Abstract
Allogeneic stem cell transplantation (SCT) can be considered the most successful method of adoptive immunotherapy of cancer. It is successful in part because of the potent graft-versus-tumor (GVT) effects of the donor graft, which are independent of the conditioning regimen. This potent GVT reaction can be harnessed in some cases to treat patients who relapse after allogeneic SCT with the use of donor leukocyte infusions (DLIs). This has led to the rapid development of reduced-intensity conditioning (RIC) regimens for allogeneic SCT, an approach that relies primarily on GVT activity. However, the effects of GVT have clear disease specificity and remain associated with significant GVHD. Optimization of GVT induction will require a better understanding of the important target antigens and effector cells, as well as the development of methods that enhance GVT reactivity without excessive GVHD. The appropriate clinical setting and timing for GVT induction need to be defined more clearly, but ultimately, the immunologic control of cancer through allogeneic adoptive immunotherapy represents one of the most potent and promising therapeutic strategies for patients with hematologic malignancies.
GVT effects in allogeneic SCT
It is well accepted that successful allogeneic stem cell transplantation (SCT) is related in part to the graft-versus-tumor (GVT) potential of the donor graft, which is independent of the conditioning regimen. Early clinical evidence for GVT activity was largely circumstantial and based on important but indirect observations that withdrawal of immunosuppression could restore remission after relapse in some cases, that development of GVHD was associated with a decreased incidence of relapse, and that T-cell depletion of the donor graft increased relapse rates, at least for patients with chronic myelogenous leukemia (CML).1 The first direct demonstration of clinical GVT activity was the successful application of donor leukocyte infusions (DLIs) to treat relapsed CML.2 The natural culmination of these observations has been the development of reduced-intensity conditioning (RIC) regimens for allogeneic SCT that promote the engraftment of donor cells and rely primarily on GVT induction rather than dose-intensive chemotherapy to cure patients with hematologic malignancies.
Biology of GVT induction
Although GVT induction is typically attributed to donor T cells, the biology of GVT induction is poorly understood, and likely involves a complex interaction of multiple cell types, antibodies, and cytokines.3 Whereas T cells are critical for antitumor activity, the contribution of alloreactive natural killer (NK) cells is particularly evident in the setting of T cell–depleted, HLA-mismatched transplantation.4 Some studies have reported conflicting results regarding the contribution of NK cells to GVT activity, although recent work suggests that GVT activity may be optimized by donor NK cells expressing appropriate killer-cell immunoglobulin-like receptor (KIR) genes.5
Another cell population that may play a role in GVT induction is dendritic cells (DCs). Both host and donor DCs can modulate alloreactivity and whereas residual host DCs appear to be important for GVHD induction, the role of DCs in GVT induction has been controversial and not well defined.6
In addition to direct and indirect cell-mediated GVT responses, antibody-mediated responses likely contribute to GVT induction, at least in some cases.3 Antibodies have been identified against several tumor targets such as CML, myeloma, and acute myelogenous leukemia (AML) cells after transplantation and/or DLIs. The mechanism of antibody-induced GVT activity is likely complicated. Antibodies can mediate both complement-mediated cytotoxicity and antibody-dependent cellular cytotoxicity, may facilitate antigen presentation or T-cell responses, or could be directed against cytokines and other molecules important for the activation or inhibition of GVT activity. B-cell reconstitution and survival are also dependent on and can be affected by the presence of the proper cytokine environment (such as expression of B-cell activating factor or BAFF).
It is clear that GVT induction is likely influenced not just by tumor type and antigen expression, but also by a complex interaction of suppressive and activating cytokines, multiple effector cells, and antibodies. In addition, the effector mechanisms for GVT induction may be different depending on the specific transplantation conditions, such as T-cell depletion and conditioning regimen intensity, and maximizing clinical activity will likely require a multifaceted approach.
RIC allogeneic SCT
The development of RIC allogeneic SCT has been one of the most important advances in the field. This modality relies less on conditioning regimen intensity and more on the GVT effects of the donor graft. In some cases, outcomes after RIC SCT appear similar to outcomes after conventional allogeneic SCT, in part because the lower mortality rate from conditioning regimen toxicity is offset by a higher risk of relapse.7,8 Among other important issues, this implies that dose intensity still has a role in disease eradication and cannot be eliminated in some cases. Dose intensity may be particularly important in patients with rapidly progressive diseases and large tumor burdens, and less important for patients with indolent diseases and lower tumor burdens.9
Numerous RIC regimens of varying intensity continue to be developed in an effort to minimize the toxicity of transplantation while attempting to maximize GVT activity, and outcomes with different regimens have been reviewed elsewhere.10 The role of in vitro or in vivo T-cell depletion with RIC SCT is not well defined, and may lead to higher relapse rates, but outcomes may be dependent in part on the extent and timing of T-cell depletion.11
Treatment of relapse after RIC allogeneic SCT is similar to approaches for relapse after conventional SCT. It is not clear if patients are more or less responsive to GVT induction for relapse after RIC; it is possible that patients who relapse early may not have had time to benefit from the GVT effects of RIC allogeneic SCT and may be more likely to respond to withdrawal of immunosuppression or DLI. Alternatively, relapse, particularly late after RIC allogeneic SCT, may select for patients not responsive to GVT induction, and alternative strategies for these patients need to be considered. It is also possible that relapsed disease may be more responsive to conventional cytotoxic therapies after a RIC allogeneic SCT compared with diseases exposed to myeloablative doses of chemotherapy. Therefore, there may be different (or more) options for conventional therapy, alone or in combination with cellular therapy, for relapse after RIC SCT. Regardless, mortality is quite high in all cases of relapse after RIC transplantation, although patients given therapy seem to have better outcomes than patients who receive no intervention12 and limited data suggest that response rates to DLI after RIC allogeneic SCT are similar to those after conventional SCT.
GVT induction to treat relapse
Relapsed CML
There is no debate that GVT induction with DLI is dramatically effective for relapsed CML after allogeneic SCT. Molecular remissions are achieved in up to 80% of patients who relapse in the chronic phase,13 and these remissions are sustained in the majority of patients. Treating relapsed CML with DLI provides one of the best opportunities to separate GVT induction from GVHD. Particularly for patients with early and indolent relapse, using low doses of donor T cells, followed by gradual dose escalation if needed, has been able to minimize acute GVHD without limiting GVT activity.14 The relative safety of a dose-escalation strategy has been confirmed by additional studies in patients with other diseases.15
Given the potential toxicity associated with even with low-dose DLI, tyrosine kinase inhibitors (TKIs) may be an effective alternative to treat relapsed CML without the risk of GVHD. Available data suggest that up to 70% of patients achieve a complete molecular remission, although unlike DLI, continued therapy is likely necessary to prevent progression.16 Even patients who do not respond to DLI may still respond to TKIs.17 Another alternative is combination therapy with imatinib (or another TKI) with DLI. This approach has not been prospectively studied, but has the advantage of rapid reduction in leukemia burden and disease control until an effective immune response can develop.18 It must be taken into consideration that many patients will likely be resistant to TKIs as the original indication for transplantation. It not known if resistance to TKIs will confer resistance to GVT induction in CML, although in one study, patients who lost a response to a TKI for relapsed CML were unlikely to respond to DLI.19
Acute leukemia
Once patients relapse after allogeneic transplantation with acute leukemia, remissions may be achieved in a subset with either conventional chemotherapy or newer biological agents, but response rates are low and long-term survival is poor. New strategies to optimize GVT effects for these patients are urgently needed.
Although acute lymphoblastic leukemia (ALL) is clearly susceptible to GVT induction,20–22 most patients with relapsed ALL do not respond to DLI, and remission rates range between 0% and 20% and overall survival (OS) is < 15%.23 In a subset of patients with Philadelphia chromosome–positive ALL, the use of new TKIs may have particular benefit with or without GVT induction.24
Outcomes after GVT induction for relapsed AML are more variable, and the most appropriate strategy remains controversial. Several issues need to be considered. Responses to conventional DLI occur in 15%-30% of patients with AML, but remissions are often transient and long-term survival and cure occurs in approximately 20% of patients. Nevertheless, patients treated with DLI appear to have better outcomes than patients who never receive DLI, with OS estimated at 21% versus 9% at 2 years, respectively.25 Furthermore, patients who relapse later after SCT and receive DLI have improved outcomes compared with patients who relapse early after SCT.25,26
The role of cytoreductive therapy before DLI remains a topic of continued debate. When patients with acute leukemia are given chemotherapy before DLI, complete remissions are more common, which could translate into improved survival.26 It may be that GVT induction is more effective for patients in remission, as highlighted by a recent European Group for Blood & Marrow Transplantation analysis.25 This report also identified a population of patients with a high probability of response; patients who received DLI in remission with a favorable karyotype had a 2-year OS of 56%, in contrast to patients who received DLI with active disease or during aplasia, who had an OS of 9%-20% (overall 15%) depending on other risk factors.
Myeloma, lymphoma, and chronic lymphocytic leukemia
Potent GVT effects have been identified for multiple myeloma (MM), nonHodgkin lymphoma (NHL), Hodgkin disease (HD), and chronic lymphocytic leukemia (CLL), as recently reviewed in detail.22 Most studies using DLI to induce GVT for relapsed myeloma have reported limited success, although a minority of patients enjoy prolonged responses.27 Immunomodulatory agents used in the treatment of myeloma, such as thalidomide and lenalidomide, have been combined with DLI in the hope of enhancing its immune effect; overall and complete responses using thalidomide/DLI have been encouraging.28 There is also interest in combining DLI with bortezomib based on data suggesting that proteasome inhibition can provide a direct antitumor effect, inhibit alloreactive T cells, and promote myeloma cell killing, which may be able to separate GVT induction from GVHD.29 Ultimately preventing relapse may be the most effective strategy for patients with myeloma; maintenance lenalidomide after autologous SCT improves progression-free survival.30 Trials using lenalidomide maintenance after allogeneic SCT are under way, although preliminary studies suggest that this may increase the risk of GVHD31
Although also susceptible to GVT effects of transplantation, response rates to DLI for relapse of NHL, HD, and CLL are quite variable,22 likely reflecting the heterogeneity of these diseases, the patients who undergo transplantation, and the variable disease and transplantation characteristics at the time of relapse. For patients with relapsed NHL, response rates vary between 53% and 85%, often with DLI given after T cell–depleted grafting, and different histologies have different susceptibilities. For example, follicular lymphoma may be particularly sensitive to GVT induction with DLI.15 DLI has also been combined with rituximab in a pilot study designed to prevent relapse after reduced intensity SCT, and was found to be both safe and effective.32
Compelling evidence also supports an important GVT effect for both HD and CLL. This is supported both by long-term remissions after RIC allogeneic SCT,33 and the response of both relapsed HD and CLL to DLI.22,34 However, for both diseases, response rates to DLI are highly variable, and defining the most appropriate timing and method of GVT induction has been difficult due to the small numbers of patients studied and the highly heterogeneous patient and disease characteristics. One recent study administered DLI to patients with mixed chimerism after a T cell–depleted RIC SCT for HD, This strategy resulted in a remarkably low 5% incidence of relapse at 4 years, compared with a 43% incidence of relapse for patients who were full chimeras and did not receive DLI. Furthermore, 79% of patients with relapse responded to DLI. This confirms that HD is very susceptible to GVT induction, and that full chimerism does not predict for a low risk of relapse.
Defining relapse after allogeneic SCT
One major and controversial issue is how best to define relapse and risk of relapse after allogeneic transplantation. This definition is likely to evolve rapidly with the availability of new and more sensitive techniques to detect minimal disease burdens. The significance of minimal residual disease (MRD) detection is dependent on the detection method used, the disease burden identified, and the specific disease being studied. This is important because how relapse is defined has major implications for patient care, data interpretation, and future clinical trial design. Various methods studied to monitor MRD include standard cytogenetics, FISH, high-sensitivity chromosome analyses, real-time quantitative PCR (for mixed chimerism or disease-specific markers), multiparameter flow cytometry, and imaging studies (CT, PET, MRI, etc) for tumor recurrence. A detailed discussion of how best to define relapse and the clinical implications of MRD monitoring has been published recently.35 Disease-specific studies to define the preferred method, optimal timing, and frequency of MRD assessment and the risk of relapse based on MRD detection are necessary to determine the appropriate timing for intervention (assuming that intervention is feasible and effective).
GVT induction to prevent relapse
Regardless of how MRD is defined, it is clear that adoptive immunotherapy is likely to be most successful when used in the setting of MRD to prevent relapse. Treating molecular relapse of CML with low-dose DLI has been quite effective and can minimize toxicity.14 PCR monitoring for relapse may also be useful in patients with acute promyelocytic leukemia, in whom detecting recurrence of the RAR-a/PML transcript often heralds relapse.36 However, most diseases do not express unique genes that can be targets for PCR analysis. In addition, PCR detection of MRD in other diseases is both more difficult and of less clear clinical significance because it is often coincident with rapid relapse.
Rather than monitoring for a tumor-specific transcript with PCR, monitoring mixed chimerism may be a surrogate for impending relapse. This is useful in both CML and ALL, and can serve as an indicator for early application of DLI.37,38 It is less clear if mixed chimerism is useful to predict relapse in AML, lymphoma, and other diseases after transplantation.34,39,40
One recent study administered DLI to patients with mixed chimerism after RIC SCT for HD. This strategy resulted in a remarkably low 5% incidence of relapse at 4 years compared with a 43% incidence of relapse for patients who were full chimeras and did not receive DLI. This suggests that HD is very susceptible to GVT induction, and that full chimerism does not predict for a low risk of relapse.
Because GVHD is significant after DLI,41 studies of prophylactic DLI must include a careful assessment of GVHD risk. Timing and dose of DLI are critical and GVT induction in close proximity to either conditioning therapy or cytoreductive chemotherapy may lead to frequent and severe GVHD,42 perhaps due to the homeostatic proliferation of T cells that occurs in lymphodepleted states or to the proximity of the cytokine-abundant phases that occur after chemotherapy.
The utility of prophylactic adoptive immunotherapy is dependent on the clinical setting. It may be particularly useful in restoring GVT activity after T cell–depleted transplantations.43 To enhance GVT induction with DLI after in vivo T-cell depletion for allogeneic SCT, we performed a phase II study using donor T cells expanded and activated through ex vivo costimulation (by exposure to anti-CD3/CD28–coated beads). Two planned doses were given at 4 months (1 × 107 CD3+ cells/kg) and 6 months (1 × 108 CD3+ cells/kg) after transplantation, and preliminary results confirmed that this was safe and that there was minimal acute GVHD.44 Longer follow-up will be needed to determine whether this approach enhances GVT activity. Other studies suggest that with the appropriate dose and schedule of DLI, GVT activity can be restored, leading to similar outcomes compared with patients who receive T cell–replete stem cell grafts.45
Novel strategies to enhance GVT activity
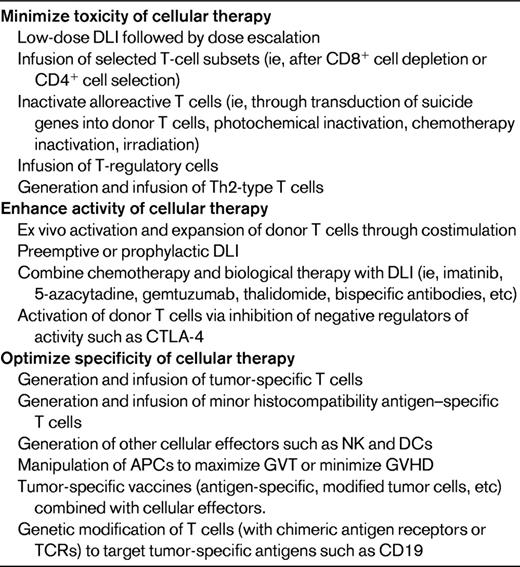
Whereas GVT induction to treat relapse is both promising and potent, high response rates are largely limited to CML, and outcomes for all patients remain limited by significant GVHD and other toxicities. Numerous innovative approaches are actively being pursued to both maximize GVT induction and limit GVHD (Table 1).
To improve on outcomes of allogeneic cell therapy, it will be necessary to understand why GVT induction is effective in some cases and not others. It is possible that donor T cells become rapidly senescent quickly after SCT or DLI,46 a mechanism that could limit GVT and lead to relapse. In this circumstance, the use of repetitive DLI may be useful, and we are testing this strategy in clinical trials. To overcome limitations associated with poor T-cell activation in vivo, we are testing the use of “activated DLI” using donor T cells activated and expanded ex vivo through costimulation. Donor T cells are exposed to artificial APCs coated with antibodies to CD3 and CD28, become activated, and can be expanded > 100-fold. Preliminary results using these cells for relapse show that this approach is safe and results in good GVT responses.47 It may also be possible to activate donor immune functions in vivo through vaccination of recipients with tumor-specific antigens48,49 or modified tumor cells.50 Another promising approach is the combination of DLI with novel antibodies that can direct and activate effector cells directly at the site of tumor; this is another strategy that theoretically could overcome possible resistance mechanisms to GVT induction without excessive toxicity.51 An alternative strategy to maintaining activation of donor T cells is inhibition of negative regulators of activity such as CTLA-4. Ipilimumab, an anti-CTLA4 monoclonal antibody, has been tested as therapy for relapse in 29 patients; 3 responses were noted, including 2 of 14 patients with relapsed HD and 1 patient with relapsed mantle cell lymphoma.52 This highlights the possibility that manipulation of both positive and negative regulators of T-cell activation may be able to enhance GVT activity.
It may also be possible to generate leukemia-specific cytotoxic T cells to use for adoptive immunotherapy.53,54 However, in most cases, tumor-specific target antigens are unknown. Minor histocompatibility antigens (mHAgs) are attractive tumor targets because they may exhibit differential tissue expression. T cells directed against mismatched mHAgs have activity in vitro against leukemic cells and have now been created and tested.55 Patients with relapsed acute leukemia after allogeneic transplantation have been treated with CD8+ T-cell clones manufactured to recognize mHAgs on recipient hematopoietic cells but not recipient dermal fibroblasts.56 Transient responses were seen, but they were accompanied by unanticipated pulmonary toxicity. Nevertheless, this approach demonstrates both the potential power and continued challenges associated with tumor-specific cellular therapy.
In other cases, potential tumor-associated antigens may be normal cellular antigens that are overexpressed. Proteinase 3 (PR3) is overexpressed in myeloid leukemic cells, and vaccination with the PR-1 epitope of PR3 has shown considerable antileukemic activity.50,57 Wilms tumor protein (WT1) is overexpressed on myeloid malignancy cells as well, and could serve as a potential target for vaccination strategies or for the generation and expansion of tumor-specific DLI products.58 Additional antigens considered as targets for immunotherapy have included BCR/ABL, NY-ESO-1, a cancer-testis antigen commonly expressed on myeloma cells, and PRAME, an HLA-24–restricted antigen on AML cells.
It is now possible to genetically modified T cells to express chimeric antigen receptors and redirect T-cell specificity.59 Exciting data have been obtained using autologous T cells expressing an anti-CD19 chimeric antigen receptor in patients with CLL and B-cell malignancies.60,61 Kochenderfer recently reported the use of donor T cells expressing an anti-CD19 chimeric antigen receptor to treat a patient with relapsed CLL after allogeneic SCT. This patient failed both DLI and second allogeneic SCT and had a dramatic response within 26 days of the cellular infusion.62
Effector cells other than T cells likely participate in GVT induction, at least in some situations. For example, NK cells can have potent antitumor activity, and several trials have demonstrated the safety and feasibility of donor NK-cell infusions after haploidentical SCT.63 New techniques to isolate and expand NK cells ex vivo should lead to more detailed testing of NK-cell immunotherapy.64
Building on these and other novel cellular strategies to enhance antitumor immune responses and modulate immune complications of transplantation should improve the safety, specificity, and success of cellular therapy after allogeneic SCT.
Second allogeneic SCT
Second allogeneic SCT needs to be considered a potent form of adoptive immunotherapy and may be appropriate for a subset of patients who relapse, although subsequent relapse and treatment-related mortality rates may be unacceptably high. Toxicity from second transplantation can be limited with the use of RIC, but at the expense of higher relapse rates. Whether a RIC regimen improves outcome compared with conventional conditioning for a second allogeneic transplantation is not known.
The most appropriate donor for second SCT is also not well defined. It would seem logical to use a new (or even a mismatched) donor, because one assumes relapse is due in part to insufficient GVT activity provided by the original donor. However, available data do not support an obvious benefit with a second donor. Factors associated with improved outcomes after second allogeneic SCT have been age, disease status, and time to relapse. Data from the Center for International Blood and Marrow Transplant Research showed that the survival for patients < 20 years of age who relapsed > 6 months from transplantation was 51% at 5 years and only 3% for older patients who relapsed within 6 months.65 The European Group for Blood & Marrow Transplantation reported the best outcomes for patients with late relapse (> 292 days) in remission at the time of second transplantation (53% survival at 3 years).66 Outcomes are also likely to be dependent on other factors such as the intensity of the first and second conditioning regimen and susceptibility of the underlying disease to GVT induction.
Because second allogeneic SCT is used primarily as adoptive immunotherapy in most cases, it is not known if this is more effective (or more toxic) than GVT induction with DLI. Studies comparing the outcomes of second SCT with DLI for relapse would be particularly important to define the most effective method of GVT induction to treat relapse.
Summary
It is now possible to harness the antitumor potential of human T cells to treat cancer, both in the setting of allogeneic SCT and with the use of DLI after allogeneic SCT. Many novel strategies are being tested to maximize the GVT reactivity associated with transplantation. Whereas allogeneic adoptive immunotherapy can be quite powerful, many issues remain to be determined for optimization of GVT activity. It is not known whether the GVT reaction is a generalized allogeneic effect or has disease-specific targets, and it has not yet been possible to consistently separate GVT from GVHD. The contribution of immune effector cells other than T cells (such as APCs and DCs) or new biologic agents and immune modulators (alone or in combination with cellular therapy) to augment GVT activity needs to be explored in detail. Understanding the mechanisms of relapse will lead to better strategies for GVT induction. Ultimately, although there is a critical need for small, innovative pilot studies, well-designed international cooperative trials are going to be needed to understand how best to optimize and harness GVT activity for maximal clinical benefit.
Acknowledgments
This work was supported in part by a grant from the National Institutes of Health (K24 CA11787901).
Disclosures
Conflict-of-interest disclosure: The author declares no competing financial interests. Off-label drug use: Cellular therapy for relapsed disease after allogeneic SCT.
Correspondence
David L. Porter, MD, 3400 Civic Center Blvd, PCAM 2 West Pavilion, Philadelphia PA 19104; Phone: (215) 662-2862; Fax: (215) 615-5888; e-mail: david.porter@uphs.upenn.edu.