Abstract
Given its relative rarity, it may at first seem surprising that chronic myeloid leukemia (CML) has garnered so much attention over the last decade. Yet, the advances in molecular pathogenesis that have been derived from studying this leukemia have clearly benefited all of oncology. Moreover, the strides in drug design and development that have also ensued around CML have given rise to what others have called a molecular revolution in cancer therapy. While a majority of patients with chronic phase CML (CP-CML) have an excellent durable response to imatinib (Gleevec, Novartis, Basel, Switzerland), a clear minority will unfortunately have signs of primary or secondary resistance to therapy. Significant efforts geared toward understanding the molecular mechanisms of imatinib resistance have yielded valuable insights into the biology of drug trafficking into and out of cells, epigenetic control of cellular processes, alterations in enzymatic structures, and the rational structural-based design of small molecule enzyme inhibitors. This review will describe the efforts at understanding the pathogenesis of imatinib resistance and the molecular rationale for the development of second- and now third-generation therapies for patients with CML.
The past decade has demonstrated the power of translational medicine, linking the discovery of the pathogenic Bcr-Abl translocation in chronic myeloid leukemia (CML) with the potential of computational chemistry to develop small molecule kinase inhibitors.1–3 The phase III International Randomized Study of Interferon and STI571 (IRIS) trial randomized newly diagnosed chronic phase CML (CP-CML) patients to either 400 mg daily of imatinib or interferon-alpha with subcutaneous low-dose cytarabine. The 7-year update was recently presented and demonstrated an estimated event-free survival (EFS) and overall survival (OS) of 81% and 86%, respectively.4 Therapeutic response assessment with imatinib is based upon meeting hematologic, cytogenetic, and molecular milestones as established by the European LeukemiaNet consortium and later adopted by the National Comprehensive Cancer Network (NCCN).5,6 Patients failing to achieve defined responses at these chronological time points are described as primarily resistant to therapy, and those losing previously obtained milestones are termed secondarily resistant. Due to a relatively high censoring rate of nearly 20% and continued participation of only 60% of the original cohort in the IRIS trial, there is a concern that the previously published response rates may underestimate the true proportion of resistant disease. Prior data had indicated a 15% to 25% rate of primary cytogenetic resistance by 18 months of therapy with imatinib, and estimates of secondary resistance ranged from 7% to 15%. Indeed, a recently published smaller companion investigation by de Lavallade and colleagues estimated that an individual’s likelihood of remaining in a complete cytogenetic response (CCyR) while still receiving imatinib 5 years after diagnosis was approximately 63%, although this may underestimate the effectiveness of imatinib due to the discontinuation of therapy in a number of patients despite continued responses.7 However, discrepancies in the definitions of treatment failure in these two trials makes direct comparisons of resistance rates challenging. Regardless, approximately one third of patients may need alternative therapeutic options to imatinib, either due to resistance or intolerance.
Resistance to chemotherapy is a recurrent issue in all cancer histologies, but the molecular understanding of the mechanisms of resistance, especially in CML, is advancing at an unprecedented rate. It is apparent that a major reason for the therapeutic successes in CML is the well-defined molecular target and relatively selective therapies aimed at that target, which is not the case for the majority of cancers and chemotherapies today. Concurrently, the availability of compounds to target these mechanisms of resistance is also expanding, providing the clinical investigator with an increasing number of options which only ten years ago seemed unfathomable. This review will evaluate the information available describing various mechanisms of imatinib resistance, describe recent updates on the molecular options for overcoming these hurdles, and describe several novel small molecule inhibitors undergoing clinical development for resistant CML.
Bcr-Abl–Dependent Mechanisms of Resistance
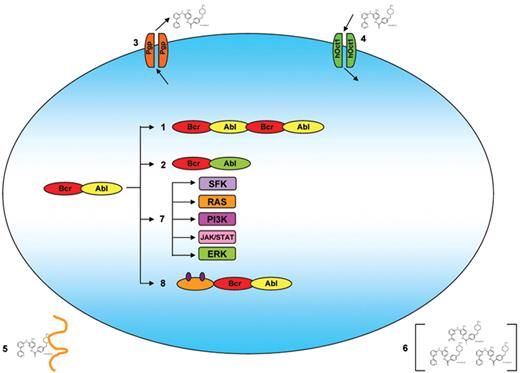
Because the Bcr-Abl enzyme is necessary and sufficient for the initiation and propagation of CML, inhibition of the Abl kinase activity was an ideal target for a molecular-based therapy.1,2,8 Shortly after the introduction of imatinib however, investigators began to describe a number of in-vitro derived cell lines with resistance to the drug, suggesting the potential for an inherent or acquired resistance to the therapy (Figure 1 ).9 This was rapidly followed by the clinical description of imatinib-resistant patients, which has resulted in efforts to understand the biology behind the observations.
Bcr-Abl Duplication
The first reports described the development of resistance through oncogene amplification. Utilizing cell lines derived from the peripheral blood of blast crisis CML patients, le Coutre and Weisberg developed imatinib-resistant clones through serial passages in imatinib-containing cultures and demonstrated elevated Abl kinase activity due to a genetic duplication of the Bcr-Abl sequence.10,11 Mahon and colleagues were also able to generate imatinib-resistant clones demonstrating an amplification in the Abl sequence.12 However, all of these samples were derived in vitro and may not have represented the true mode of clinical resistance. Nevertheless, Gorre et al obtained cells directly from imatinib-resistant patients, and genetic duplication of the Bcr-Abl gene was identified by using FISH analysis as one possible source of imatinib resistance.13 Yet the majority of patients fail to clinically demonstrate Abl amplification as a primary mode of treatment failure.
Bcr-Abl Mutation
As originally described by Schindler and colleagues, imatinib interacts with the nucleotide binding site of the Abl enzyme in the inactive, closed confirmation.14 This relatively rigid structural requirement for entry and binding of imatinib to the ATP-binding site also serves as a potential source for resistance. In samples obtained from imatinib-resistant patients, Gorre et al demonstrated a single C→T nucleotide substitution at position 944 of the Abl gene, resulting in a threonine to isoleucine substitution at amino acid 315 (Th315→ Ile315; T315I) of the Abl protein sequence.13 This amino acid substitution eliminates a critical oxygen molecule needed for hydrogen bonding between imatinib and the Abl kinase, and also creates steric hindrance to the binding of imatinib. Numerous additional mutations have been characterized throughout the Abl sequence, including the P-loop, C-helix, SH2 domain, substrate binding site, A-loop, and C-terminal lobe, some even prior to the initiation of therapy.15–17 Mutational frequencies also appear to increase as patients progress from chronic phase through to blast phase disease.
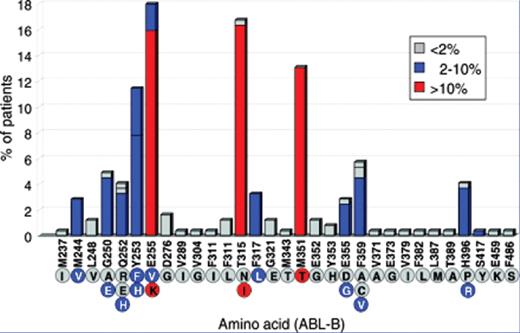
Although the total number of known point mutations continues to grow, their clinical significance in an individual patient may vary (Figure 2 ).9 When screening a cohort of patients with known clinical resistance, Nicolini demonstrated a decreased progression-free survival (PFS) and OS for only those patients harboring P-loop mutations or the T315I alteration.18 In a separate retrospective analysis of imatinib-resistant patients, Jabbour also demonstrated a high risk of disease progression associated with Abl mutations, but in their analysis, only non–P-loop mutations were associated with a poorer OS, and only when considering mutations as a time-dependent covariate.19 Bradford reviewed the clinical significance of point mutations located at the various structural domains of the Abl kinase, regardless of the patient’s clinical resistance status. In this cohort, a large majority of patients developing a mutation subsequently developed imatinib resistance, with the highest risk for disease progression conferred by mutations located in the P-loop.20 Chu and colleagues were able to identify mutations in CD34+ CML progenitor cells in 7 of 8 patients with chronic phase disease with rising Bcr-Abl transcript levels.21 However, only 2 patients subsequently demonstrated progressive disease, suggesting again that not all mutations are clinically significant. Because prior retrospective observations had identified kinase domain (KD) mutations in patients prior to tyrosine kinase inhibitor (TKI) therapy, Willis and colleagues prospectively assessed the frequency of mutations in imatinib-naive patients with CML to determine the frequency of these abnormalities as well as to determine the longer-term clinical significance of these a priori alterations.16,17,22 Utilizing a combination of an allele-specific polymerase chain reaction (PCR) assay together with conventional sequencing, changes were identified in 15 of 66 patients (23%), with the T315I detected most frequently. Mutations were detected in accelerated and blast phase patients, but none were seen in the 20 chronic phase patients. Interestingly, the identification of a mutation utilizing the very sensitive allele specific oligonucleotide (ASO) technology was not correlated with either EFS or OS. Moreover, 2 patients with the T315I mutation were able to achieve a CCyR with imatinib, 1 of whom obtained a complete molecular response (CMR), indicating that mutations detected by these very sensitive assays may not always confer a growth advantage to the clone.
Recently, a new splice variant has been described whereby a portion of the 8th intron is retained, resulting in a frame-shift mutation and subsequent insertion of 10 unique amino acids followed by an early stop codon.23 While infrequently identified in previously untreated patients, the transcript appeared to be more common in imatinib-refractory CP-CML patients, but not as common in accelerated phase (AP-CML) patients. Molecular modeling indicated that the splice variant had three-dimensional structural changes that could potentially mimic that of the T315I mutation in its interaction with imatinib. However, given the lack of progressive accumulation over time, it is unclear whether the splice variant has a transforming capacity and whether its presence results in a proliferative advantage upon imatinib exposure.
Bcr-Abl–Independent Mechanisms of Resistance
Drug Efflux
Additional mechanisms have been postulated to describe resistance seen in various model systems, although none have been clearly identified as a sole source of clinical resistance. Utilizing a cell line derived from a blast crisis CML patient and subsequently passaged through increasing dosages of imatinib, Mahon et al demonstrated an increase in the expression of the P-glycoprotein (Pgp) efflux pump.12 However, this same cell line also demonstrated a 6-fold amplification of the Bcr-Abl gene product, and no discrimination between the imatinib resistance imparted by the Abl duplication versus the Pgp overexpression was made. Measuring protein expression alone does not indicate functionality, and recently, Dulucq and colleagues evaluated polymorphisms in the multidrug resistance (MDR) sequence and revealed a differential major molecular response rate (MMR) to imatinib in three different subgroups with alternative single nucleotide polymorphisms (SNPs).24 Utilizing two different Pgp inhibitors, Che and Kotaki et al were able to modulate the activity of the export protein and restore imatinib susceptibility to previously resistant cell lines.25,26 More recently, two groups have used a small inhibitory ribonucleic acid (siRNA) to downregulate Pgp expression and have restored imatinib susceptibility in vitro while concurrently demonstrating an increased intracellular concentration of imatinib.27,28 Clinically, Langue and colleagues reported a similar clinical response to imatinib in patients with myeloid blast crisis independent of the level of expression of Pgp seen in the blasts.29 Similarly, Crossman et al failed to find a statistically significant difference between the levels of Pgp in bone marrow mononuclear cells in both pretreatment and post-therapy samples in patients who had achieved a CCyR versus those achieving less than a minor cytogenetic response after 10 months of imatinib therapy, raising the suspicion that Pgp expression itself may not be a clinically relevant marker of resistance in population studies.30
Drug Import
Recently, uptake transporters, especially the organic cation transporter hOCT1, have been the source of investigation for their role in imatinib resistance. Utilizing a number of CML cell lines, Thomas et al demonstrated hOCT1 expression and then, using specific hOCT inhibitors, elicited a reduced receptor-mediated uptake of imatinib, although there were no attempts to correlate the reduced drug levels and a decreased efficacy of imatinib.31 In a follow-up study, White and colleagues demonstrated a differential in-vitro susceptibility to imatinib based upon the expression and function of hOCT1, but the significance is limited by the small sample size and lack of correlative in-vivo data.32 Subsequently, Crossman demonstrated a reduced level of hOCT1 in bone marrow mononuclear cells in patients who had failed to achieve at least a minor cytogenetic response versus those with a CCyR after 10 months of imatinib therapy.30 Other than evaluating for Pgp expression, Crossman did not assess for additional confounding etiologies to explain the imatinib resistance, and the overall cohort was quite small. More recently, a larger evaluation of 70 patients demonstrated a statistically significant difference for CCyR rate at 6 months, PFS and OS based upon the pretreatment hOCT1 expression level.33 The Tyrosine Kinase Inhibitor Optimization and Selectivity (TOPS) trial demonstrated that patients with lower hOCT1 levels had reduced MMR rates at 12 months when receiving the standard-dose imatinib compared with high-dose imatinib.34 Whether this will translate into meaningful differences in the rate of primary imatinib resistance or overall survival is not known.
Drug Binding
Previous mouse models had implicated a possible role for imatinib sequestration in the plasma by the serum protein α1-acid glycoprotein (AGP) as a mechanism of therapy resistance.35,36 Although its primary function remains unknown, AGP has a documented ability to bind basic drugs. In their report, Gambacorti-Passerini et al demonstrated that AGP-bound imatinib in vitro reduced the ability of imatinib to inhibit Abl kinase activity in a dose-dependent manner. Subsequently, elevated plasma AGP concentrations in tumor-bearing mice were associated with progressive disease despite therapy with imatinib, and the AGP competitive binder erythromycin reversed this effect. Although AGP levels were shown to be elevated in patients with CML and further increased with disease progression, Jørgensen et al were not able to demonstrate binding of imatinib to AGP, either derived from normal donors or from the serum of patients with CML.37 A potential explanation for the discrepancy lies with the methods used to isolate the AGP leading to an alteration in the chemical structure, augmenting the capacity of the AGP to recapitulate its in-vivo activity. So while a recent study indicated that plasma AGP concentrations had a marked influence on total imatinib plasma concentrations, the importance of this finding also remains in question due to the lack of clinical data demonstrating variable outcomes based upon patients’ AGP levels.38
Drug Concentration
Recently, several reports have indicated a potential association between trough imatinib concentrations and its correlation with CCyR and MMR rates.39,40 Alternatively, a recent single institution study demonstrated similar trough imatinib concentrations as described by Picard and Larson, yet no differences were seen in those patients obtaining and those failing to obtain a CCyR or an MMR. The duration of therapy prior to the assessment of imatinib trough concentrations as well as differences in pretreatment disease characteristics may limit direct study comparisons. Moreover, since no prospective data exist on the impact of dose intensification in those with suboptimal plasma levels, the importance of imatinib level monitoring will require further validation. As previously reported, intracellular drug concentrations both in the myeloid cell population as well as in the purported stem cell niche may also vary as widely as plasma concentrations, adding additional variables to the equation.30,31,41
Alternative Signaling Pathway Activation
Bcr-Abl–induced cellular transformation alters cellular signaling, cell cycle regulation, and proliferation of hematopoietic progenitor cells by mediating signaling through a number of growth-promoting second messenger systems. The Bcr-Abl protein appears to be able to activate the Ras/Raf/Mek kinase pathway either through Grb-2–mediated binding of the Y177 moiety in the Bcr sequence or through Shc and Crkl, which also bind to the Bcr-Abl gene sequence.42–44 The specific mitogen-activated protein (MAP) kinase(s) that Ras activates in CML remain to be fully described. One potential pathway involves the recruitment of Raf to the cell membrane, which subsequently activates the Mek1/Mek2 and the extracellular receptor regulated kinase (Erk) pathways. Additional studies indicate that Grb-2 can recruit Gab-2 with subsequent activation of both the phosphatidylinositol 3′ kinase (PI3K) and Erk pathways.45 Activation of the Janus kinase (Jak) and subsequent phosphorylation of the signal transducer and activator of transcription (STAT) pathway have also been identified in both Bcr-Abl–positive cell lines and in primary CML cells and may contribute to the transforming ability of Bcr-Abl.46 Several Stat family members including Stat5, Stat1 and Stat3 appear to be activated in both Bcr-Abl–positive cell lines and primary CML cells.47,48 Finally, recent evidence suggests the involvement of activated Erk2, but not Erk1, in the development of imatinib-resistant cell lines.49
Bcr-Abl also induces the activation of the Src family kinases (SFK), which may promote disease progression as well as alter responsiveness to Bcr-Abl–specific therapies. Bcr-Abl directly interacts with SFK and allows the Abl kinase to adopt an open and active conformation, potentially permanently altering the enzyme’s cellular regulation and kinetics.50,51 Phosphorylation of the Bcr-Abl SH2 and SH3 domains by the SFK may increase the activity of the Abl kinase and may alter its susceptibility to imatinib.52 Thus despite the inhibitory effects of imatinib, phosphorylation of key regulatory sequences within the Abl protein sequence may prevent imatinib from completely inactivating the enzyme. Additionally, Bcr-Abl–independent SFK activation may participate in a Bcr-Abl–independent mechanism of imatinib resistance.53–56 While there have been no clinical examples of SFK-activating mutations in imatinib-resistant cell lines or primary CML specimens, cellular activation of this pathway through numerous other cross-talk networks may still facilitate resistance. Recently, Ptasznik and colleagues demonstrated that an antisense RNA for Lyn partially restored imatinib susceptibility.54 However, there is limited clinical validation that inhibition of the SFKs are solely responsible for the clinical activity seen with dasatinib (Sprycel, Bristol-Myers Squibb, New York, New York) in imatinib-resistant patients. If SFK activation alone led to imatinib resistance, then mutations, such as the T315I, would potentially remain dasatinib responsive, and this has yet to be demonstrated.
Epigenetic Modification
Protein function can be governed by a balance of acetylation and deacetylation, much like phosphorylation affects protein activity.57 Alterations in the pattern of acetylation of non-histone proteins can promote abnormal cellular proliferation and resistance to apoptosis, which are important cellular changes in the development of leukemia. A recent manuscript described the development of imatinib resistance in a CML cell line through the concurrent upregulation of Class I and III deacetylases (HDACs) and down-regulation of several histone acetyltransferases (HATs).58 Treatment of these cells with the HDAC inhibitor SAHA restored the acetylation pattern of several proteins and altered the apoptotic threshold. Additionally, the use of HDAC inhibitors together with TKIs showed a synergistic effect on the level of apoptosis in primary cells isolated from CML patients.59,60 However, HDAC inhibitors have yet to be successfully translated into clinical therapies for imatinib-resistant patients.
Therapeutic Options
As previously discussed, approximately 30% of patients may require an alternative treatment to imatinib, either due to disease resistance or medication intolerance. General consensus indicates that patients failing imatinib should be screened for compliance as well as Abl mutations, and either be considered for imatinib dose escalation, a second-generation TKI, or hematopoietic stem cell transplantation (HSCT).6 The optimal therapeutic decision, especially in future research regarding frontline treatment in CML, may rely upon identifying whether resistance is an acquired phenomenon versus a pre-established characteristic of the leukemia. Until this is clarified, however, additional therapeutic options for imatinib-resistant patients are sorely needed and remain an intensive area of investigation (Table 1 ).
Imatinib Dose Escalation
As previously noted, if resistance is an acquired phenomenon due to exposure of leukemia cells to subtherapeutic levels of imatinib, then initial use of higher doses of imatinib may overcome primary resistance. At least five trials to date have assessed the efficacy of higher doses of imatinib (600 mg/day to 800 mg/day) in previously untreated chronic phase patients, but only one has demonstrated an improved transformation-free survival compared with historic control cohorts.61–65 Alternatively, at least two reports to date have evaluated the efficacy of increasing the dose of imatinib in patients with disease that is resistant to standard dose therapy (secondary resistance). Kantarjian recently updated the results of a randomized phase II trial evaluating dasatinib (70 mg twice daily) versus imatinib (400 mg twice daily) in patients failing standard dose imatinib.66 With a minimum follow-up of 2 years, there was no statistical difference in the primary endpoint of an MCyR at 12 weeks (36% for dasatinib vs 29% for imatinib; P = .40), but the rates of MCyR, CCyR and MMR at later time points all favored dasatinib. Moreover, the rates of treatment failure at both 6 months (15% vs 76%) and 15 months (28% vs 82%) both favored dasatinib. Notable improvements in the rate of major cytogenetic responses with dasatinib versus high-dose imatinib were seen in patients failing to have any cytogenetic response with prior imatinib or those failing 600 mg/day of imatinib and improved CCyR rates were also seen in those failing 600 mg/day of imatinib. Jabbour and colleagues recently reported on 84 previously treated, imatinib-resistant CP-CML patients undergoing dose escalation from 400 mg to 800 mg of imatinib (n = 72) or 300 mg to 600 mg of imatinib (n = 12).67 Despite 3-year EFS and OS rates of 47% and 76%, respectively, CCyRs were only seen in 40% of patients, including only 5% of those with a hematologic failure prior to entering the study. After a median follow-up of 5 years, only 30% maintained a CCyR while still receiving imatinib. Several caveats include that 95% of the patients in the report were previously treated with interferon and more than one third had primary refractory disease as defined by failing to achieve any cytogenetic response, thereby limiting the applicability to the majority of CML patients. Both studies indicate that imatinib dose escalation is feasible and can provide durable responses. However, caution is warranted before further dose escalation of imatinib is undertaken, especially in those failing to achieve any cytogenetic response to standard dose imatinib and those progressing on 600 mg per day of imatinib.
Dasatinib (Bristol-Myers Squibb, New York, New York)
Because this multikinase inhibitor is believed to be able to bind Bcr-Abl in both its open/active as well as its closed/inactive conformation, it is also able to bind the Src family kinases (SFK) given their similar geometry to the Abl active conformation. Thus, dasatinib has activity against imatinib-resistant Abl mutations as well as a number of additional tyrosine kinase families potentially involved in mediating imatinib resistance.68 Through the Src/Abl Tyrosine kinase inhibition Activity: Research Trials of dasatinib (START) phase II program, the efficacy of dasatinib has been evaluated in all phases of imatinib-resistant CML. As previously described, the START-R trial evaluated dasatinib 70 mg twice daily versus 400 mg twice daily imatinib in resistant CP-CML patients and demonstrated an apparent advantage to imatinib, mainly in those failing to achieve any cytogenetic response or those failing higher doses of imatinib.66 The START-C trial has also evaluated dasatinib in 288 imatinib-resistant patients. After a median follow-up of 15 months, 87% of patients had achieved a new complete hematologic responses (CHR) and 56% had achieved a new MCyR with an estimated 90% PFS.69
When grouped together, the presence or absence of an Abl kinase mutation does not appear to influence the rates of CHR or MCyR in imatinib-resistant patients receiving dasatinib. However, there are clearly subsets of mutations that appear to be resistant to dasatinib both in vitro as well as in vivo. Six manuscripts have described the outgrowth of new Abl mutations in imatinib-resistant patients receiving second-line dasatinib.70–75 Cortes and colleagues detailed the development and loss of Abl mutations in patients receiving second and third-line therapy (Figure 3 ).71 Jabbour and colleagues recently confirmed equivalent response rates to second-generation TKIs (dasatinib and nilotinib) when imatinib-resistant patients are grouped according to the presence or absence of a mutation, but when segregated according to the actual IC50 of the mutation, patients with CP-CML with mutations demonstrating low IC50 values had statistically better MCyR, CCyR, and PFS compared with those possessing more resistant mutations.76 However, the survival differences did not appear in patients with AP- or BP-CML. The etiology of dasatinib resistance in many patients failing to respond to these second-generation TKIs is potentially independent of the mutations identified and eliciting that actual source is a critically important area of ongoing investigation.
Nilotinib (Tasigna, Novartis, Basel, Switzerland)
Like imatinib, nilotinib appears to target only the inactive conformation of the Abl enzyme, yet it has a higher affinity for the kinase as well as demonstrated activity against multiple imatinib-resistant mutations. Cellular import of nilotinib may not be mediated by hOCT1, but it does appear to be a substrate for Pgp.77 Nilotinib has been evaluated in a number of phase II trials in patients with chronic and accelerated phase disease. A report on approximately 220 imatinib-resistant CP-CML patients was recently updated, indicating a 56% MCyR rate and a 41% CCyR rate after a minimum follow-up of 19 months.78 Importantly, more than three quarters maintained their MCyR at 24 months with a reported PFS of 50% to 60%. Like dasatinib, the mechanisms involved in mediating nilotinib resistance remain unknown in many clinical cases. As previously discussed, new Abl mutations have been described in imatinib-resistant patients receiving nilotinib as either second- or third-line treatment (Figure 3 ).70,71 In population studies, the presence or absence of a KD mutation does not appear to influence the MCyR rate, yet there is a correlation in individual cases between the Bcr-Abl nilotinib IC50 and the MCyR rate.79 Nilotinib-resistant cell lines have also demonstrated Pgp over expression, Abl amplification and Lyn kinase activation, which may signal why these cells remain sensitive to dasatinib.77 However, the mechanism responsible for many clinical cases of nilotinib resistance remains a subject of speculation requiring further research.
Individualized Therapy
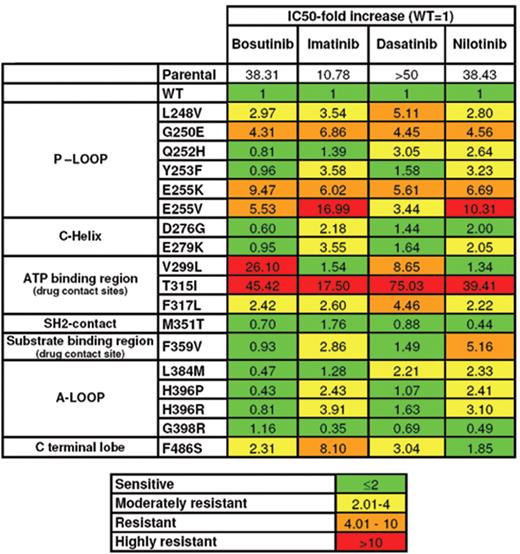
As previously discussed, patients failing imatinib should be screened for compliance, potentially including an assessment of imatinib drug levels. Additionally, mutational assessments should be made to identify possible mechanisms of resistance. Prior phase I and phase II clinical trials as well as case series indicate that patients failing imatinib can often respond to the second- or even third-line TKI-based therapy, including those with and without identifiable KD mutations.66,69–71,73,78,79 Therapeutic decisions may be assisted by knowing the patient’s mutational status, which can evolve over time, and the purported IC50 for each mutation and the associated therapeutic options (Figure 4 ).80 Moreover, clinicians should remember that recurrent mutations commonly develop after specific second-line therapies, including mutations at positions 299 and 317 in those receiving dasatinib, and at positions 253, 255, 311 and 359 in those treated with nilotinib. Therefore, those with pre-existing P-loop mutations may be more susceptible to dasatinib while those with 299 and 317 mutations may benefit from nilotinib. However, a significant number of patients will not have an apparent mutation, and therapeutic decision making will be largely empiric, guided also by known differences in potential side effects of the medications. Additionally, it should be emphasized that the identification of a KD mutation does not absolutely establish the mechanism of resistance. However, individualizing the pharmacodynamics of the mutations together with novel side-effect profiles of the second-generation TKIs may assist clinicians in optimizing treatment decisions.
Experimental Options
A majority of patients with imatinib resistance will never achieve a CCyR with subsequent treatments. Importantly, recent evidence indicates that patients receiving a second-generation TKI and failing to achieve any cytogenetic response at 6 months had only a 10% chance of achieving an MCyR at one year, and those failing to achieve an MCyR 12 months into their therapy have a nearly 20% chance of disease progression over the subsequent year.81 Moreover, no firmly established guidelines exist to assist in therapeutic decisions in these resistant patients. Given that the median duration of responses to third-line therapies ranges from only 3 to 20 months, additional therapeutic options are urgently needed. An impressive array of compounds are currently undergoing preclinical evaluation, but a discussion of all of these exceeds the scope of this review. The following is a brief description of those agents either currently undergoing or having recently completed clinical evaluation in Philadelphia chromosome (Ph)–positive leukemias.
Tyrosine Kinase Inhibitors
Bosutinib (Wyeth, Madison, New Jersey)
This dual Abl/Src inhibitor, with limited activity against c-Kit and the platelet-derived growth factor receptors (PDGFRs), has recently been undergoing phase II testing.82 Approximately 137 primarily imatinib-resistant CP-CML patients have been treated to date, and after a median follow-up of 8 months, 79% have achieved a CHR, with 40% achieving an MCyR, and 29% a CCyR. Ninety-one percent of patients have maintained their MCyR over this brief interval. Utilizing a chemical proteomics approach, Rix and colleagues have indicated the relative specificity of bosutinib and dasatinib for a number of cellular kinases, demonstrating unique profiles for each compound.83 Whether these differences will translate into clinical responses in dasatinib- or nilotinib-resistant patients remains to be determined.
INNO-406 (CytRx, Los Angeles, California)
This orally bioavailable dual Abl/Src inhibitor has an increased affinity to Bcr-Abl compared with imatinib and demonstrates in-vitro activity against a number of Abl mutations but, unlike dasatinib, appears to inhibit only Lyn of the SKFs.84 Mouse models have also demonstrated activity in Ph+ CNS leukemias, especially when combined with cyclosporin A, an inhibitor of the Pgp export pump.85 Previous reports have described the phase I results where 46 imatinib-resistant patients were treated, including 21 with CP-CML, 9 with AP-CML, 7 with BP-CML and 9 with Ph+ ALL.86 CCyR were seen in 3 patients. An expansion cohort of patients being treated at the maximum tolerated dose (MTD) is currently underway at the time of the most recent report.
AP24534 (Ariad, Cambridge, Massachusetts)
As previously described, Abl kinase mutations, including the T315I, are likely responsible for many cases of clinical resistance to TKI-based therapies. The frequency of the identification of a T315I mutation varies based upon the population screened, but may be as high as 15% in imatinib-resistant patients.87 Because available TKIs have no activity against this mutation, a growing number of investigational agents with different modes of activity are being clinically evaluated in this patient population. This multi-kinase inhibitor has demonstrated activity against a number of kinases, including wild-type Bcr-Abl as well as the T315 mutation.88 Utilizing cell lines, it has also demonstrated activity against Flt3, c-Kit, and the fibroblast growth factor receptor (FGFR) family.89 After animal model testing demonstrated activity against wild-type CML as well as a T315I Bcr-Abl cell line, AP24534 has recently begun phase I testing in multiple hematologic malignancies that have relapsed or are refractory to standard care.
Aurora Kinase Inhibitors
XL-228 (Exelixis, South San Francisco, California)
Unlike normal cells, leukemias often contain a number of karyotypic abnormalities, including evidence of aneuploidy. Several serine/threonine kinases, known as mitotic kinases, regulate the transition from G2 through cytokinesis. In humans, the Aurora kinases A and B appear to play a central role in this process, including responsibilities for centrosome duplication, alignment of chromosomes, and mitotic checkpoint arrest.90 Overexpression of these kinases can be oncogenic, but inhibition can lead to aberrant mitosis resulting in mitotic catastrophe in the leukemia cells. XL-228 is a potent multi-targeted protein TKI that has demonstrated nanomolar-range activity against Abl, SFK, insulin-like growth factor receptor 1 (IGFR1), as well as Aurora kinase A.91 Additionally, it appears to have significant in-vitro activity against the T315I mutation. Twenty-seven patients with clinical resistance to imatinib as well as at least one other TKI have been enrolled in a phase I clinical trial and approximately three quarters of patients harbor highly resistant mutations. Dose escalation continues in patients receiving either once- or twice-weekly dosing, but preliminary evidence suggests activity in those receiving 3.6 mg/kg and higher. These include hematologic or cytogenetic response in 7 of 35 (20%) patients, including 3 of the 9 patients with the T315I mutation (1 CCyR, 1 MCyR, and 1 minor cytogenetic response).92
AT9283 (Astex, Cambridge, United Kingdom)
AT9283 is an Aurora kinase A and B inhibitor that also demonstrates nanomolar-range activity against Abl, JAK2, and JAK3.93 In vitro, leukemia cells exposed to AT9283 form large aneuploidal cells, which ultimately undergo apoptosis. Utilizing a continuous 72-hour intravenous infusion, 29 patients with acute leukemia, high-risk myelodysplastic syndrome, and imatinib- and dasatinib-resistant CML have been treated at eight different dose levels. Two of the CML patients demonstrated a hematologic response, including 1 with a PCyR. Based upon clinical and pharmacodynamic data, an investigation utilizing a lower-dose 6-day continuous infusion is reportedly proceeding.
PHA-739358 (Nerivano Medical Sciences, Milan, Italy)
PHA-739358 is also an Aurora kinase A and B inhibitor that has demonstrated in-vitro activity against both wild-type Bcr-Abl and the T315I mutation.94 Preclinical data also suggested activity against Bcr-Abl CD34+ CML progenitor cells from previously untreated patients as well as those derived from imatinib-resistant patients containing the T315I mutation. Preliminary clinical results of a phase II trial reported on 7 patients (1 in chronic phase, 1 in accelerated phase, 5 in blast phase), 6 of whom bore the T315I mutation. Two patients (1 CP-CML and 1 AP-CML) had a CHR. The CP-CML patient also had a minor cytogenetic response, and the AP-CML patient had a CCyR and a CMR.95 Additional studies are reportedly ongoing to explore alternative dosing schedules.
KW-2449 (Kyowa Hakko Kirin Pharma, Tokyo, Japan)
KW-2449 is also an oral Aurora kinase A inhibitor with concurrent nanomolar range activity against Ab1, Flt-3 and FGFR1.96 In a phase I study, KW-2449 was administered at a range of 25 to 500 mg/day using an every-12-hour dosing scheme for 14-days with a 7- to 28-day rest period. Five imatinib-resistant CML patients were accrued, 3 of whom carried the T315I mutation. One BP-CML patient actually had a disappearance of the T315I clone and an improvement in blast count. Pharmacokinetic and dynamic assessments indicated a rapid half-life requiring termination of the trial, and recently a new phase I/II investigation using doses of 450 mg/day to 800 mg/day in an every 6 to 8 hour dosing scheme is underway in patients with acute myeloid leukemia.97
MK-0457 (formerly VX-680) (Merck, Whitehouse Station, New Jersey)
MK-0457 is also a small-molecule inhibitor of Aurora kinase A and B as well as Jak-2. Interestingly, it also binds to the wild-type as well as multiple Abl kinase mutations, including the T315I, in the nanomolar range. It had previously demonstrated activity against Ph+ cell lines, including those harboring the T315I mutation.98 Based upon these findings, a phase I investigation in patients with treatment-resistant CML and Ph+ acute lymphocytic leukemias was completed and demonstrated hematologic activity in 3 patients with the T315I, including a patient who demonstrated a complete disappearance of the T315I mutation.99 Unfortunately, the project was terminated, apparently after a patient experienced QTc prolongation, and its clinical development remains in doubt.
Apoptosis Modulators
Homoharringtonine (ChemGenex, Victoria, Australia)
Homoharringtonine (HHT) is believed to inhibit protein synthesis as well as induce a disruption of the mitochondrial membrane resulting in a release of cytochrome-c and activation of the caspase system. HHT also mediates alterations in the stability of the anti-apoptotic protein MCL-1, which may also enhance apoptosis. A phase II study is currently evaluating a semisynthetic formulation of HHT in 50 patients with imatinib-resistant CML harboring the T315I mutation. All patients had failed imatinib, and 82% had failed two or more TKIs. Information to date from 30 evaluable patients, including 15 with CP-CML, 10 with AP-CML, and 6 with BP-CML, indicates hematologic and cytogenetic responses in all phases of disease, and the T315I clone has disappeared in 60% of evaluable patients.100
Switch Pocket Inhibitors
DCC-2036 (Deciphera, Lawrence, Kansas)
A recent class of non–ATP competitive multi-kinase inhibitors, termed “switch pocket inhibitors,” has recently entered clinical investigation. These small molecules bind to distinct residues that the Abl kinase uses to undergo the conformational change from the inactive to the active state. Structurally, these agents have the ability to avoid the steric hindrance that is created by the T315I mutation by avoiding the ATP-binding site.101 The lead compound, DCC-2036, inhibits the proliferation of Ph+ cell lines, including those harboring the T315I mutation. Animal models have also suggested significant preclinical activity. A phase I trial for patients with chronic phase CML or Ph+ ALL has recently been initiated in three centers.
Conclusion
It has been 10 years since imatinib revolutionized the concept of molecularly targeted therapies by demonstrating that a small molecule inhibitor of a tyrosine kinase can fundamentally alter the pathobiology of a leukemia. Shortly thereafter, clinical resistance to this TKI developed in a minority of the patients, but investigators have quickly identified numerous potential mechanisms responsible for the failures. Moreover, recent advances have facilitated the development of an impressive number of small molecule inhibitors directed at either the Abl kinase mutations or at alternative kinase pathways that mediate disease resistance. The challenges in treating CML continue, and important research continues in a number of vital arenas including a) identifying those patients at highest risk for resistance at the initiation of therapy, b) altering primary therapeutic strategies to minimize the risk of primary resistance, c) developing novel therapies to treat primary and secondary resistance disease when it does occur, and d) developing therapeutic strategies to eliminate minimal residual disease so that the risk of late-term resistance is eliminated. Given the propensity of leukemia to develop novel mechanisms of resistance, this will be quite a daunting challenge, but the successes to date indicate a much brighter outlook for CML patients than even 5 years ago.
Novel small molecule multi-kinase inhibitors currently undergoing clinical investigation in chronic myeloid leukemia.
| Drug name . | Sponsor . | Histologies under investigation . | Potential drug targets . | Hematology clinical trial registration . |
|---|---|---|---|---|
| *Clinical or laboratory activity against the T315I mutation; (c) completed clinical trial; (t) terminated clinical trial | ||||
| ABL indicates Bcr-Abl (Abelson) kinase; SFK, Src family kinase; KIT, CD117; TEC, Tec protein kinase; STE20, serine/threonine 20 kinase; CAMK2G, calcium/calmodulin-dependent protein kinase (CaM kinase) II gamma kinase; PDGFR, platelet-derived growth factor receptor; FGFR1, fibroblast growth factor receptor 1; IGF1R, insulin like growth factor receptor; JAK, Janus kinase; FLT3, fms-like tyrosine kinase receptor-3; RET, rearranged during transfection kinase; TRK, tropomyosin-receptor-kinase; MCL-1, myeloid cell leukemia sequence 1; TIE2, tyrosine kinase with immunoglobulin-like and EGF-like domains 2; KDR, kinase insert domain receptor A gene. | ||||
| Approved Agents | ||||
| Dasatinib | BMS | ABL, KIT, PDGFR, SFK | FDA approved | |
| Nilotinib | Novartis | ABL, KIT, PDGFR | FDA Approved | |
| Investigational Agents | ||||
| Bosutinib | Wyeth | CML, breast cancer | ABL, CAMK2G SFK, STE20, TEC | Phase I/II/III NCT00574873 NCT00261846 INNO-406 |
| (NS-187) | CytRx | CML, Ph+ ALL | ABL, KIT, LYN, PDGFR | Phase I/II NCT00352677 (c) |
| AP24534* | Ariad | CML, advanced hematologic malignancies | ABL, FGFR1, FLT3, KIT, VEGFR | Phase I NCT00660920 |
| XL228* | Exelixis | CML, Ph+ ALL, lymphoma, myeloma, solid tumors | ABL, Aurora A, FGFR1–3, IGF1R, SRC | Phase I NCT00464113 |
| AT9283 | Astex Therapeutics | CML, AML, ALL, MDS, myelofibrosis, NHL, solid cancers | ABL, Aurora A&B, FLT3, JAK2, JAK3 | Phase I/II NCT00522990 |
| PHA739358* | Nerviano Medical Sciences | CML, myeloma, prostate | ABL, Aurora A&B, FGFR1, RET, TRK | Phase II NCT00335868 |
| KW-2449* | Kyowa Hakko Kirin Pharma | CML, AML | ABL, Aurora A, FGFR1, FLT3 | Phase I NCT00346632(t) Phase I/II NCT00779480 |
| MK-0457* | Merck | CML, ALL, MDS | ABL, Aurora A&B, FLT3, JAK2 | Phase I/II NCT00111683(c) |
| Homoharringtonine (HHT)* | ChemGenex | CML | cytochrome C, MCL-1 | Phase II NCT00375219 NCT00462943 NCT00114959 (c) |
| DCC2036* | Deciphera | CML, Ph+ ALL | ABL, FLT3, KDR SFK, TIE2 | Phase I NCT00827138 |
| Drug name . | Sponsor . | Histologies under investigation . | Potential drug targets . | Hematology clinical trial registration . |
|---|---|---|---|---|
| *Clinical or laboratory activity against the T315I mutation; (c) completed clinical trial; (t) terminated clinical trial | ||||
| ABL indicates Bcr-Abl (Abelson) kinase; SFK, Src family kinase; KIT, CD117; TEC, Tec protein kinase; STE20, serine/threonine 20 kinase; CAMK2G, calcium/calmodulin-dependent protein kinase (CaM kinase) II gamma kinase; PDGFR, platelet-derived growth factor receptor; FGFR1, fibroblast growth factor receptor 1; IGF1R, insulin like growth factor receptor; JAK, Janus kinase; FLT3, fms-like tyrosine kinase receptor-3; RET, rearranged during transfection kinase; TRK, tropomyosin-receptor-kinase; MCL-1, myeloid cell leukemia sequence 1; TIE2, tyrosine kinase with immunoglobulin-like and EGF-like domains 2; KDR, kinase insert domain receptor A gene. | ||||
| Approved Agents | ||||
| Dasatinib | BMS | ABL, KIT, PDGFR, SFK | FDA approved | |
| Nilotinib | Novartis | ABL, KIT, PDGFR | FDA Approved | |
| Investigational Agents | ||||
| Bosutinib | Wyeth | CML, breast cancer | ABL, CAMK2G SFK, STE20, TEC | Phase I/II/III NCT00574873 NCT00261846 INNO-406 |
| (NS-187) | CytRx | CML, Ph+ ALL | ABL, KIT, LYN, PDGFR | Phase I/II NCT00352677 (c) |
| AP24534* | Ariad | CML, advanced hematologic malignancies | ABL, FGFR1, FLT3, KIT, VEGFR | Phase I NCT00660920 |
| XL228* | Exelixis | CML, Ph+ ALL, lymphoma, myeloma, solid tumors | ABL, Aurora A, FGFR1–3, IGF1R, SRC | Phase I NCT00464113 |
| AT9283 | Astex Therapeutics | CML, AML, ALL, MDS, myelofibrosis, NHL, solid cancers | ABL, Aurora A&B, FLT3, JAK2, JAK3 | Phase I/II NCT00522990 |
| PHA739358* | Nerviano Medical Sciences | CML, myeloma, prostate | ABL, Aurora A&B, FGFR1, RET, TRK | Phase II NCT00335868 |
| KW-2449* | Kyowa Hakko Kirin Pharma | CML, AML | ABL, Aurora A, FGFR1, FLT3 | Phase I NCT00346632(t) Phase I/II NCT00779480 |
| MK-0457* | Merck | CML, ALL, MDS | ABL, Aurora A&B, FLT3, JAK2 | Phase I/II NCT00111683(c) |
| Homoharringtonine (HHT)* | ChemGenex | CML | cytochrome C, MCL-1 | Phase II NCT00375219 NCT00462943 NCT00114959 (c) |
| DCC2036* | Deciphera | CML, Ph+ ALL | ABL, FLT3, KDR SFK, TIE2 | Phase I NCT00827138 |
Proposed mechanisms of imatinib resistance. 1) Denotes duplication or amplification of the Bcr-Abl sequence; 2) Denotes mutations in the Bcr-Abl sequence; 3) denotes imatinib export by the P-glycoprotein export protein; 4) denotes import of imatinib by the hOCT1 protein; 5) denotes binding of imatinib in the plasma by α1-acid glycoprotein (AGP); 6) denotes variability in the plasma level of imatinib; 7) denotes activation of alternative signaling cascades leading to Bcr-Abl independent growth; and 8) denotes alterations in the epigenetic regulation of the expression of the Bcr-Abl sequence.
Proposed mechanisms of imatinib resistance. 1) Denotes duplication or amplification of the Bcr-Abl sequence; 2) Denotes mutations in the Bcr-Abl sequence; 3) denotes imatinib export by the P-glycoprotein export protein; 4) denotes import of imatinib by the hOCT1 protein; 5) denotes binding of imatinib in the plasma by α1-acid glycoprotein (AGP); 6) denotes variability in the plasma level of imatinib; 7) denotes activation of alternative signaling cascades leading to Bcr-Abl independent growth; and 8) denotes alterations in the epigenetic regulation of the expression of the Bcr-Abl sequence.
The figure represents the frequency ofAblkinase domain mutations detected in clinical specimens from 245 patients with mutations (219 with CML and 26 with Ph+ acute lymphoblastic leukemia). The numbering on the X-axis represents the amino acid location and the letters inside the circles indicate the amino acid encoded by the mutated nucleotide. On the Y-axis, the percentage of patients with each mutation is color-coded as shown in the box. The data is derived from 20 published papers as detailed in the primary manuscript.9 This research was originally published in Blood. Hughes T, Deininger M, Hochhaus A, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108:28–37. © the American Society of Hematology.
The figure represents the frequency ofAblkinase domain mutations detected in clinical specimens from 245 patients with mutations (219 with CML and 26 with Ph+ acute lymphoblastic leukemia). The numbering on the X-axis represents the amino acid location and the letters inside the circles indicate the amino acid encoded by the mutated nucleotide. On the Y-axis, the percentage of patients with each mutation is color-coded as shown in the box. The data is derived from 20 published papers as detailed in the primary manuscript.9 This research was originally published in Blood. Hughes T, Deininger M, Hochhaus A, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108:28–37. © the American Society of Hematology.
Mutations developing in patients with imatinib-resistant Ph+ leukemia treated with second-generation tyrosine kinase inhibitors (TKIs). A) New Abl kinase mutations were detected in 61 imatinib-resistant CML patients and the position and frequency of each mutation is outlined in the graph. B) Imatinib-resistant patients (either with or without preexisting Abl kinase mutations received therapy with a second generation TKI (dasatinib, nilotinib, or SKI-606 [bosutinib]) and the subsequent development or loss of mutations are described. A smaller subset went on to receive therapy with a third TKI as indicated. C) The location and frequency of the development or loss of Abl kinase mutations with second/third line TKI therapy are further characterized.63 This research was originally published in Blood. Cortes J, Jabbour E, Kantarjian H, et al. Dynamics of BCR-ABL kinase domain mutations in chronic myeloid leukemia after sequential treatment with multiple tyrosine kinase inhibitors. Blood. 2007;110:4005–4011. © the American Society of Hematology.
Mutations developing in patients with imatinib-resistant Ph+ leukemia treated with second-generation tyrosine kinase inhibitors (TKIs). A) New Abl kinase mutations were detected in 61 imatinib-resistant CML patients and the position and frequency of each mutation is outlined in the graph. B) Imatinib-resistant patients (either with or without preexisting Abl kinase mutations received therapy with a second generation TKI (dasatinib, nilotinib, or SKI-606 [bosutinib]) and the subsequent development or loss of mutations are described. A smaller subset went on to receive therapy with a third TKI as indicated. C) The location and frequency of the development or loss of Abl kinase mutations with second/third line TKI therapy are further characterized.63 This research was originally published in Blood. Cortes J, Jabbour E, Kantarjian H, et al. Dynamics of BCR-ABL kinase domain mutations in chronic myeloid leukemia after sequential treatment with multiple tyrosine kinase inhibitors. Blood. 2007;110:4005–4011. © the American Society of Hematology.
IC50values for bosutinib, imatinib, dasatinib, and nilotinib against 18 mutations of the Bcr-Abl sequence expressed in Ba/F3 transfected cells. IC50, relative concentration of the compound that inhibits 50% of the enzymes activity; WT, wild type; P loop, phosphate-binding loop; ATP, adenosine triphosphate; SH2, Src homology 2; A loop, activation loop. This table was originally presented in the Journal of Clinical Oncology. Redaelli S, Piazza R, Rostagno R, et al. Activity of bosutinib, dasatinib, and nilotinib against 18 imatinib-resistant BCR/ABL mutants. J Clin Oncol. 2009;27:479–471. The data is also available at www.ilte-cml.org/TKI-table.pdf. © The Journal of Clinical Oncology.
IC50values for bosutinib, imatinib, dasatinib, and nilotinib against 18 mutations of the Bcr-Abl sequence expressed in Ba/F3 transfected cells. IC50, relative concentration of the compound that inhibits 50% of the enzymes activity; WT, wild type; P loop, phosphate-binding loop; ATP, adenosine triphosphate; SH2, Src homology 2; A loop, activation loop. This table was originally presented in the Journal of Clinical Oncology. Redaelli S, Piazza R, Rostagno R, et al. Activity of bosutinib, dasatinib, and nilotinib against 18 imatinib-resistant BCR/ABL mutants. J Clin Oncol. 2009;27:479–471. The data is also available at www.ilte-cml.org/TKI-table.pdf. © The Journal of Clinical Oncology.
Disclosures Conflict-of-interest disclosures: DB receives grant support from Novartis Pharmaceuticals. MT reports that he is on the speakers bureau for Novartis and receives grant support from Novartis, Bristol-Myers Squibb, Exelixis, and Merck. Off-label drug use: None disclosed.
References
Author notes
Division of Hematology and Oncology, Department of Internal Medicine, University of Michigan, Ann Arbor, MI
Department of Internal Medicine, University of Michigan Comprehensive Cancer Center, Ann Arbor, MI

![Figure 3. Mutations developing in patients with imatinib-resistant Ph+ leukemia treated with second-generation tyrosine kinase inhibitors (TKIs).
A) New Abl kinase mutations were detected in 61 imatinib-resistant CML patients and the position and frequency of each mutation is outlined in the graph. B) Imatinib-resistant patients (either with or without preexisting Abl kinase mutations received therapy with a second generation TKI (dasatinib, nilotinib, or SKI-606 [bosutinib]) and the subsequent development or loss of mutations are described. A smaller subset went on to receive therapy with a third TKI as indicated. C) The location and frequency of the development or loss of Abl kinase mutations with second/third line TKI therapy are further characterized.63
This research was originally published in Blood. Cortes J, Jabbour E, Kantarjian H, et al. Dynamics of BCR-ABL kinase domain mutations in chronic myeloid leukemia after sequential treatment with multiple tyrosine kinase inhibitors. Blood. 2007;110:4005–4011. © the American Society of Hematology.](https://ash.silverchair-cdn.com/ash/content_public/journal/hematology/2009/1/10.1182_asheducation-2009.1.461/2/m_talpaz_fig3.jpeg?Expires=1770369285&Signature=wxaw8w5WsvFp6U2olHNl6j~10X0GSOfLgJUtsKKSmdEhAiVGlFINXv81TsDwMmdqsuqkrhTTwvZiZmHzXU-UJIsVf1VjMm3rDZrNqv5zyDQ-IVf9CjOyy~pfUnZYPRbKlLa48QNUm8PjIAupn~MmFDqYgOX3XL6iUHfYd3vgATpdIr27WuBO3N2aVEHYd~FVd7~QpQoux6q9fkRo~jQSXryyQO22N9Dbp6zeaYNqTHSsf3LHdWXKb1Ofh~LNOE61eCnwGuiavCaKlKSGh61XSLTSt0BuF1HrhZORCQx7SwnZv1kMh6iDj9Vyoga2R5t4~7y6MvdX4bpBXCoOgiiRiw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)