrent, or opportunistic infections. Adapted from Dinauer et al1 with permission.
Algorithm for the diagnosis of acquired neutropenia. “Anti-neutrophil antibody” is enclosed in parentheses to indicate that the test has limited utility (see text). abnl, abnormal; AML, acute myeloid leukemia; ANC, absolute neutrophil count; BMF, bone marrow failure; CBC, complete blood count; diff, differential count; Dx, diagnosis; Hx, history; Ig, immunoglobulins A, G, and M; LGL, large granular lymphocyte; MDS, myelodysplastic syndrome; NGS, next generation sequencing; Nl, normal; Sx, symptoms. “Severe phenotype” indicates severe, recurrent, or opportunistic infections. Adapted from Dinauer et al1 with permission.
Antineutrophil antibody measurements have little or no role in the diagnosis, because most tests have high false-negative and false-positive rates,26-28 although specialized testing for antibodies to individual epitopes can be more specific.5,26 Importantly, at least for young children, the presence or absence of detectable antibody does not predict the time to nearly universal resolution.9 A notable exception is neonatal isoimmune neutropenia, in which identification of a specific antibody in maternal serum can confirm the diagnosis suggested by paternal and maternal leukocyte typing.29
Because neutropenia can be a presenting sign of immunodeficiency or a systemic autoimmune disorder, further screening is indicated, particularly in adolescent or young adult women,30 and repeat bone marrow examinations are indicated to evaluate for leukemia or myelodysplasia in adults with worsening neutropenia or additional cytopenias.31 Although there is a broad spectrum of immunologic diseases associated with neutropenia, immunoglobulin screening is usually sufficient unless the phenotype suggests a more serious form of combined immunodeficiency.32 Similarly, screening for systemic autoimmunity should be more extensive in patients with multiple cytopenias, splenomegaly, or clinical features associated with systemic autoimmune or hyperinflammatory conditions.32
Without specific tests, the diagnosis of chronic benign/autoimmune neutropenia is often a matter of exclusion. Congenital neutropenia can be ruled out by identification of an adequate ANC in response to infection (except in neonates), or a twofold or greater rise in ANC after glucocorticoid challenge.12,13 That test demonstrates mobilization of the bone marrow reserve pool of mature neutrophils by determining the ANC before and 4 to 6 hours after a single dose of prednisone (1-2 mg/kg). Alternatively, current next-generation sequencing panels for congenital neutropenia or bone marrow failure can test for congenital neutropenia noninvasively and, in some cases, more accurately than bone marrow examination. Although specific phenotypes may inform single-gene or gene-family sequencing,3 these panels provide an expensive (but actually cost-effective compared with multiple single-gene analyses) means to assess the multiple genes responsible for a wide array of variable phenotypes of congenital neutropenia and bone marrow failure syndromes.4
Bone marrow examination should be used for rapid diagnosis in cases with severe infection, severe stomatitis or recurrent high fever, or with clinical or laboratory findings suggestive of myelodysplastic syndromes or leukemia. Because these conditions are more common in adults than in children, medical hematologists tend to examine the bone marrow more frequently and earlier in evaluations than do pediatric hematologists.
Treatment and precautions
Aggressive management of documented infection in neutropenic patients is a standard of care that requires no further discussion here, except to note that although patients with extreme agranulocytosis are quite susceptible to fever, they may show diminished signs of inflammation at localized sites of infection. Management of fever without known source, prophylaxis, and precautions for acquired neutropenia are not well standardized and have little evidence base or consensus, and so will be discussed in a “How I Treat” format.
Transient neutropenia usually resolves spontaneously or with treatment of the underlying cause. Drug-induced neutropenia usually requires only discontinuation of the offending drug, although that may be hard to identify in patients receiving multiple medications. An exception to the stopping rule may be individuals with schizophrenia who respond only to clozapine, but develop mild neutropenia, with ANCs below the usual threshold for stopping the drug. However, if the neutrophil count is stable in a functionally adequate range (eg, 500-1000 cells/μL), then one must consider the relative risk of developing more severe agranulocytosis vs the known high mortality of inadequately treated schizophrenia,33 or the drug can be restarted with careful monitoring.34 Although granulocyte colony-stimulating factor (G-CSF) is often prescribed for drug-induced agranulocytosis with or without serious infection, and it is theoretically probable that it hastens recovery, there is no evidence of a significant clinical benefit in this setting.
For chronic autoimmune/benign neutropenia, no treatment is usually necessary, because serious infections are very rare in both children and adults with the disorder.5,6,31,35 If increased ANCs can be demonstrated at the times of several febrile illnesses, then subsequent emergency department visits can be limited to episodes when the child appears to be seriously ill. Some children with recurrent otitis media benefit from prophylactic antibiotics, but the best drug, trimethoprim/sulfamethoxazole, can itself be associated with neutropenia. G-CSF (filgrastim) is only very rarely indicated for serious or recurrent invasive infections (which would call into question the diagnosis of “benign” neutropenia), but may provide improved quality of life for families making frequent emergency department visits for febrile illnesses.
Notably, unlike the delayed G-CSF responses observed in severe congenital neutropenia,36 patients with acquired neutropenia, particularly those with adequate bone marrow storage pools of mature neutrophils, show nearly immediate improvement in neutrophil counts. Doses should be started in a low range (eg, 1-2 μg/kg per day), because the rapid, vigorous responses can cause severe bone pain, which needs to be carefully balanced against the therapeutic effect. Also unlike congenital neutropenia patients, those treated with G-CSF for acquired neutropenia are not at risk for development of myelodysplasia or leukemia.
Although many families try to isolate the patient and sterilize their living quarters, simple common-sense precautions are quite sufficient. Measures such as the “neutropenic diet” and use of antibacterial skin cleansers and household disinfectants are both inconvenient and ineffective, and the social and psychological costs of excessive precautions outweigh their questionable benefits. Good dental hygiene is essential, to avoid chronic gingivitis and tooth loss. Very importantly, children should adhere to recommended immunization schedules.
Acknowledgments
Supported by National Institutes of Health, National Institute of Allergy and Infectious Diseases grant R24AI049393-11.
Correspondence
Peter E. Newburger, Departments of Pediatrics and Molecular, Cell, and Cancer Biology, University of Massachusetts Medical School, 55 N Lake Ave, Worcester, MA 01655; e-mail peter.newburger@umassmed.edu.
References
Competing Interests
Conflict-of-interest disclosure: The author declares no competing financial interests.
Author notes
Off-label drug use: None disclosed.