Abstract
An 18-year-old African-American male with sickle cell disease (SCD) is admitted to the hospital with a vaso-occlusive pain crisis affecting his chest and right upper extremity. He has a history of asthma but does not have a fever or respiratory symptoms, and a chest X-ray is negative for an infiltrate. He is treated with intravenous fluids and morphine. You are asked about the potential efficacy of systemic corticosteroids as an adjunctive treatment for pain control.
Pain is the most common complication of SCD, with a lifetime prevalence of greater than 95%.1 There is a general consensus that an underlying inflammatory state contributes to the pain of SCD and to the complex phenomenon called sickle cell vasculopathy, which also consists of many other pathophysiologic components.2 Pro-inflammatory red cells and cytokines are believed to activate the vascular endothelium, compromise vascular integrity, and promote both erythrocyte and leukocyte adhesion in vascular beds. Multiple studies have demonstrated that patients with SCD have chronically elevated levels of multiple inflammatory mediators,3–4 suggesting the utility of systemic corticosteroids as a treatment for vaso-occlusive events such as pain. However, the exact relationship between measures of pain and those of vaso-occlusion and sickle cell vasculopathy are still under study. Furthermore, recent retrospective data suggest a correlation between the use of corticosteroids for acute chest syndrome and complications such as rebound pain and stroke,5–7 raising the issue of both safety and efficacy of corticosteroids in this patient population. To determine the potential role of systemic corticosteroids in the management of acute pain in SCD, we conducted a comprehensive, computerized literature search of the PubMed database for randomized, double-blind, placebo-controlled trials in which patients with SCD were treated with intravenous or oral corticosteroids for pain or acute chest syndrome.
The search strategy combined the National Library of Medicine's Medical Subject Heading (MeSH) terms “anemia, sickle cell” (no restrictions, 15,357 hits) with the keyword “glucocorticoids” (to exclude studies in which patients received synthetic mineralocorticoids). The bibliographies of the included articles were also scanned for relevant citations, and the principal investigators of ongoing clinical trials were contacted via e-mail for preliminary results. This strategy yielded 56 citations for review. Excluded were 18 case reports, six editorials, six reviews, three retrospective studies, and one meta-analysis. One article was not available in English, so it was excluded, as were 10 studies in which participants were not administered intravenous or oral corticosteroids, and seven reports that were not specific to participants with SCD. Four full-length manuscripts were left for review, two of which were excluded because one was a case series10 and one an in vitro study.11 One ongoing trial was identified,12 but no preliminary results were available for analysis.
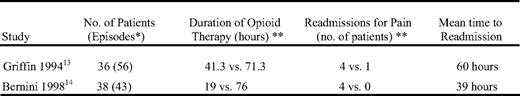
The two remaining manuscripts13–14 originated from the same institution and represented 74 patients between the ages of 1.4 and 19 years (mean age approximately 6.7 years; Table 1). The 74 patients represented 99 episodes of either pain or acute chest syndrome, of which 48 were randomized to receive steroids, and 51 were randomized to receive placebo. One study13 randomized patients admitted with pain to either methylprednisolone 15 mg/kg/dose up to 1000 mg intravenously for two doses or placebo, and reported a shorter duration of analgesic therapy in the experimental arm (41.3 vs. 71.3 h; p = 0.03). The second study14 randomized patients admitted with acute chest syndrome to either dexamethasone 0.3 mg/kg/dose intravenously for four doses or placebo and reported a shorter mean duration of hospitalization in the experimental arm (47 vs. 80 h; p = 0.005). A pooled analysis showed a combined relative risk of 8.5 (95% confidence interval 1.1–65.4; p = 0.04) for readmission to the hospital in favor of placebo.
The available evidence suggests that the use of systemic corticosteroids for the acute pain of SCD is associated with a shorter duration of opioid therapy, at least in children. However, it is unknown whether this equates to a shorter duration of pain. The use of corticosteroids does appear to increase the risk of rebound pain and subsequent readmission to the hospital. The underlying mechanism of rebound pain following the use of corticosteroids is unknown, although proposed hypotheses include rebound inflammation and retrograde embolization of marrow fat.15–16
Given the available data, our strength of recommendation for the use of systemic corticosteroids in patients admitted for acute pain of SCD is Grade 2B.17 This strength of recommendation is based on two relatively sound clinical trials of small numbers of mostly children from the same institution, which yielded both benefits and possible harms of therapy.
In conclusion, we suggest that systemic corticosteroids be used with caution in patients with SCD. Further research into the phenomenon of rebound pain following the use of corticosteroids may help to further elucidate the underlying pathophysiology of varying pain phenotypes in SCD.
Disclosures
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Off-label drug use: None disclosed
Correspondence
Vandy Black, MD, Johns Hopkins University, 720 Rutland Avenue, Ross 1125, Baltimore, MD 21205; Phone: 410-955-6132; Fax: 410-955-8208; e-mail: vblack4@jhmi.edu