Abstract
Cryopreserved umbilical cord blood (UCB) from 4-6/6 HLA-A,B antigen and DRB1 allele matched unrelated neonatal donors contains sufficient numbers of hematopoietic stem cells (HSC) to engraft most younger pediatric patients with leukemia. Recent data demonstrate promising results in larger children and adults, as well as in patients with nonmalignant disorders. As a result, the number of UCB transplantations (UCBT) being performed is increasing dramatically. UCB has the clear benefits of rapid availability and a reduced stringency of requirement for HLA match. The latter attribute has the potential to extend the donor pool, which is of great importance for racial and ethnic minorities. Furthermore, new preparative regimens combined with double-unit grafts have been associated with improved engraftment and survival in larger children and adults, making UCBT a viable potential alternative to unrelated volunteer donor transplantation, especially in preference to transplantation using mismatched volunteers. This review summarizes the current status of unrelated donor UCBT and describes both the challenges and current areas of research associated with this HSC source.
Introduction
Despite there being many millions of registered donors on global unrelated volunteer registries, due to the complexity of human histocompatibility, as well as the logistical challenges of donor availability, unrelated volunteer registries are limited in their ability to provide a prompt hematopoietic stem cell (HSC) source for many patients, with most ethnic minorities not having ready access to suitable donors.1,2 Further, it has been estimated that increased minority recruitment will have only a modest effect on the ability to improve HSC availability1 and is unlikely to be feasible or cost effective. Finally, despite decades of clinical investigation, HLA mismatch is frequently associated with high transplant-related mortality (TRM).3 Even with the use of fully matched donors, graft-versus-host disease (GVHD) remains a significant challenge, particularly in older adults and especially with the use of unmodified peripheral blood HSC regardless of recipient age.
Unrelated donor umbilical cord blood (UCB) has the potential to resolve these limitations for many patients. UCB is capable of reconstituting hematopoiesis after myeloablative4,5 or reduced-intensity/nonmyeloablative therapy.5–8 Unrelated donor public UCB banking programs have been initiated in many countries around the world, with an estimated 250,000 units banked for public use and an estimated 8000 unrelated donor UCB transplantations performed to date.4 Multiple studies in patients with hematologic malignancies have demonstrated that cryopreserved UCB from 4-6/6 HLA-A,B antigen and DRB1 allele matched unrelated donors contains sufficient numbers of HSC to engraft most pediatric patients.4,5 While the early experience of UCBT in larger children and adults was associated with very high TRM,9,10 more recent data demonstrate promising results in larger children and adults,5,11 as well as in patients with nonmalignant disorders.4,5 As a result, the number of UCBT being performed in the U.S. is increasing dramatically2 (Figures 1A and 1B; see Color Figures, page 510). While UCB has both potential benefits and limitations (summarized in Table 1 ), two clinical benefits deserve emphasis. Firstly, UCB is a cryopreserved HSC source that is rapidly available without the risk of donor unavailability, and transplantation can be scheduled almost entirely according to patient needs rather than donor availability. This can be highly advantageous for some patients. Perhaps more important, for a given degree of HLA match there is a decreased incidence of GVHD compared with that seen after transplantation of unrelated volunteer HSC4,5,12 yet a graft-versus-malignancy (GVM) effect is retained.13 Recent single-institution data suggests that this reduced stringency of required HLA match permits an extension of transplantation access to patients of non-northwestern European origin (Table 2 ). While the full extent to which this is true is not currently known, it is clear that UCB can offer transplantation to patients without any suitable unrelated donors. This review discusses the current status of unrelated donor UCBT. While challenges in UCBT remain, the recent improvements in the outcome of UCBT set the stage for the debate: when is UCBT an alternative to the use of unrelated volunteer donors?
Cell Dose and HLA Match: Impact on UCBT Outcome
Cell dose
A chief limitation of UCB is the low total nucleated cell (TNC) dose/kg recipient body weight. Multiple studies have demonstrated the devastating impact of low cell dose upon engraftment, TRM, and survival, especially in larger children and adults.4,5 For example, Wagner et al reported a TRM in excess of 70% for recipients of myeloablative single unit transplants with an infused CD34+ dose of less than 1.7 × 107/kg.9 Similarly, limited cell dose was, in retrospect, a major contributor to the relatively low survival in the first U.S. adult UCBT series published by Laughlin.10 While single-institution series have shown considerably better outcomes after myeloablative single-unit UCBT,14 even rivaling the survival after sibling donor transplantation in one series,15 it is clear that the problem of low cell dose in a single UCB unit must be resolved for adult patients. Eurocord has recommended that units less than 3 × 107 TNC/kg not be used.4 However, this would exclude most U.S. adult patients from undergoing UCBT. Clearly, other strategies are needed to make UCB widely applicable, especially in the U.S. where the average weight of adult patients is high.
HLA match
Due to the clearly adverse impact of low TNC upon engraftment and survival, and the fact that most UCBTs to date have involved either 5/6 or 4/6 HLA-A,B antigen, DRB1 allele-matched UCB units, the importance of HLA match has been less appreciated than that of cell dose. However, analyses by the National Cord Blood Program at the New York Blood Center (NYBC) involving larger numbers of patients, including those receiving 6/6 or 3/6 matched units, have demonstrated a significant adverse impact of HLA mismatch upon engraftment, GVHD, TRM and disease-free survival (DFS) independent of TNC dose.16 Interestingly, the NYBC has reported that no TNC dose effect can be demonstrated after transplantation of 6/6 A,B antigen, DRB1 allele–matched UCB units.16 This suggests that, in the range of cell dose tested (0.7 - >10 × 107 TNC/kg), HLA match can largely compensate for low dose. Though the statistical power supporting this conclusion is limited by small patient numbers to date, this is a very important observation that should be closely investigated in the future. In addition, the NYBC has shown that units with unidirectional mismatches in the direction of GVHD (“no rejection mismatch”) provide engraftment, TRM, and survival rates comparable with 6/6 HLA matched units, also with no cell dose effect.16
Eurocord analyses have also demonstrated that increasing HLA mismatch adversely affects engraftment.4 However, mismatch was also associated with a reduction in malignant relapse. This has therefore negated a significant effect of 1-2 antigen HLA mismatch on DFS in hematologic malignancies in the Eurocord analyses. In contrast, these investigators have confirmed a progressively worse survival with increasing HLA mismatch in patients with nonmalignant disorders.4 The reasons for the differing findings between the NYBC and Eurocord data in relation to the effect of mismatch upon malignant relapse and DFS are unclear; it is a critical research question for the field. Regardless, the recognition of the importance of HLA match adds increased complexity to UCB unit selection where both TNC dose and HLA-A,B antigen and DRB1 allele match must be carefully considered. Further, the threshold of an “adequately dosed” single unit cannot be defined in isolation, as this is dependent upon the HLA match. Therefore, it may be most appropriate to use a “sliding scale” strategy in unit selection. This means the less well-matched the unit, the greater the cell dose needed to ensure a successful transplantation outcome. Eurocord investigators have suggested an algorithm of 6/6 > 3, 5/6 > 4, and 4/6 > 5 × 107 TNC/kg, respectively, for the “satisfactory single.”4 This algorithm, while reasonable, still needs prospective and independent validation.
Strategies to Improve UCBT in Adults
As with any new transplantation therapy, early investigations of adult UCBT have been hindered by a high proportion of patients with advanced disease, with disease status being a major variable affecting transplantation success.17 Nonetheless, both the low cell dose and the inability of some adults to tolerate high-dose conditioning are major limitations of adult UCBT that must be resolved.
Double-unit grafts to augment cell dose
Given most patients that have one 4-6/6 HLA-matched UCB unit will have access to a second unit of similar characteristics, the administration of a double-unit graft is a relatively simple strategy to augment graft cell dose. Double unit UCBT after 120 mg/kg cyclophosphamide, 75 mg/m2 fludarabine and 1320 cGy total body irradiation (TBI) with cyclosporine-A and mycophenolate mofetil (CSA/MMF) has been associated with improved engraftment and reduced TRM as compared to single-unit historic controls,11 with a DFS at 1 year of 72% (95% confidence interval [CI]: 49–95) in patients with leukemia who underwent transplantation in remission. This is despite the fact that one unit was responsible for sustained donor engraftment, and this unit had a relatively low median TNC count of 1.8 × 107/kg. These data have recently been updated by the University of Minnesota, demonstrating a DFS of 54% (95% CI: 42% to 66%) at 3 years in 83 patients with high-risk or advanced hematologic malignancies treated with myeloablative conditioning (Figure 2 ). Such outcomes therefore support double-unit UCBT as a valid potential alternative to unrelated volunteer donor HSC for adult patients. However, the lower limit of cell dose for each unit in the graft is yet to be defined. Most transplantation centers would not permit transplantation of less than 1.5 × 107 TNC/kg/unit, and some larger patients will not have such units available.
Reduced-intensity or nonmyeloablative UCBT
Reduced-intensity or nonmyeloablative UCBT has been investigated as an approach to extend the potential benefits of allograft to those of older age, with extensive prior therapy, or with significant comorbidities.6,8,18 Brunstein et al have recently updated nonablative UCBT outcomes using a cyclophosphamide/fludarabine/200 cGy TBI regimen with CSA/MMF and predominantly double-unit grafts. This study demonstrated a 3-year survival of 45% in 110 adults (median age, 51 years) with advanced hematologic malignancies.18 Notably, this group has shown that the presence of comorbidities is a critical determinant of transplantation outcome, with a 3-year transplantation survival of 8% versus 56% according to the presence or absence of significant comorbidities, respectively, after nonablative UCBT.19 Ballen et al have investigated a reduced-intensity regimen of fludarabine, melphalan, rabbit antithymocyte globulin (ATG) and CSA/MMF with a double-unit UCBT in 21 adults with hematologic malignancies or severe aplastic anemia.8 Day 100 TRM after this regimen was relatively low at 14%, with a promising 1-year DFS of 67%. These reports and those of others (reviewed in Brunstein and Wagner19) confirms that UCBT is an option for patients unsuitable for ablative conditioning.
UCBT for Nonmalignant Diseases
UCBT has also been investigated for metabolic storage diseases and may be associated with favorable improvement in the natural history of these disorders,20 although in some subtypes transplantation prior to the onset of symptoms is required.21 Importantly, both the rapid availability and the low incidence of chronic GVHD after UCBT make this an extremely attractive HSC source for treatment of those young patients in whom cell dose is not a major limitation. Reports in immunodeficiencies are also starting to emerge.22,23 While only small series of outcomes of UCBT for severe aplastic anemia (SAA) and hemoglobinopathies have been reported, Mao et al have demonstrated sustained DFS in 7 of 9 patients with SAA, and Jaing et al have shown sustained donor engraftment in 5 of 5 patients who underwent transplantation for β-thalassemia major, suggesting UCBT can be considered as therapy in such patients who are without a suitably matched unrelated volunteer donor.24,25 UCBT in such patients, however, will clearly be associated with a significant risk of graft rejection and will therefore likely benefit from the investigation of novel preparative regimens such as that described by Mazur et al.26
Comparisons of Unrelated Donor UCB and Bone Marrow
No randomized trials have compared the transplantation of unrelated volunteer donors and UCB. While these are currently being considered by the U.S. Bone Marrow Transplantation (BMT) Clinical Trials Network (CTN), the logistics of such a study will be extremely challenging. However, a retrospective analysis has recently compared the outcomes of 4-6/6 HLA-A,B antigen and DRB1 allele-matched single-unit UCBT with those of 8/8 allele-matched unrelated volunteer donor transplantations in children younger than 16 years with leukemia (Table 3 ).13 This analysis revealed significantly superior 5-year DFS after 6/6-matched UCBT (n = 35) compared with the gold standard of 8/8 allele matched bone marrow (BM) (n = 116). Further, the DFS after 5/6 (n = 201) or 4/6 (n = 267) matched UCBT was comparable to the transplantation of 8/8 allele matched BM. Notably, compared with 8/8 allele-matched BMT, TRM was comparable in matched and high cell dose (> 3 × 107 TNC/kg) 5/6-matched UCBT. Further, while TRM was higher in recipients of low cell dose (< 3 × 107 TNC/kg) 5/ 6 and 4/6 (any cell dose) UCBT, relapse was lower, accounting for the lack of difference in DFS compared with BM recipients. These results support the use of HLA-matched or mismatched UCBT in children with leukemia.
The outcome of adult single-unit myeloablative UCBT recipients (in which the median infused TNC count was 2.2 × 107/kg) has been compared with recipients of unrelated donor BM by Laughlin et al.27 The limitation of low cell dose likely contributed to an inferior hematopoietic recovery and increased TRM in UCBT recipients (n = 150) as compared with that of 6/6 HLA-matched unrelated volunteer BM recipients (n = 367). However, DFS after UCBT was comparable with that of HLA-mismatched BM recipients (n = 83), introducing UCBT as a valid alternative to the use of HLA-mismatched volunteer donors in adults. Notably, a similar comparison by Eurocord revealed comparable DFS after HLA-matched unrelated donor BM transplantation (n = 584) and HLA-mismatched UCBT (n = 98) despite UCBT recipients having more advanced disease.12 UCBT recipients had inferior engraftment and less grade II-IV acute GVHD, whereas chronic GVHD, TRM, and relapse were no different. Two-year DFS for recipients of UCBT and BMT were 43% (95% CI: 33–53) and 49% (95% CI: 45–53) if in first remission (P = .31); 44% (95% CI: 32–56) and 47% (95% CI: 43–50) if in second remission (P = .64); and 23% (95% CI: 17–29) and 19% (95% CI: 16–22) if advanced disease (P = .92). Of great interest for the future will be comparisons of double-unit ablative UCBT with matched and mismatched unrelated donor HSC transplantations including recipients of mobilized peripheral blood and the comparison of these grafts after nonablative conditioning.
Current Areas of Research and Development
A wide variety of aspects of UCB banking, biology, and transplantation practice are currently being investigated.
UCB banking
A major question from the viewpoint of UCB banking, and its associated funding, is how big must the UCB inventory be to guarantee access to UCB units of at least 5/6 match for all patients? While preliminary experience suggests that UCB does extend transplantation access to patients of non-northwestern European ancestry, the full extent of this benefit is not known. The NYBC16 and the American Red Cross28 have demonstrated that the creation of ethnically diverse UCB inventories is possible. However, the NYBC has also shown that African-American patients are the least likely of any group to find a suitable UCB unit.16 Sophisticated analyses that incorporate match and dose will be required to make estimates of the size of the optimal inventory. Ethical aspects associated with this issue are further discussed by Katz-Benichou.29
A further issue in UCB banking is unit quality. Although it is estimated that there are already approximately 250,000 units banked worldwide, it is not clear as to how many of these are of both sufficient size and quality to be suitable for transplantation. Transplantation centers have found that unit quality can vary from unit to unit and bank to bank. McCullough et al evaluated 268 units from banks in the U.S. and Europe and, alarmingly, discovered quality issues in 56%, with 10% of these considered to be likely associated with patient risk.30 How unit quality should be regulated is currently being debated.
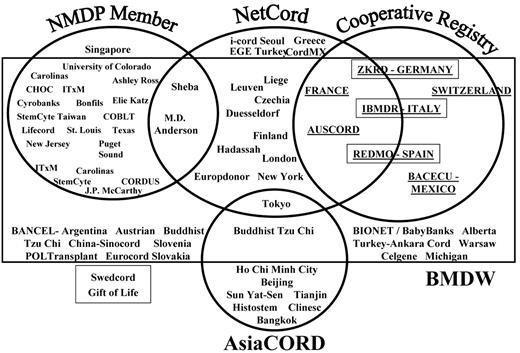
Notably, there have been major developments in the funding and organization of the infrastructure that orchestrates the acquisition of and access to UCB in the U.S. This has been facilitated by the “Stem Cell Therapeutic and Research Act of 2005,” which authorizes at least $79 million to collect 150,000 new UCB units and supports the creation of a national cord blood program in the U.S. It is hoped that this will facilitate the UCB search process. The navigation of UCB searches is highly complex, as highlighted in Figure 3 . The promises of and challenges associated with reforming this process are highlighted by Atlas31 and Rubinstein.2
Cell dose vs HLA match in unit selection and strategies to augment engraftment
One of the major controversies in the field is how to “trade off” dose versus match in UCB unit selection. Data from the NYBC suggest that a twofold increase in TNC dose is required to compensate for the adverse impact upon TRM and survival of increasing mismatch in 4/6 as compared with 5/6 UCBT recipients.16 However, in larger children and adults, such a magnitude of increase is usually not possible. One alternative strategy currently being investigated in a U.S. multicenter study is to prioritize HLA match over dose in unit selection (above a threshold of 1.5 × 107 TNC/kg/unit) but to augment graft cell dose by infusing 2 units. In addition, the importance of factors beyond TNC dose and HLA-A, -B antigen and DRB1 allele match will need to be elucidated. Such variables include whether the unit is red blood cell (RBC) depleted, the CD34+ dose, HLA-A and -B match at high resolution, matching at HLA-C, whether there is an attached segment for confirmatory typing, the age of the unit, which bank the unit comes from, and the availability of back-up units in the case of a problem at thaw or in the event of graft failure.
However, in transplantation practice the biggest question (beyond optimal unit selection) remains, how can we guarantee UCB engraftment? To this end, a multicenter trial of double-unit UCBT in adults is under way sponsored by the Center for International Blood and Marrow Transplant Research (CIBMTR). In addition, a phase 3 randomized study of single- versus double-unit UCBT in children is being conducted by the BMT CTN to investigate if an advantage of double-unit UCBT can be seen in children, and whether the potential benefit seen with double-unit UCBT can be attributed to the addition of fludarabine and MMF (and/or the removal of ATG and corticosteroids). Other strategies being pursued include: (1) the use of T-cell–depleted haplo-identical grafts from a third party as a “bridge” to abrogate neutropenia until a single UCB unit engrafts (phase 2 clinical studies)14; (2) ex vivo expansion (phase 1/2 clinical studies);32–34 or (3) intra-bone marrow injection (phase 1/2 clinical studies).35 Whether these strategies will demonstrate benefits over double-unit UCBT with both units unmanipulated will be of great interest. Alternatively, if better unit selection, improved conditioning, and/or double-unit grafts overcome the engraftment barrier, the field may turn to ex vivo expanded lymphocytes to augment immune reconstitution.36,37
UCBT outcome in specific malignancies
A further area of interest is the outcome of UCBT in specific diseases especially after reduced-intensity or non-myeloablative regimens, which have been investigated in a wide variety of diagnoses. Barker et al have reported a progression-free survival of 63% in 16 patients with advanced follicular or mantle cell non-Hodgkin lymphoma or chronic lymphocytic leukemia. Brunstein et al have reported a 2-year survival of 31% in 43 nonmyeloablative UCB transplant recipients with high-risk acute myelogenous leukemia, which was comparable with the 32% survival of 21 patients receiving sibling donor transplants with similar diagnoses. Such reports will facilitate assessment of the potency of the UCB GVM effect in specific diagnoses as well as assist in the development of measures to improve disease-specific outcomes. Patients with myelodysplasia or myelofibrosis who have not had prior chemotherapy are frequently unsuitable for high-dose myeloablation and yet are at a high risk of graft rejection after nonmyeloablative conditioning.38 Research is required as to how to optimize conditioning to ensure both engraftment and disease eradication in patients with these diagnoses.
GVHD, infection and relapse
A unique aspect of UCBT is the less than expected severity of GVHD. Studies to understand the biology of this phenomenon are ongoing.39 Meanwhile, clinical investigators have reported that the chronic GVHD after UCBT is more responsive to treatment and associated with a lower TRM than after unrelated volunteer transplantation.40 Equally important is the nature of the immune reconstitution and opportunisitc infections associated with UCBT.41 Szabolcs et al have found that infections, particularly viral infections, are the major cause of death after UCBT and usually occur in the first 100 days after transplantation.41 Interestingly, Parody et al have reported that while UCBT was associated with a higher frequency of severe infections in the first 3 years compared with unrelated donor BM or peripheral blood HSC recipients (85% vs 69% vs 67%, respectively), there was a similar risk of infection related death in all 3 groups.42 Clearly, very aggressive supportive care and prophylaxis is critical in UCB transplant recipients, especially in the first post-transplantation months. An important research focus is to understand who is most at risk41 and ultimately how immune reconstitution in these patients may be enhanced.
The understanding of UCBT immune reconstitution takes on an even greater importance given the report of Parkman et al, who found that patients with a proliferative response against herpes group viruses had a lower risk of leukemic relapse after UCBT.43 Interestingly, there is also a suggestion that double-unit UCBT may be associated with less relapse than single-unit UCBT.44 Exactly how this could be mediated is a current research priority. Other anti-leukemia strategies currently being investigated include the use of UCB-derived T cells expressing chimeric antigen receptor to target B-cell malignancies45 or the use of UCB-derived NK cells.46
Conclusions
The US General Accounting Office Report in October 2002 documented that more than 10,000 patients per year in the US need an unrelated donor HSC transplantation and do not receive one. UCB has the potential to nearly resolve the limitations of search time, donor availability, and the lack of suitably matched donors for many patients. However, given the importance of HLA match as well as dose, the “UCB promise” will only be realized if there is a sufficient increase in the size of the global UCB inventory, and this is going to require substantial funding of public UCB banks.
UCBT is currently considered by many as a valid potential alternative for any patient who requires an unrelated donor allograft and who is without a suitably matched and readily available volunteer. Some transplantation centers now give UCB the priority as the unrelated HSC source of choice in children and, albeit less frequently, also in adults. Others conduct a simultaneous search for both unrelated volunteers and UCB, thus offering UCB as an immediate potential alternative to unrelated volunteers.47 It is possible that UCB (particularly 5-6/6 HLA-matched) may become the preferred HSC source even for those patients with fully matched unrelated volunteer donors. Finally, assuming we can increase the global UCB inventory, UCB is likely the best way to extend transplantation access to minorities; thus, in the future we may be able to offer an HSC source to all.
Benefits and limitations of umbilical cord blood (UCB) as a hematopoietic stem cell (HSC) source compared with unrelated volunteer donors (URD).
| Benefit of UCB . | Comparison with URD . |
|---|---|
|
|
| Limitation of UCB | Comparison with URD |
|
|
| Benefit of UCB . | Comparison with URD . |
|---|---|
|
|
| Limitation of UCB | Comparison with URD |
|
|
Ancestry of 28 umbilical cord blood (UCB) transplant recipients at Memorial Sloan-Kettering Cancer Center 10/1/05-8/7/07. Patients were offered UCB transplantation if allogeneic transplantation was indicated and no suitably matched related or unrelated volunteer donor was available (n = 26). Although potential 10/10 matched unrelated volunteer donors were identified for both of the 2 patients of Northwestern European ancestry, they each received UCB due to transplantation urgency (n = 1) and patient preference (n = 1). UCB units were 4-6/6 HLA-matched at A and B antigens and DRB1 alleles.
| Patient ancestry . | N . |
|---|---|
| Northwestern Europe | 2 |
| African American | 5 |
| Asian | 3 |
| Middle Eastern | 1 |
| Central/South American | 6 |
| Southern Europe | 3 |
| Eastern Europe | 3 |
| Mixed | 5 |
| Patient ancestry . | N . |
|---|---|
| Northwestern Europe | 2 |
| African American | 5 |
| Asian | 3 |
| Middle Eastern | 1 |
| Central/South American | 6 |
| Southern Europe | 3 |
| Eastern Europe | 3 |
| Mixed | 5 |
Comparison of outcomes after 8/8 allele-matched unrelated donor bone marrow and 4-6 A,B antigen, DRB1 allele matched umbilical cord blood transplantation (UCBT) in children with acute leukemia.13 Survival data is reported at 5 years after transplantation.
| HSC Source . | TRM, % . | Relapse, % . | LFS, % . | OS, % . |
|---|---|---|---|---|
| 8/8 matched BM (n = 116) | 19 | 41 | 38 | 45 |
| UCB (n = 503) | ||||
| 6/6 | 6 | 34 | 60 | 63 |
| 5/6 > 3.0 × 107 NC/kg | 29 | 31 | 41 | 45 |
| 5/6 < 3.0 × 107 NC/kg | 43 | 21 | 37 | 36 |
| 4/6 | 49 | 20 | 33 | 33 |
| HSC Source . | TRM, % . | Relapse, % . | LFS, % . | OS, % . |
|---|---|---|---|---|
| 8/8 matched BM (n = 116) | 19 | 41 | 38 | 45 |
| UCB (n = 503) | ||||
| 6/6 | 6 | 34 | 60 | 63 |
| 5/6 > 3.0 × 107 NC/kg | 29 | 31 | 41 | 45 |
| 5/6 < 3.0 × 107 NC/kg | 43 | 21 | 37 | 36 |
| 4/6 | 49 | 20 | 33 | 33 |
Probability of disease-free survival after myeloablative double unit umbilical cord blood transplantation (UCBT) (n = 83). Slide courtesy of Dr John Wagner, University of Minnesota.
Probability of disease-free survival after myeloablative double unit umbilical cord blood transplantation (UCBT) (n = 83). Slide courtesy of Dr John Wagner, University of Minnesota.
Global umbilical cord blood (UCB) banks and their relationship to UCB registries. (Slide courtesy of Mary Halet, NMDP).
Global umbilical cord blood (UCB) banks and their relationship to UCB registries. (Slide courtesy of Mary Halet, NMDP).
Memorial Sloan-Kettering Cancer Center, New York, NY