Abstract
Human herpesvirus 8 (HHV8) is a gamma herpesvirus associated with Kaposi sarcoma, multicentric Castleman disease, and primary effusion lymphoma, lymphoproliferative diseases that are most commonly observed in immunocompromised individuals. The viral genome expresses genes responsible for inhibition of apoptosis, cell cycle entry, and angiogenesis. Viral homologs of human regulatory genes are expressed, providing stimuli for angiogenesis, B-cell proliferation, and immune evasion. Variations in expression of these factors give rise to the 3 known HHV8-associated malignancies. Identification of these pathogenetic mechanisms has led to exploration of targeted treatment approaches for all 3 of these disorders with success in Kaposi sarcoma and multicentric Castleman disease; primary effusion lymphoma remains a clinical challenge.
Introduction
Since human herpesvirus 8 (HHV8; also known as Kaposi Sarcoma Herpesvirus [KSHV]) DNA sequences were first identified in cutaneous Kaposi sarcoma (KS) tissue by Chang et al in 1994,1 much has been learned about its role in the pathogenesis of KS and other lymphoproliferative disorders, including multicentric Castleman disease (MCD) and primary effusion lymphoma (PEL). These rare neoplastic disorders that result from HHV8 infection are most commonly associated with immunodeficiency states, including HIV infection, iatrogenic immunodeficiency, and aging. This review focuses on the unique pathogenetic role the virus plays in each of these neoplasms and discusses clinical management strategies with a focus on the lymphoproliferative disorders.
Pathogenesis of HHV8-associated disease
HHV8 is a gamma herpesvirus and, like other viruses in its class, has both latent and lytic cycles. Figure 1 illustrates the differences in viral gene transcripts identified in HHV8-associated disease and will be referred to in the text. One of the unique characteristics of this virus is its expression of viral homologs of human regulatory proteins such as cyclin D, IL-6, bcl-2, and others.2 Infection is largely latent in B cells, neoplastic KS spindle cells, and some atypical endothelial cells in KS. Lytic infection occurs in < 3% KS cells3 and is more frequent in MCD.
Genome diagram of KSHV and viral transcripts expressed in KS, PEL, and MCD. There are more than 90 genes in the viral genome, but this diagram only shows those mentioned in this review. The arrows underneath the genome indicate the transcripts expressed in virus-infected cells in the 3 pathologies associated with KSHV. As discussed in the text, the majority of cells are latently infected in KS, PEL, and MCD, whereas there is a higher rate of lytically infected cells in MCD than in KS or PEL. The vIRF-3/K10.5/LANA-2 transcript appears to be expressed only in KSHV-infected B cells, as found in PEL and MCD. Used with permission from Schulz et al.4
Genome diagram of KSHV and viral transcripts expressed in KS, PEL, and MCD. There are more than 90 genes in the viral genome, but this diagram only shows those mentioned in this review. The arrows underneath the genome indicate the transcripts expressed in virus-infected cells in the 3 pathologies associated with KSHV. As discussed in the text, the majority of cells are latently infected in KS, PEL, and MCD, whereas there is a higher rate of lytically infected cells in MCD than in KS or PEL. The vIRF-3/K10.5/LANA-2 transcript appears to be expressed only in KSHV-infected B cells, as found in PEL and MCD. Used with permission from Schulz et al.4
Latent gene expression
HHV8 latent genes expressed include latency associated nuclear antigen (LANA-1), v-FLIP (a viral analog of the FLICE inhibitory protein), and v-cyclin, all expressed off of the LANA promoter; and Kaposin B (for review, see Schulz4 and Fukumoto5 ). Latent gene expression is present in all 3 disorders and centers around the ability of these proteins to promote cell cycle progression and inhibit apoptosis, whether in KS spindle cells or B cells associated with MCD or PEL.
The role of latency in the pathogenesis of HHV-8 disease has been described previously.3 Cell cycle progression is promoted by LANA-1, which binds the tumor suppressor Rb, leading to enhanced expression of E2F, and by expression of v-cyclin, which binds to and activates cdk6 (Figure 2). Apoptosis is suppressed by binding of LANA-1 to p53, blocking its ability to act as a transcriptional activator and promoting survival. LANA-1 is also responsible for maintenance of the latent viral episome. V-FLIP is the third of the LANA-promoter coding regions that prevents Fas-induced programmed cell death by interfering with the Fas/TNFR pathway. Cell survival is also promoted through v-FLIP activation of NF-κB. In cultured PEL cells, inhibition of v-FLIP expression results in cell death and v-FLIP expression in primary endothelial cells results in the formation of KS-like spindle cells, a process that can be reversed with inhibitors of NF-κB. In KS, NF-κB may also play a role in up-regulation of host cytokine transcription. Kaposin B may play a role in stabilization of cytokine mRNA and may enhance cytokine release. Cytokines are responsible for the angiogenesis and inflammatory infiltrates that form a part of the histologic pattern observed in KS.
Pathogenesis of the HHV8-associated diseases KS, PEL, and MCD. Shown is the pathogenesis of the HHV8-associated diseases KS, PEL, and MCD demonstrating viral effects on apoptosis, cell cycle progression, angiogenesis, cytokine production, and B-cell proliferation as described in the text.
Pathogenesis of the HHV8-associated diseases KS, PEL, and MCD. Shown is the pathogenesis of the HHV8-associated diseases KS, PEL, and MCD demonstrating viral effects on apoptosis, cell cycle progression, angiogenesis, cytokine production, and B-cell proliferation as described in the text.
Lytic gene expression
HHV8 lytic genes include v-IL6, v-BCL2, v-MIP, viral G-protein coupled receptor (v-GPCR), and viral IFN regulatory factor (v-IRF-1), all of which are homologs of human regulatory genes. Lytic virus expression is most common in MCD, less so in KS, and uncommon in PEL. Although the expression of lytic cycle genes in the 3 diseases discussed here may differ, there are certainly commonalities that can be related to the clinical characteristics of the disorders. The unique role of HHV8 in the pathogenesis of each of the 3 malignancies is discussed below (Figure 2).
KS.
HHV8 is required for the development of KS and the virus is found in all subtypes of the disease, including classical, endemic, epidemic (HIV-associated), and posttransplantation KS. KS lesions are characterized by the presence of neoangiogenesis. Cultured cells transfected with v-GPCR up-regulate VEGF and bFGF,6 factors that play key roles in the pathogenesis of KS. Expression of v-GPCR in transgenic mice produces angioproliferative lesions that resemble KS.7 VEGF expression is associated with the vascular proliferation seen in KS histologic sections and may be responsible for the lymphedema so frequently associated with extensive cutaneous involvement with the disease. Furthermore, HHV8 infection induces c-kit gene expression in dermal microvascular endothelial cells, transforming them from a cobblestone-like monolayer to KS-like spindle cells.8 C-kit immunoreactivity can be identified in 45% of AIDS-KS biopsies and in 56% of classic KS cases.9 Finally, HHV8 infection also up-regulates mRNA expression of multiple matrix metalloproteinases.10 All of these findings represent potential targets for therapeutic intervention.
PEL.
PEL is characterized as an aggressive lymphoma presenting with malignant pleural, pericardial, or peritoneal effusions in the absence of a discrete tumor mass. The cells are of B-cell origin, although they rarely express CD20. Expression of CD38 and 138 suggest a late stage of B-cell differentiation.4,11 HHV8 is universally associated with this disease. The pattern of gene expression is predominantly latent. Most cells express LANA, v-cyclin, v-FLIP, and kaposin. V-IL6 is expressed in 2% to 5% of PEL cells, significantly higher than other lytic genes.4 As in KS, VEGF expression is high in PEL-derived cell lines and can be detected in the effusions of patients with PEL, suggesting that VEGF may play a role in the origin of the effusions.4 It is noteworthy that a majority of PEL patients also demonstrate latent coinfection with EBV, although there is limited expression of EBV-related genes and their role in pathogenesis remains unclear, with HHV8 likely playing the major role.12
MCD.
Also known as “angiofollicular hyperplasia,” MCD is most commonly observed in HIV patients and transplantation recipients, in whom it is virtually always associated with HHV8. In this disease, up to 50% of B cells within the mantle zone of the lymph node are infected based upon detection of LANA-1.4 Gene expression is broad in MCD, indicating a much stronger component of lytic infection than in either PEL or KS. V-IL6 is expressed in many of the LANA-positive cells, is frequently detected in blood, and is believed to be a key factor responsible for B-cell proliferation. In addition, expression of v-FLIP, v-GPCR, and kaposin-B may play a role in enhancing cytokine expression, with VEGF again playing an important role in the “angioproliferative” component, as is the case in KS.
Clinical presentation and management
KS
The incidence of AIDS-associated KS has declined dramatically since the introduction of combination antiretroviral therapy (cART) in 1996, but it remains the most common malignancy in HIV-infected individuals. In addition, the classic form of KS occurring in older individuals from endemic HHV8 regions is occasionally seen and KS remains a significant problem in sub-Saharan Africa in areas without cART access.
The lesions typically have a violaceous appearance and involve mucocutaneous surfaces. The disease can be cosmetically disfiguring and, with extensive spread of the disease in the skin, may be associated with lymphedema, pain, and secondary infection. Visceral involvement, infrequently observed in the cART era, may result in gastrointestinal or respiratory symptoms. Death due to KS is rare and can be associated with pulmonary involvement.
Localized, cosmetically unsightly lesions are most commonly treated locally with liquid nitrogen or, less often, with intralesional injection of vincristine. Localized radiotherapy is also an option for larger lesions, but doses should be kept low to avoid late complications of therapy, such as sclerotic skin changes and chronic lymphedema.
Systemic disease responds well to institution of cART in most patients, demonstrating the beneficial effect of immune reconstitution.13 In a small number of patients, institution of cART may be associated with initial progression of KS as a manifestation of an immune reconstitution inflammatory syndrome.
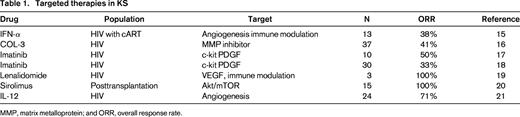
For patients with more advanced, symptomatic disease, systemic chemotherapy is used, typically with liposomal doxorubicin (Doxil) or paclitaxel (Taxol).14 A variety of investigational agents have been studied or are currently in clinical trials in patients with KS, with some successes, as noted in Table 1. IFN-α, perhaps functioning as an angiogenesis inhibitor, was found to be an active agent in KS very early in the HIV epidemic15 ; however, toxicities, use of cART, and availability of other effective agents have limited its use in recent years.
Significant responses were seen in patients treated with the matrix-metalloprotein inhibitor COL-3 and in 2 trials of imatinib. A case report of 3 patients with advanced refractory KS responded to treatment with lenalidomide19 and a phase 1/2 trial has just completed enrollment through the AIDS Malignancy Consortium (AMC).
Finally, targeting Akt/mammalian target of rapamycin (mTOR) activation by the HHV8 GPCR with sirolimus has proven to be active in KS associated with renal transplantation20 for those who do not respond to reduction in immunosuppression.
MCD
MCD has been observed in both HIV-seropositive and HIV-seronegative patients. Those cases occurring in the setting of HIV infection are most likely to be associated with HHV8, whereas HIV-seronegative patients are more often HHV8-negative.4,22 The clinical presentation has described previously by Sebbing et al22 and Mylona et al.23 Most individuals with MCD present with diffuse lymphoadenopathy, fever, weight loss, and hepatosplenomegaly. KS is present in up to 70% of individuals with MCD at diagnosis. Laboratory abnormalities include anemia in most patients, polyclonal hypergammaglobulinemia, hypoalbuminemia, cytopenias, respiratory symptoms, elevated C-reactive protein, and weight loss. Lymphocytic interstitial pneumonia may occasionally be observed and a polyneuropathy may occur with or without POEMS syndrome. The disease may take on a pattern of exacerbations with subsequent spontaneous remissions, whereas in others, a severe acute illness may occur with a rapid downhill course.
The diagnosis of MCD is based upon tissue biopsy, usually from a lymph node. The plasmacytic variant is most commonly observed in HIV patients and consists of hyperplastic follicles with indistinct borders and interfollicular zones containing sheets of plasma cells and vascular hyperplasia.22 In some cases, plasmablasts may be seen in the mantle zone in patients with HIV disease. These are most often polyclonal, but occasionally will progress to monoclonal plasmablastic lymphomas.23 Studies to identify the presence of HHV8 either from tissue or peripheral blood should be performed. Immunohistochemical staining for LANA will identify the presence of HHV8 in 10% to 30% of lymphocytes in the mantle zone.4 It should be remembered that HIV-negative individuals may not demonstrate the presence of HHV8 in nodal lymphocytes, but should still show the classic histologic findings of MCD.
Treatment of MCD
Chemotherapy.
A review of all MCD cases reported in the literature including patients treated with vinblastine; CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone); ABV (doxorubicin, bleomycin, vincristine); oral etoposide; or intermittent cyclophosphamide demonstrated that although some durable responses could be observed, most were relatively short lived and incomplete.23
IFN-α.
Anti-herpesvirus therapy.
Although active lytic viral replication is highest in MCD and disease flare is usually associated with an increase in HHV8 viremia that is responsive to anti-herpesvirus agents, data supporting their use as treatment for this disease are somewhat lacking and mostly anecdotal. A series of 3 cases reportedly responded to ganciclovir.23 In another series, 2 of 6 patients responded to a variety of anti-herpesvirus agents.26 Responses were not observed in 5 patients treated with cidofovir.23 Of interest is a more recent pilot study targeting 2 HHV-8 lytic genes, in which 86% of 14 HIV-positive patients with MCD responded to high-dose zidovudine plus valganciclovir.27
Rituximab.
Because the pathogenesis of MCD reflects HHV8 infection of B cells in the mantle zone, the use of an anti-CD20 monoclonal antibody to eliminate these pathogenic cells seems rational In a prospective trial, 4 weekly 375 mg/m2 infusions in 21 patients resulted in resolution of clinical symptoms and laboratory abnormalities in 20 patients and 70% had radiographic response.28 Overall survival and disease-free survival at 2 years were 95% and 79%, respectively Responding patients demonstrated declines in KSHV peripheral blood viral load. A second prospective trial demonstrated remission at 60 days in 22 of 24 patients treated with 4 weekly doses of rituximab.29
In a multicenter retrospective study, 52 patients with HIV-associated MCD had outcomes evaluated based upon use of different MCD therapies.26 Treatment with rituximab with or without chemotherapy resulted in significantly better overall survival (not reached vs 5.1 years, P = .03) compared with chemotherapy alone or anti-herpesvirus therapy. These observations provide the best evidence that rituximab, either alone or in combination with chemotherapy, represents the best option for first-line treatment for MCD in patients with HIV infection. It should be noted that patients with MCD and concurrent KS may experience significant progression of KS after rituximab therapy. In as study of 12 MCD patients with KS, treatment with a combination of liposomal doxorubicin and rituximab was highly active in controlling both HHV-8–related diseases.30
Hu-Anti-IL6R.
Immediately after administration of this humanized monoclonal anti-IL-6 receptor antibody to 7 HIV-negative patients, fever and fatigue disappeared and anemia and serum levels of C-reactive protein, fibrinogen, and albumin started to improve.31 By 3 months, patients had reductions in lymphadenopathy and hypergammaglobulinemia and improvement of renal function. Remissions were not sustained, however, and recurrence was observed.
KSHV inflammatory cytokine syndrome
Uldrick et al32 reported a series of 6 patients with HIV and HHV-8 coinfection without pathologic evidence of MCD who presented with an inflammatory syndrome similar to that observed in MCD. These patients had HHV-8 viral lytic activity and cytokine patterns, including marked elevation of vIL-6 and hIL-6, that resembled those observed in patients with MCD. The diagnosis is made based upon the finding of MCD-like clinical manifestations (eg, fever, fatigue, edema, cachexia, arthralgia, myalgia, respiratory or GI symptoms, neuropathy, cytopenias, lymphadenopathy, or hepatosplenomegaly) with evidence of inflammation (elevated C-reactive protein) and elevated KSHV viral load in the absence of any evidence of MCD. Because this is a newly described syndrome, there is no reported therapeutic experience. However, treatment modalities described for MCD, such as rituximab, should be considered if the diagnosis seems likely.
PEL
PEL is characterized by the presence of malignant pleural, pericardial, or peritoneal effusions in the absence of a discrete tumor mass. An extracavitary form of the disease has also been described.4 These are rare lymphomas that comprise only approximately 2% to 4% of all HIV-associated lymphomas.33 Cases are occasionally observed in the posttransplantation setting and in elderly patients in areas where HHV8 is endemic, such as the Mediterranean and sub-Saharan Africa.33
Cytologic examination of fluid demonstrates large cells that may have either an immunoblastic or plasmablastic appearance.4 Positive immunohistochemical staining for LANA-1 is required to make the diagnosis. The disease most frequently occurs in HIV-infected individuals with relatively advanced immunodeficiency and often in the presence of other HHV8-related disorders such as KS and MCD.33 Although the cells are B cells, they typically express neither a B- nor a T-cell immunophenotype and fail to express surface or cytoplasmic Ig. The tumor cells are typically positive for CD45, CD30, CD38, and CD138,33 suggesting plasmablastic differentiation. In a review of 61 cases of PEL reported in the literature, 93% were CD45-positive, 38/52 (73%) were CD30-positive, and T- and B-cell markers were expressed in 4.9% and 1.6%, respectively.34
The clinical presentation of PEL (for review, see Chen et al33 ) is a result of accumulation of malignant effusions resulting in dyspnea, chest pain, or abdominal distention. The pleural space is the most commonly involved. Twenty-seven to 71% of patients have a prior diagnosis of KS. By definition, all patients have stage IV disease and International Prognostic Index score is not predictive of clinical outcome35 There is no standard of care and there are no prospective trials of any treatment for this entity, although CHOP-like chemotherapy is often used.
In a multicenter retrospective analysis of 28 cases of PEL (the largest series reported to date), 15 patients received CHOP-like regimens, some of which included etoposide and some methotrexate. Other regimens included dose-reduced CHOP (n =6), IFN-α (n = 2), IFN with cidofovir (n = 3), and no therapy (n = 1). With a median followup of 3.8 years, the overall median survival was 6.2 months. For 14 patients who achieved complete response, the 1-year disease-free survival rate was 78.6% (95% confidence interval, 56.6-100.6) and the median disease-free survival was 94.8 months. The only independent poor prognostic factors were Eastern Cooperative Oncology Group score of > 2 and absence of prior cART.35
In the 3 largest series reported (N=11-28), the complete response rates in response to CHOP-like chemotherapy ranged from 43% to 50% and median survivals were 3 to 6 months.33
The role of high-dose chemotherapy with autologous stem cell transplantation in PEL is unclear, because only 2 case reports have been reported in patients with relapsed/refractory disease, one successful (HIV-negative) and one not successful (HIV-positive).33
In view of evidence of up-regulation of NF-κB expression in PEL, the role of the proteasome inhibitor bortezomib has been explored. However, despite demonstrating growth inhibition and apoptosis in cultured PEL cells,36 reactivation of HHV8 lytic gene expression and cell death in mice with human PEL xenografts, and increased survival in SCID mice inoculated with UM-PEL-1 cells,37 bortezomib failed to demonstrate activity in 3 patients treated with the drug either alone or in combination with chemotherapy.38
Experiments using PEL cell lines and/or murine xenograft PEL models have suggested that several agents, including rapamycin (sirolimus),39 IFN-α combined with arsenic trioxide,40 the anti-CD30/drug conjugate brentuximab vedotin,41 and histone deacetylase inhibitors,42 exert antitumor effects in PEL. The combination of bortezomib with the histone deacetylase inhibitor vorinostat was shown to potently reactivate HHV-8 lytic replication, inducing PEL cell death and prolonging mouse survival in a xenograft model.43 Clinical use of this combination has yet to be reported. The mTOR inhibitor rapamycin decreases production of VEGF and may prevent accumulation of effusions, but clinical data are lacking. Two cases in which disease responded to cART alone in patients with PEL have also been reported.44
Given the low level of lytic infection in patients with PEL, the expectation of success with anti-herpesvirus therapy is low. There have, however, been some isolated reports of success with intracavitary cidofovir45 and with systemic cidofovir combined with IFN-α and cART.46 Rapid achievement of complete response was observed in a single patient treated with a combination of azidothymidine and IFN-α.47 In both the patient's primary tumor cells and in PEL cell lines, this proapoptotic effect was demonstrated to be mediated through concomitant activation of TNF-related apoptosis-inducing ligand and NF-κB.
Summary
HHV8-associated neoplasms represent a unique group of rare malignancies. Although we have yet to fully understand the mechanisms by which this fascinating herpesvirus is responsible for many of the genetic and biochemical observations that have been described, targeted approaches based on these findings show signs of success, particularly in KS and MCD. PEL remains problematic and its rarity makes clinical study difficult.
Disclosures
Conflict-of-interest disclosure: The author declares no competing financial interests. Off-label drug use: None disclosed.
Correspondence
Lawrence Kaplan, Division of Hematology-Oncology, Box 0324, UCSF, San Francisco, CA 94143; Phone: 415-353-2421; Fax: 415-353-2467; e-mail: lkaplan@medicine.ucsf.edu.