Abstract
Thrombocytopenia is a common hematologic finding with variable clinical expression. A low platelet count may be the initial manifestation of infections such as HIV and hepatitis C virus or it may reflect the activity of life-threatening disorders such as the thrombotic microangiopathies. A correct identification of the causes of thrombocytopenia is crucial for the appropriate management of these patients. In this review, we present a systematic evaluation of adults with thrombocytopenia. The approach is clearly different between outpatients, who are frequently asymptomatic and in whom we can sometimes indulge in sophisticated and relatively lengthy investigations, and the dramatic presentation of acute thrombocytopenia in the emergency department or in the intensive care unit, which requires immediate intervention and for which only a few diagnostic tests are available. A brief discussion of the most common etiologies seen in both settings is provided.
Introduction
Thrombocytopenia is defined as a platelet count below the 2.5th lower percentile of the normal platelet count distribution. Results of the third US National Health and Nutrition Examination Survey (NHANES III) support the traditional value of 150 × 109/L as the lower limit of normal.1 However, platelet counts between 100 and 150 × 109/L do not necessarily indicate disease if they have been stable for more than 6 months,2 and the adoption of a cutoff value of 100 × 109/L may be more appropriate to identify a pathologic condition.3 Furthermore, it is now appreciated that in many non-Western countries, the lower threshold of the normal platelet count is lower than 150 × 109/L.3
The relevance of thrombocytopenia in the individual patient is variable and depends on the clinical presentation. Because platelets play an essential role in preserving vessel wall integrity, thrombocytopenia is associated with a defect of primary hemostasis. Clinically significant spontaneous bleeding does not usually occur until the platelet count is less than 10-20 × 109/L. However, the presence of thrombocytopenia can aggravate surgical or traumatic bleeding or prevent the administration of effective treatment for several conditions (eg, antiviral therapy for chronic hepatitis C virus infection or cancer chemotherapy). In other situations, a low platelet count is the only initial manifestation of an underlying disorder that poses greater risks than thrombocytopenia itself (eg, HIV infection or myelodysplastic syndromes) or is an important marker of disease activity (eg, thrombotic microangiopathies). Establishing the cause of thrombocytopenia has obvious clinical repercussions, but is sometimes quite challenging. This is particularly the case for hospitalized patients, in whom thrombocytopenia appears frequently in the background of a multisystem disorder and may be determined by multiple mechanisms. Conversely, in the outpatient setting, thrombocytopenia is often isolated and asymptomatic, and the diagnosis of the specific cause is usually straightforward (Table 1). Thrombocytopenia in pregnancy deserves special consideration because of the possible consequences on the fetus. A structured approach to the diagnosis of thrombocytopenia involves an integration of clinical findings and appropriate support from the laboratory and other medical disciplines.
Clinical scenarios and most common causes of thrombocytopenia
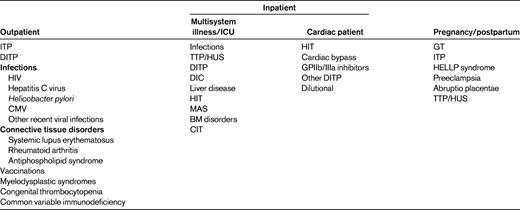
TTP/HUS indicates thrombotic thrombocytopenic purpura/hemolytic uremic syndrome; MAS, macrophage activation syndrome (including hemophagocytic syndrome); CIT, chemotherapy-induced thrombocytopenia; HELLP, hemolysis, elevated liver enzymes, and low platelets.
Mechanisms of thrombocytopenia
The major mechanisms for a reduced platelet count are decreased production and increased destruction of platelets. Typical examples of the former are the BM failure syndromes (eg, aplastic anaemia, myelodysplastic syndromes, and chemotherapy-induced thrombocytopenia), whereas increased destruction is seen in conditions such as disseminated intravascular coagulation (DIC) and the thrombotic microangiopathies. Two less common mechanisms are platelet sequestration and hemodilution. Platelet sequestration is seen in congestive splenomegaly due to portal hypertension and is characterized by redistribution of platelets from the circulating pool to the splenic pool.4 Hemodilution is seen in patients who have suffered a massive hemorrhage and have received colloids, crystalloids, and platelet-poor blood products.
It is now known that in many cases of thrombocytopenia, such as primary immune thrombocytopenia (ITP) and hepatitis C virus infection, multiple mechanisms may contribute to the development of thrombocytopenia.
Role of history taking and physical examination
Taking a thorough medical history can provide invaluable information and greatly facilitate diagnosis. Aspects of particular relevance that should be investigated include the presence of a family history of thrombocytopenia (it is not infrequent to diagnose congenital thrombocytopenia in adults); the temporal profile of the thrombocytopenia or of the bleeding manifestations (new onset, chronic, or relapsing); disease history, with particular reference to autoimmune disorders, infections, or malignancies; pregnancy status in premenopausal woman; recent medications and vaccinations; recent travels (eg, malaria, rickettsiosis, dengue fever); recent transfusions; recent organ transplantation; ingestion of alcohol and quinine-containing beverages; dietary habits; and risk factors for retroviral infections and viral hepatitis. A history of recurrent, symptomatic thrombocytopenia with platelet counts returning to normal within days, even in the absence of specific treatment, should prompt investigation of a drug-induced thrombocytopenia. The bleeding history does not help in diagnosing the nature of the thrombocytopenia, but gives important clues about its duration and defines its clinical phenotype. Collecting a detailed medical history is not always possible, the typical situation being the unconscious patient with severe thrombocytopenia in the intensive care unit (ICU). However, in such cases, thrombocytopenia is almost always an acute event and the disease history and exposure to medications (eg, heparin and antibiotics) immediately preceding the development of thrombocytopenia should be available in the patient's notes.
Physical examination should focus on the location and severity of bleeding risk and other abnormalities that can help in the diagnosis of the thrombocytopenia, such as the presence of organomegaly or skeletal abnormalities. Patients with thrombocytopenia typically experience mucocutaneous bleeding. The presence of joint or extensive soft tissue bleeding suggests the presence of coagulation abnormalities, such as occurs in DIC. The presence of an ischemic limb of skin necrosis should raise suspicion of heparin-induced thrombocytopenia (HIT).
Role of the laboratory
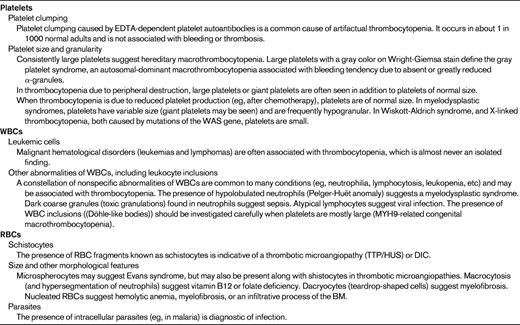
Step 1: Observation of the peripheral blood smear
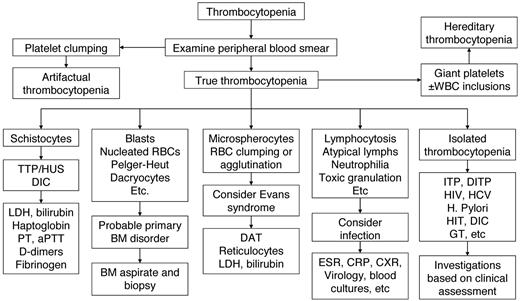
In the era of genomic medicine and widespread molecular testing, examination of the peripheral blood film still remains the most important investigation guiding our diagnostic approach to thrombocytopenia (Figure 1). All 3 blood cell lineages should be assessed carefully (Table 2). From a practical perspective, when we are investigating thrombocytopenia in a critically ill patient, the immediate information we need to obtain is whether it is thrombotic microangiopathy (as shown by RBC fragmentation) or acute leukemia (blasts). Even a short delay in making these diagnoses may prove fatal for the patient if appropriate treatment is not initiated promptly.
Algorithm for workup of thrombocytopenia based on observation of the peripheral blood film. TTP/HUS indicates thrombotic thrombocytopenic purpura/hemolytic uremic syndrome.
Algorithm for workup of thrombocytopenia based on observation of the peripheral blood film. TTP/HUS indicates thrombotic thrombocytopenic purpura/hemolytic uremic syndrome.
Step 2: Additional investigations
Bearing in mind that thrombocytopenia can be the end result of pathogenetic mechanisms that are not mutually exclusive and that, particularly in the acute care setting, multiple potential causes of thrombocytopenia can be identified, a basic laboratory evaluation should include liver and renal function tests, a clotting screen with D-dimers, and measurement of lactate dehydrogenase.
Second-tier investigations should be prompted by clinical findings and the results of the peripheral blood smear. There is no single hematologic or biochemical test that is conclusive for a given mechanism of thrombocytopenia. If the etiology of the thrombocytopenia is unclear, a BM aspirate and biopsy should be performed to rule out a primary BM disorder. Reticulated platelets or the equivalent immature platelet fraction can help in discriminating between thrombocytopenia due to BM failure (low percentages) and hyperdestructive thrombocytopenia (high percentages),5,6 although the specificity of these tests has not been validated prospectively. Limited evidence suggests that plasma glycocalicin and thrombopoietin levels can increase the specificity of reticulated platelets in thrombocytopenia due to increased platelet destruction.7 The most common specific etiologies and associated investigations are discussed in the next sections.
Isolated thrombocytopenia
In the context of this review, we define isolated thrombocytopenia as a low platelet count in the absence of abnormalities of RBC and WBC lineages and no signs or symptoms of systemic illness.
A low platelet count during a routine evaluation in an otherwise asymptomatic person is a relatively common reason for referrals to hospital outpatient clinics by general practitioners. Nevertheless, patients with severe thrombocytopenia can present to the emergency department with mucocutaneous bleeding or internal hemorrhage. Isolated thrombocytopenia has a limited differential diagnosis (Table 1). The 2 most prevalent etiologies are ITP and drug-induced thrombocytopenia (DITP).
ITP
Although ITP is the most common cause of isolated thrombocytopenia, there are no tests sensitive or specific enough to confirm this diagnosis, which remains one of exclusion. There is no consensus on the set of investigations to perform, and practice varies greatly not only from country to country, but also from center to center within the same country. There is little doubt that local resources may play a relevant role in the choice of investigations. In my current practice, I follow the recommendations set forth in the International Consensus Report on the investigation and management of ITP (Table 3),8 although admittedly some of these recommendations are based on poor evidence. I also request an ultrasound of the abdomen (to rule out the occasional initial manifestation of chronic liver disease with hypersplenism and the presence of enlarged abdominal-pelvic lymph nodes) and a chest X-ray (to rule out “silent” mediastinal lymphadenopathy and “silent” tuberculosis). Antiplatelet Ab assays are not very sensitive, although their specificity approaches 90%. They may be useful in differentiating ITP from DITP. The role of the BM biopsy and aspirate in patients with isolated thrombocytopenia remains controversial. The International Consensus Report panel recommends performing these investigations in patients more than 60 years of age, because isolated thrombocytopenia may be the initial abnormality of a myelodysplastic syndrome. Conversely, the updated ASH guidelines for immune thrombocytopenia suggest that BM studies are not necessary in patients of any age in whom physical examination, complete blood count, and examination of the peripheral blood smear do not suggest etiologies other than ITP.9
Basic laboratory evaluation of patients with suspected ITP according to the International Consensus Report
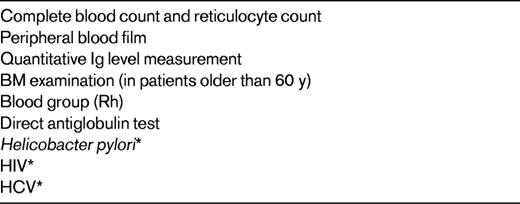
Adapted from Provan et al.8
*Recommended by the majority of the panel for adult patients regardless of geographic locale.
DITP
The list of drugs associated with thrombocytopenia is an ever-increasing one (www.ouhsc.edu/platelets). Because of its peculiar pathogenesis and clinical course, HIT will be discussed separately. The pathophysiologic mechanism of DITP is the development of drug-dependent Abs against new epitopes of platelet glycoproteins created by their interaction with the drug. Patients with DITP usually present with moderate to severe thrombocytopenia and bleeding manifestations of varying degrees of severity. The decrease of the platelet count typically occurs within 2-3 days (sometimes a few hours) of taking a drug that has been taken previously or 1-3 weeks after starting a new drug. When the drug is stopped, the thrombocytopenia usually resolves in 5-10 days after drug withdrawal. Clinically, DITP can be easily confused with ITP and only an accurate history collection can help in the diagnostic process.10 If the patient has recently taken a medication for the first time, a diagnosis of DITP should be considered. DITP should also be suspected when patients have recurrent episodes of thrombocytopenia with prompt recovery. Sometimes the diagnosis is very challenging because the substance causing the thrombocytopenia is not a drug, but a food or beverage, such as walnuts,11 cow's milk,12 cranberry juice,13 tonic water (which contains quinine), and certain herbal remedies.14
The diagnosis of DITP is mostly empirical, being based on platelet recovery after discontinuation of the drug or after abstaining from certain foods or beverages. Laboratory diagnosis involves the demonstration of drug-dependent antiplatelet Abs by methods such as flow cytometry, platelet immunofluorescence test, ELISA, and immunoprecipitation-Western blotting.
Thrombocytopenia in the hospitalized patient
Thrombocytopenia may complicate the course of the hospital stay of patients with a variety of medical and surgical problems. In one study, thrombocytopenia was observed in approximately 1% of adult inpatients in an acute care hospital.15 However, less than 30% of these patients presented with bleeding manifestations. As expected, thrombocytopenia is much more common in ICUs, where it is found in in 8%-68% of patients on admission, and in 13%-44% of patients during the stay in the unit.16 Many potential etiologies are often concomitant in the acute care setting (eg, sepsis, DIC, drugs, and cardiac bypass surgery), and it is not always possible to elucidate the cause of the thrombocytopenia. However, because of its frequency, consideration should always be given to DITP. The frequency of DITP in critically ill patients is approximately 20%. Antibiotics in this setting are a frequent etiology.17,18 Tests for the detection of drug-dependent antiplatelet Abs are not widely available, are time-consuming, and are not sensitive enough to be incorporated in a diagnostic algorithm for the urgent management of patients with severe thrombocytopenia. The decision to discontinue a potential causative drug in such cases should rely solely on clinical criteria.19
Heparin-induced thrombocytopenia
HIT occurs in 0.5%-5% of heparin-treated subjects, depending on the patient population studied.20 It should be suspected in any patient who, while on heparin therapy, has a ≥ 50% decrease in platelet count compared with baseline or a total platelet count of < 100 × 109/L with normal baseline counts. Thrombocytopenia is usually moderate, with median platelet counts ranging from 50-80 × 109/L and nadir counts rarely below 20 × 109/L. Clinical manifestations may include venous or arterial thrombosis, necrotic skin lesions at heparin injection sites, or acute systemic reactions subsequent to IV heparin bolus administration. At present, it is not possible to predict which patients will develop these complications. However, HIT is relatively rare in the ICU, where it accounts for fewer than 1% of cases of thrombocytopenia.21
HIT typically develops after exposure to heparin for 5-10 days. Earlier onset of HIT (sometimes a few hours after the first heparin administration) occurs in approximately 30% of cases. These patients have a history of exposure to heparin in the prior 3 months, thereby developing Abs against the heparin-PF4 complex. Less commonly (in 10%-15% of cases), HIT has a delayed onset, occurring several days after all heparin has been stopped.
HIT is often a clinical emergency, and on such occasions, the presumptive diagnosis has to be based solely on clinical findings. There is simply no time to wait for the results of heparin-PF4 Ab testing. In addition, these Abs can also be present in heparin-treated patients who do not have a clinical syndrome of HIT. Clinicians can be supported in their choices by clinical scoring systems based on the pretest probability of HIT, such as the one known as the “4Ts”: Thrombocytopenia, Thrombosis, Timing, and other causes of Thrombocytopenia (Table 4).22 In patients with strongly suspected HIT, heparin therapy should be stopped and an alternative anticoagulant be administered until the results of a confirmatory test are available. Although the gold standard for diagnostic tests for HIT is the 14C-serotonin release assay, this is available in only a few comprehensive centers. Commercial enzyme immunoassays are widely available and very sensitive (> 90%), but are not very specific. However, a positive ELISA with high optical density values can improve the accuracy and specificity of the diagnosis.23
The 4Ts pretest probability of heparin-induced thrombocytopenia
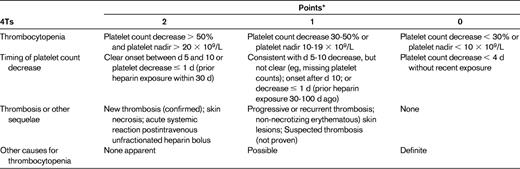
Pretest probability score: 6-8, high; 4-5, intermediate; 0-3, low. Adapted from Lo et al.22
*0, 1, or 2 for each category with a maximum possible score of 8.
DIC
DIC is a consumptive coagulopathy complicating several diseases. It is characterized by activation of intravascular coagulation with microvascular thrombi formation, thrombocytopenia, depletion of clotting factors, variable bleeding complications, and end-organ damage. DIC can develop acutely or present with a chronic course. The International Society on Thrombosis and Haemostasis (ISTH) further recommends classifying DIC as overt (decompensated hemostatic system) or non-overt (compensated coagulopathy).24
Acute DIC is commonly seen in severe sepsis and septic shock, after trauma (especially neurotrauma), after surgery, as an obstetric complication (eg, abruptio placentae, amniotic fluid embolism, and preeclampsia), after ABO-incompatible blood transfusion, and as a complication of acute promyelocytic leukemia. Consumptive coagulopathy in these cases is severe and leads to bleeding manifestations (eg, mucocutaneous bleeding and blood oozing from wound sites) and frequent organ damage (eg, renal and hepatic damage). There is no single laboratory test for accurate and precise diagnosis of DIC. The ISTH committee has proposed a scoring system using the parameters reported in Table 5,24 in which a score ≥ 5 is consistent with overt DIC. Chronic DIC is more frequently observed in solid tumors and in large aortic aneurysms, usually with few obvious clinical or laboratory indications of the presence of DIC. Fibrinogen levels may be slightly decreased, within the reference range, or even increased. Platelets may be moderately low or normal and D-dimer levels are modestly elevated.
Diagnostic score for the diagnosis of overt DIC
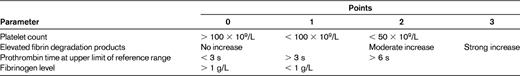
An overall score of 5 or more is compatible with overt DIC. A score less than 5 is suggestive of non-overt/low-grade DIC. Adapted from Taylor et al.24
Thrombocytopenia in the cardiac patient
Several mechanisms can induce thrombocytopenia in patients undergoing open heart surgery. Cardiopulmonary bypass may result in mechanical destruction of platelets, hemodilution in the bypass circuit, and drug-induced platelet destruction. More rare causes include sepsis, intra-aortic balloon pumping, and posttransfusion purpura. The nadir platelet count is typically seen on the second or third day after surgery, with a rapid platelet count recovery thereafter.
Severe thrombocytopenia is observed in 0.1%-2% of patients after exposure to GPIIb/IIIa inhibitors (eg, abciximab, tirofiban, or eptifibatide) during percutaneous coronary intervention. The peculiarity of this DITP is its rapid onset, usually within a few hours after surgery. This phenomenon has been attributed to the presence of naturally occurring Abs against neoepitopes exposed by alteration of the GPIIb/IIIa molecule.25 In typical cases, thrombocytopenia resolves within 10 days. Delayed development of thrombocytopenia 3-6 days after treatment with abciximab has been described in a few patients.26 The mechanism of the thrombocytopenia in these cases is the production of Abs against murine peptide sequences of abciximab, which react with other target epitopes on abciximab-coated platelets.
HIT is an important cause of thrombocytopenia in patients undergoing cardiac surgery. It occurs in 1%-3% of patients receiving heparin beyond the first postoperative week27 and in 10% of patients after ventricular assist device implantation.28 Extreme caution should be used in the interpretation of the assays for HIT because of the high proportion of false positives. In fact, in the first 10 days after cardiac surgery, 25%-70% of patients develop a positive immunoassay for heparin-PF4 Abs and 4%-20% have an abnormal serotonin release assay.27
Thrombocytopenia in pregnancy
Platelet counts < 150 × 109/L have been reported in 6%-15% of women at the end of pregnancy, but counts < 100 × 109/L are observed in only 1% of women.29 The most common causes of thrombocytopenia are gestational thrombocytopenia (GT; 70%), preeclampsia (21%), and ITP (3%).30
GT is seen in the mid-second to third trimester of pregnancy and is supposed to represent the extreme variation of the physiologic decrease of the platelet count that is observed during pregnancy.29 There is no clearly defined minimum value of the platelet count in GT, but counts < 70 × 109/L should raise suspicion of an alternative diagnosis. There are no confirmatory laboratory tests of GT and the diagnosis remains one of exclusion. To support a diagnosis of GT, women should have no past history of thrombocytopenia (except during a previous pregnancy), and the thrombocytopenia should resolve spontaneously within 1-2 months after delivery. Furthermore, the fetus/newborn baby should have not suffered from thrombocytopenia.
ITP occurs in 1-2 in 1000 pregnancies, but is the most common cause of isolated thrombocytopenia in the first and early second trimesters.31 Approximately one-third of cases are first diagnosed during pregnancy, whereas two-thirds are in patients with preexisting disease. There are variable reports of exacerbation of ITP during pregnancy or in the postpartum period. Approximately half of patients with a prior diagnosis of ITP experience a mild decline in platelet count progressively during pregnancy. Differentiating ITP from GT is clinically relevant, because pregnancies in women with ITP may be complicated by severe neonatal thrombocytopenia in 9%-15% of cases, with a risk of neonatal intracranial hemorrhage of 1%-2%.32 In women with no history of ITP, platelet counts below 100 × 109/L early in pregnancy and declining as gestation progresses are more consistent with ITP than with GT. The situation becomes more complicated if a low platelet count is detected during the third trimester. Again, there are no clear lower limits of the platelet count in GT, and there is a “hazy” platelet count range between 50 and 70 × 109/L in which the diagnosis remains uncertain. From a clinical perspective, knowing the exact diagnosis at that stage of pregnancy changes little in the management of the pregnancy, although consideration will be given to the possible thrombocytopenia of the neonate. Whenever the platelet count is < 50 × 109/L in the absence of obstetric complications, the diagnosis should be ITP by default. As always in medicine, results need to be interpreted in the clinical context.
Conclusions
A low platelet count can result from a wide range of conditions and may be determined by multiple mechanisms. Prompt recognition of the cause of thrombocytopenia is often crucial for the correct management of patients, as in acute promyelocytic leukemia, heparin-induced thrombocytopenia, or thrombotic thrombocytopenic purpura/hemolytic uremic syndrome. The initial approach to determining the cause of thrombocytopenia is based on the patient's history of underlying diseases and drug treatments, on physical examination, and on careful examination of the peripheral blood smear. The 2 most common causes of a low platelet count in the absence of other hematologic abnormalities and no evidence of a multisystem disease are ITP and DITP. The most common cause of a low platelet count in pregnancy is GT. In hospitalized and critically ill patients, the diagnosis of thrombocytopenia is often challenging due to the presence of several potential etiologies, including drugs and infections. Examination of the BM with aspiration and biopsy is warranted in patients with severe or worsening thrombocytopenia of unexplained nature. Thrombocytopenia in pregnancy deserves special consideration because of the possible consequences on the fetus.
Disclosures
Conflict-of-interest disclosure: The author is on the board of directors or an advisory committee for Nycomed; has consulted for LFB, Symphogen, SuppreMol, Amgen, and GlaxoSmithKline; has received honoraria from Amgen and GlaxoSmithKline; and has been affiliated with the speakers' bureau for Amgen, GlaxoSmithKline, Bayer, Novo, and Baxter. Off-label drug use: None disclosed.
Correspondence
Dr Roberto Stasi, Department of Haematology, St George's Hospital, Blackshaw Road, London SW17 0QT, United Kingdom; Phone: 44-208-725-3545; Fax: 44-208-725-3918; e-mail: roberto.stasi@stgeorges.nhs.uk.