Abstract
The past 15 years have seen major leaps in our understanding of the molecular genetic mutations that act as drivers of acute myeloid leukemia (AML). Clinical trials of agents against specific mutant proteins, such as FLT3-internal tandem duplications (ITDs) and isocitrate dehydrogenase mutations (IDHs) are ongoing. This review discusses agents in clinical trials that target specific gene mutations and/or epigenetic targets.
Learning Objectives
A variety of pharmaceuticals against specific genetic and epigenetic targets are in clinical trials
Clinical trials using these targeted agents show promising early results
The future treatment of AML will likely incorporate novel agents in combination or with chemotherapy
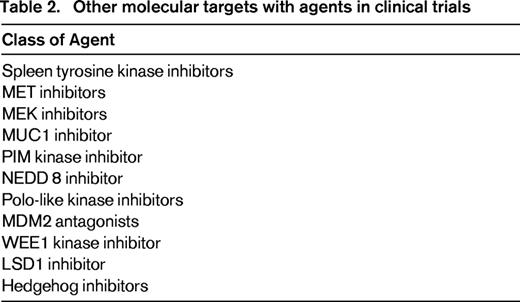
Acute myeloid leukemia (AML) is an acquired disease of chromosomal translocations and somatic mutations, with single or multiple genetic events operating alone or together to produce the phenotype of differentiation block and proliferation at the myeloblast stage of hematopoiesis. The revolution in techniques and the reduction in the costs of next-generation sequencing (NGS) of DNA allows us to examine with extraordinary detail, the contribution of gene mutations to the pathogenesis of newly diagnosed, refractory, and relapsed AML. Techniques, such as CHIP-seq, have given us unprecedented ability to understand the epigenetic state of leukemic myeloblasts. Unlike solid malignancies, patients with AML have relatively few, perhaps 30, common, recurrent, genetic alterations.1,2 The genetic alterations with multiple retrospective studies supporting their prognostic import, NPM1, FLT3, and CEBPA, are incorporated into the current World Health Organization guidelines on the diagnosis of AML.3 Mutations found in genes such as c-KIT, isocitrate dehydrogenase (IDH1 and IDH2) and FLT-3 provide druggable molecular targets in patients with AML that may improve rates of complete remission (CR), disease-free survival (DFS), and overall survival (OS). In addition, inhibitors of proteins involved in regulating the epigenetic state of cells, such as the histone methyltransferase DOT1L and inhibitors of BET proteins show evidence of clinical activity in ongoing phase 1 studies (Table 1).
Response rate in clinical trials of targeted agents for the treatment of AML
Note that response criteria between trials do not necessarily use the international working group criteria and therefore, between trial comparisons are difficult to make.
The therapeutic limitations of our current approach to treating newly diagnosed “fit” patients with AML using induction chemotherapy are well known; multiple international retrospective studies show that only 40% of patients younger than age 60 survive >5 years.4 Indeed, even “favorable risk” core binding factor leukemias have an unacceptably high mortality rate of 40% at 5 years.5 The prognosis for patients who relapse after achieving a CR is dismal and patients older than age 60 fare little better. The de facto pharmacologic options for “unfit” patients, low-dose cytarabine or hypomethylating agents, are modestly effective but inadequate.6,7 The inhibition of molecular genetic pathways in AML is in its infancy, but they provide an early look at how we may use small molecule inhibitors to treat AML in the next few years.
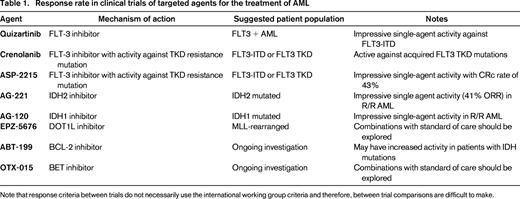
In this brief monograph, I present an overview of the most exciting targeted molecular therapies that are currently in clinical trials and give a roadmap to what the treatment of leukemia may look like 5 years from now. This review is not meant to be exhaustive; the landscape of targets is well known and new drugs available against these targets are introduced frequently. Rather, I focus on therapies that have clinical data available and that I believe may make it into clinical practice as single agents in the next 5 years. Targets not addressed in this review are summarized in Table 2.
FLT-3
FLT3 internal tandem duplications (FLT3-ITDs) are seen in ∼30% of patients with de novo AML. Patients with FLT3-ITD have a poor prognosis.8,9 Given the prevalence of FLT3-ITD and the suboptimal outcomes, the development of inhibitors of mutant FLT3 is seen as a priority in curing patients with FLT3–positive disease. Efforts to target AML with FLT-3-ITD are ongoing. Despite this effort and a number of “first-generation” FLT-3 inhibitors, both those that are used off-label (Sorafenib and Sunitinib) and have been explored in late stage clinical trials (Lestartinib, Midostaurin), the search for a novel inhibitor of FLT-3 that leads to an overall survival benefit compared with chemotherapy continues. Previous ASH education sessions provided a comprehensive review of treating FLT-3–positive disease.10 The state-of-the-art, however, and excitement, revolves around three drugs in clinical trials, Quizartinib, Crenolanib, and ASP-2215.
Quizartinib
Formerly known as AC220, Quizartinib was developed expressly to treat FLT3 mutation-positive AML as a “second-generation” FLT3 inhibitor.11 It is both a highly selective and potent inhibitor of FLT3 mutated AML in vitro and in xenograft models of disease. A phase I study of Quizartinib in patients with relapsed or refractory AML, regardless of FLT3 mutation status, was completed using both intermittent (2 weeks on and 2 weeks off) and continuous dosing in sequential 28 day cycles. The maximum tolerated dose was not reached in the intermittent dosing cohorts and was determined to be 200 mg/day in the continuous dosing cohort.12 A variety of phase II studies have been conducted using Quizartinib in the relapsed and refractory setting (see References).13-15 What is remarkable about all of these studies, whether patients were in first relapse or later, young or old, is the relatively remarkable composite complete remission rate, partial remission rate, and median duration of response. In all of the phase II studies using Quizartinib as a single agent for relapsed/refractory disease the CRc (composite complete remission rate that includes CR, CRi, and CRp) ranged between 44% and 54%, whereas the overall response rate (CRc + PR) was between 61% and 72%. Of crucial importance, the PR definition did not require normalization of platelet and neutrophil counts as defined in the International Working Group Criteria. Median duration of response ranged between 11.3 and 12.7 weeks.
Despite the single-agent activity of Quizartinib, 50% of patients relapse within 3 months. Further studies suggest that the mechanism of resistance to Quizartinib is the development of acquired mutations in the tyrosine kinase domain of the FLT2 gene, including mutations in D835 and F691. Because of this, agents that can overcome this resistance and lead to a longer duration of response are seen as crucial to the development of targeted inhibitors of mutant FLT3.
Crenolanib
The tyrosine kinase inhibitor, Crenolanib, initially developed as an inhibitor of PDGFR, was demonstrated to have activity against mutations in the activation loop of FLT3, the most common being a substitution at amino acid D835.16 As the primary mechanism of resistance to the FLT-3 inhibitor Quizartinib (AC220) is development of TKD mutations in the activation loop, it was hypothesized that Crenolanib would be a pan selective FLT-3 inhibitor that would overcome Quizartinib resistance. A phase II study of Crenolanib in patients with relapsed or refractory AML and a FLT3-ITD or FLT3-TKD was presented at the ASH annual meeting in 2014.17 Crenolanib was administered at a dose of 200 mg/m2/d, 3 times/d in continuous 28 day cycles, and patients were stratified based on whether they had received prior FLT3 directed therapy (eg, Quizartinib, Midostaurin, Sorafenib, PLX3397).
Crenolanib induced a complete remission with incomplete blood count recovery (CRi) in 23% of patients who were FLT3 inhibitor naïve, but in only 5% of patients who had received prior FLT3 therapy. Although both treatment groups had similar degrees of hematologic improvement (31% and 33%, respectively), it is unclear whether that translated into clinically significant benefit for the patients. Crenolanib is now being investigated in combination with induction chemotherapy in patients with newly diagnosed AML with a FLT3-ITD or TKD (NCT02283177).
ASP-2215
ASP-2215 is a potent inhibitor of both FLT3-ITD and FLT3-TKD mutations. A phase I/II trial was initiated in 2013 and interim results were reported in 2015.18 One-hundred sixty-six patients were enrolled in a combination of the dose escalation and in-parallel dose expansion cohorts and the maximum tolerated dose was 300 mg daily. Of note, both FLT3 wild-type and FLT3 mutant patients were enrolled on the study. FLT3 wild-type patients derived minimal benefit from the study drug with a composite complete remission rate (encompassing CR, CRi, and CRp) of 8% and a PR rate of 3%. In the FLT3 mutant patient population, the overall response rate was 57% with a composite CR rate of 43% and a partial remission rate of 15%. A phase 1 study of ASP2215 in combination with induction consolidation chemotherapy is ongoing (NCT02236013) and a randomized phase III study of ASP2215 versus salvage chemotherapy is planned (NCT02421939).
IDH1 and IDH2
IDH, the enzyme that converts isocitrate to alpha-ketoglutarate in the mitochondria (IDH2) or the cytoplasm (IDH1) as part of the citric acid cycle, is mutated in a subset of patients with de novo adult AML in retrospective analyses of large clinical trial databases. IDH2 is mutated in 10%-15% of patients and IDH1 is mutated in 5%-10% of adult AML.19-21 The prevalence of both IDH mutations appears to increase as patients age; IDH mutations have not been found, to date, in any patients with pediatric AML. Mutations in IDH2 are enriched in patients with normal karyotypes, but up to 30% of patients with IDH2 mutations have abnormal cytogenetics at the time of diagnosis that generally fall into the intermediate or unfavorable cytogenetic risk groups as defined by the National Comprehensive Cancer Network (NCCN). Elegant preclinical work done over the past 5 years has shown that the mutant IDH enzymes acquire neomorphic activity and catalyze the conversion of alpha-ketoglutarate into beta-hydroxygutarate (2-HG), elevate levels of 2-HG, and lead to dysregulation of target genes in the affected myeloblasts, leading to a block in differentiation and clinical AML.22-24 Inhibitors of mutant IDH1 and mutant IDH2 are currently in phase 1 clinical trials (NCT02381886, NCT01915498, NCT02074839) and early results have demonstrated that these agents have encouraging efficacy in patients with relapsed disease.
Interim results of a phase I/II study of AG-221 (Agios/Celgene), the first IDH-2 inhibitor currently in clinical trials, presented at the annual meeting of the European Hematology Association in 2015 demonstrated an overall response rate of 41%, in patients with relapsed/refractory AML.48 Twenty-seven percent of patients cleared their bone marrow of blasts with various levels of count recovery (true CR, CRi, and morphologic leukemia-free states) and 18% of patients achieved a true CR. An additional 14% of the patients had a true PR with normalization of platelet count and absolute neutrophil count (ANC). Seventy-six percent of the responding patients have been on treatment for at least 6 months. Interestingly, an additional 44% of patients had clinical stable disease, defined as a stable or decreased blast percentage in the bone marrow that does not meet the criteria for PR. Some of these stable disease patients are red cell transfusion independent, have normal platelet counts and a normal ANC, despite persistence of blasts in the bone marrow and peripheral blood. The number of patients with clinically meaningful stable disease, and those who are simply smoldering AML is an area of active investigation as it has implications for the OS benefit that may be observed in these patients.
Inhibitors of mutant IDH1 in clinical development include AG-120 (Agios) and IDH305 (Novartis). Early results of AG-120 in patients with relapsed AML have shown similar evidence of efficacy as the IDH-2 inhibitor, with an overall response rate of 31% and a true CR rate of 15%. An additional 27 patients had stable disease. Dose escalation continues and expansion cohorts in patients with relapsed/refractory AML have been initiated.
BCL-2 inhibitors, bromodomain Inhibitors, and DOT1L inhibitors
A variety of agents against non-mutated molecular targets are in the midst of clinical trials including BET inhibitors, DOT1L inhibitors, and the BCL-2 inhibitor ABT-199. The early results for these agents have show responses, but their activity is modest. Because of that, it is uncertain if these compounds will move forward as single agents for the treatment of AML. For example, the BCL-2 inhibitor ABT-199 showed a CR/CRi in 5 of 32 patients, the majority of whom had relapsed or refractory disease. Interestingly, 3 of the 5 patients with a CR/CRi had an IDH mutation.25 Although there is preclinical data suggesting that IDH1 and IDH2 mutations induce BCL-2 dependence in AML and inhibition of BCL-2 may be therapeutically effective, the small numbers of responders in this early study makes any statement about the clinical effectiveness of BCL-2 inhibition in IDH mutant AML premature.26
Similarly, preclinical studies of DOT1L inhibition in acute leukemia associated with translocations involving the mixed lineage leukemia (MLL) gene, show remarkable effectiveness in preclinical studies. Translating these remarkable results to patients has been more difficult. Inhibition of DOT1L with the small molecule EPZ-5676 produced a complete remission in 2 of 34 patients with an MLL rearrangement or MLL-partial tandem duplication. In 1 patient, not only did morphologic evidence of myeloid disease disappear, but leukemia cutis resolved and the patient achieved a cytogenetic remission.27
Similar to the excitement around DOT1L inhibition, small molecule inhibition of BET proteins has a robust preclinical rationale that is currently being tested in multiple clinical trials for AML (NCT02158858, NCT02308761, NCT01943851).28-30 To date, the only report from a clinical trial has been of the bromodomain inhibitor OTX015.31 In this study, 36 patients with relapsed and refractory leukemia (33 with AML, 2 with ALL, and 1 with MDS) were enrolled on this phase 1 dose escalation study and 28 were evaluable for dose limiting toxicity. Of these, 1 patient had a CRp and 1 patient had a true CR. Three other patients had evidence of clinical activity (decrease in blast percentage and resolution of gingival hypertrophy).
The results above speak to the difficulty of translating robust preclinical studies into therapeutically effective treatments in the clinic. The path forward for each of these drugs is either to identify a biomarker of response, or to consider combining these agents with other drugs that are synergistic.
Incorporating novel inhibitors into clinical practice: pitfalls and opportunities
Clonal evolution
When thinking about molecularly targeted therapies for AML we encounter the issue described in the introduction: AML is molecularly heterogeneous. The proliferative advantage of leukemic myeloblasts may shift away from the target that is suppressed by a novel agent, to a new molecular genetic alteration. This leads to the potential of a never-ending cascade of new gene mutations arising that need to be suppressed and old mutations that have been suppressed re-emerging to cause a relapse. Indeed, a classic example of this seen in routine clinical practice is the emergence of overt FLT3-ITD mutations in patients with relapsed AML. In addition, many patients with FLT3-ITD mutations treated with FLT-3 inhibitors are unable to achieve a true complete remission because FLT-3 is one of many drivers of disease. Finally, the clone that needs to be targeted, the so called “founder clone,” may have genetic alterations that are not discoverable with routine clinical assays.
Our ability to identify and target the founder clone may change in the next decade. With current technology, there are 2 potential ways to overcome therapeutic resistance. The first is to use targeted molecular agents in combination rather than sequentially. For example, patients with a FLT-3 ITD and IDH mutations can be targeted with both FLT3 and IDH inhibitors. This “off the shelf” approach of mixing and matching targets is attractive intellectually but realistically problematic. This, primarily, because we do not have the agents for many of the targets. Although these drugs will hopefully be developed over the next 5-10 years, a comprehensive approach to clinical trials that involves multiple pharmaceutical companies that test combination therapies is needed to quickly develop phase 1 trials that test combinations.
Given the inherent limitations of targeted therapy for AML, perhaps the ideal way to eradicate leukemia and produce cures is combining targeted therapy with chemotherapy or hypomethylating agents. The historical precedent for this suggestion is the example of the differentiating agent, all-trans retinoic acid (ATRA) for APL. Interestingly, single agent use of ATRA is remarkably effective, but the 3 year overall survival rate with ATRA alone is only 71%; this in a disease where the founder clone contains the t(15:17) translocation.32 Until the recent introduction of ATRA in combination with ATO the most effective way of curing APL was combining ATRA with traditional cytotoxic chemotherapy. Given the precedent, those patients with de novo AML, fit for induction chemotherapy, should be enrolled on clinical studies that combine induction chemotherapy with an inhibitor of a desired molecular target.
Conclusions
With varying degrees of potency, efficacy and durability, inhibitors of FLT-3, IDH1, IDH2, DOT1L, BET proteins, and ABT-199 demonstrate proof of concept that the molecular genetic alterations that drive AML, are targetable. However, AML is rarely driven by 1 genetic event and targeting a single mutation is unlikely to lead to clinical cure. Because AML arises from a complex set of molecular genetic events with competing clones that vie for a selective advantage, it is extraordinarily unlikely that we will ever treat AML with a single, imatinib-like drug. In addition, clonal evolution between diagnosis and relapse makes it unlikely that those same molecularly targeted drugs that put a patient into remission at the time of diagnosis will produce a CR at the time of relapse. In addition, with any of these molecularly targeted agents, especially those that lead to differentiation, will these agents cure AML, or simply turn an acute disease in to a chronic disease.
Correspondence
Eytan M. Stein, Leukemia Service, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY 10065; Phone: 212-639-3314; Fax: 212-772-8550; e-mail: steine@mskcc.org.
References
Competing Interests
Conflict-of-interest disclosure: The author has consulted for Agios Pharmaceuticals and Seattle Genetics.
Author notes
Off-label drug use: None disclosed.