Abstract
Successful blood and marrow transplant (BMT), both autologous and allogeneic, requires the infusion of a sufficient number of hematopoietic progenitor/stem cells (HPCs) capable of homing to the marrow cavity and regenerating a full array of hematopoietic cell lineages in a timely fashion. At present, the most commonly used surrogate marker for HPCs is the cell surface marker CD34, identified in the clinical laboratory by flow cytometry. Clinical studies have shown that infusion of at least 2 × 106 CD34+ cells/kg recipient body weight results in reliable engraftment as measured by recovery of adequate neutrophil and platelet counts approximately 14 days after transplant. Recruitment of HPCs from the marrow into the blood is termed mobilization, or, more commonly, stem cell mobilization.
In Section I, Dr. Tsvee Lapidot and colleagues review the wide range of factors influencing stem cell mobilization. Our current understanding focuses on chemokines, proteolytic enzymes, adhesion molecules, cytokines and stromal cell-stem cell interactions. On the basis of this understanding, new approaches to mobilization have been designed and are now starting to undergo clinical testing.
In Section II, Dr. Michele Cottler-Fox describes factors predicting the ability to mobilize the older patient with myeloma. In addition, clinical approaches to improving collection by individualizing the timing of apheresis and adjusting the volume of blood processed to achieve a desired product are discussed. Key to this process is the daily enumeration of blood CD34+ cells. Newer methods of enumerating and mobilizing autologous blood HPCs are discussed.
In Section III, Dr. John DiPersio and colleagues provide data on clinical results of mobilizing allogeneic donors with G-CSF, GM-CSF and the combination of both as relates to the number and type of cells collected by apheresis. Newer methods of stem cell mobilization as well as the relationship of graft composition on immune reconstitution and GVHD are discussed.
I. Current Understanding of Factors Influencing Stem Cell Mobilization
Tsvee Lapidot, PhD,* Isabelle Petit, PhD, and Orit Kollet, PhD
The Weizmann Institute of Science, Rehovot 76100, Israel
Acknowledgments: Special thanks go to Drs. Michele Fox, Luen Bik To, and Josef Vormoor for fruitful discussions and for critical reviews of this manuscript.
Recruitment of hematopoietic stem and progenitor cells to the blood following treatment with chemotherapy, or cytokines, is a clinical process termed mobilization. This process mimics enhancement of the physiological release of stem cells and progenitors from the bone marrow (BM) reservoir in response to stress signals during injury and inflammation. Currently, mobilized cells are the preferable and major source of stem and progenitor cells harvested for autologous and allogeneic transplantations because of the higher yield of these cells, leading to faster engraftment and decreased procedural risks compared with harvested BM cells. The emerging picture of stem cell mobilization involves interfering with the physiological interplay between mesenchymal stromal and hematopoietic cells regulating both bone and BM remodeling processes, which also mediate stem/progenitor cell proliferation and migration. The mobilization process is initiated by stress-induced activation of neutrophils and osteoclasts by chemotherapy and repeated stimulation with cytokines such as granulocyte colony-stimulating factor (G-CSF), resulting in shedding and release of membrane-bound stem cell factor (SCF), proliferation of progenitor cells, as well as activation and/or degradation of adhesion molecules such as VLA-4 and P/E selectins. The dynamic secretion and inactivation of the chemokines stromal cell derived factor-1 (SDF-1)/CXCL12 and interleukin-8 (IL-8)/CXCL8, and multiple cycles of inactivation and degradation of BM components by proteolytic enzymes, such as elastase, cathepsin G, proteinase 3, CD26, and various matrix metalloproteinases (MMPs), are implicated as major players in progenitor mobilization. These mechanisms will be reviewed in this section.
The road to stem cell mobilization began in the 1960s, with publication of a few reports documenting the presence of hematopoietic stem cells in the peripheral blood of mice, dogs, and monkeys, followed by reports revealing low levels of progenitors in the human circulation during steady-state homeostasis. However, steady-state progenitors in the circulation of mice were shown to be inferior to BM as a source of repopulating stem cells. More important, although sporadic clinical transplantations documented successful hematopoietic recovery, in most cases graft failure was detected in autologous, syngeneic, and fully matched related allogeneic transplantations, using steady-state peripheral blood cells. Moreover, the first successful human blood leukocyte transplantations were not better than BM as a source of repopulating stem cells (reviewed in Korbling and Fliender1 and To et al2). While the levels of human progenitors in the circulation during steady-state homeostasis are low, they are significantly elevated in patients with myeloproliferative disorders.3 Similarly, a transient increase in circulating progenitors was documented in dogs treated with dextran sulfate and humans treated with endotoxin or other stress-inducing mobilization agents. These encouraging results were followed by preliminary reports in the late 1970s documenting increased levels of progenitors in the circulation of patients after chemotherapy treatment with cyclophosphamide and other drugs. Technical improvements including in vitro colony assays and the availability of large-scale harvesting of human progenitors by continuous-flow leukopheresis enabled closer examination of chemotherapy-/druginduced mobilization in treated patients.1,2 In the early 1980s, To and colleagues reported high levels of progenitors in the circulation of leukemia patients in early remission.2 Clinical studies by this group were the first to document the beneficial faster repopulation in patients transplanted with autologous mobilized peripheral blood (PBL). Initially, the mobilization protocols were based on chemotherapy alone. However, after the discovery of human G-CSF by Welte et al,4 mobilization protocols began to include G-CSF, which today is the standard mobilizing agent.2
Definitive, Repopulating Stem Cells Are Migrating Cells
During late embryonic development, both human and murine stem cells migrate via the blood circulation from the fetal liver to the BM and repopulate this tissue with high levels of immature and maturing cells. These in turn are released into the circulation, while a small pool of undifferentiated stem and progenitor cells within the BM is maintained throughout life. Prior to their localization in the murine fetal liver, hematopoietic stem cells can be isolated from the aorta-gonad-mesonephros (AGM) region and the yolk sac even before completion of blood circulation development.5 However, some of these stem cells are not definitive, since they cannot rescue and repopulate lethally irradiated recipients because of their inability to migrate in the host circulation and home to and repopulate the BM. These predefinitive stem cells isolated from the murine yolk sac can still engraft the liver of newborn mice preconditioned as fetuses with chemotherapy if the predefinitive stem cells are directly injected into this organ.6 Furthermore, an additional maturation step provided to predefinitive progenitors isolated from the AGM region, in the form of in vitro incubation on stromal cells and stimulation with cytokines, shifts these cells into definitive stem cells with functional migration, homing, and repopulation potential.5 Murine embryos that lack the chemokine SDF-1 or its receptor CXCR4 have multiple lethal defects, including impaired seeding of the fetal BM (reviewed in Lapidot and Petit7). We have shown the essential roles of SDF-1/CXCR4 interactions in a functional, preclinical model for human stem cells using non-obese diabetes severe combined immune deficient (NOD/SCID) mice as recipients. Homing and repopulation in both primary and serially transplanted mice with human CD34 stem cells was dependent on CXCR4 signaling,8,9 which is dynamically expressed by human progenitors.10 Moreover, SDF-1-mediated migration of human CD34 cells in vitro correlated with their in vivo repopulation potential in transplanted patients.11 In conclusion, stem cell motility (migration, homing, and release) is essential for BM repopulation and for the development of the hematopoietic system.
Hematopoietic Stem Cells in the Circulation Can Home Back to the BM
The role of circulating stem cells in steady-state homeostasis is currently unknown. While some progenitors are needed for seeding of the thymus, which requires migration of lymphocyte precursors from the BM, this process is markedly reduced in adult life.12 Stem cells migrate also to nonhematopoietic organs such as the liver, especially during liver injury/inflammation, creating an alarm situation and transmitting stress signals that mobilize and recruit stem cells as part of organ repair.13 Ramshaw et al suggest that circulating stem cells can reengraft the BM, documenting successful engraftment of unconditioned murine recipients transplanted with high doses of BM cells.14 In support of this approach, Wright et al elegantly demonstrated rapid clearance of intravenous transplanted mouse stem cells from the murine circulation within a few minutes. By using genetically marked parabiotic mice with a shared circulation, they showed that the low levels of circulating stem cells can durably reengraft the BM, suggesting continuous release and reengraftment of the BM as sequential events taking part in physiological processes.15 In parallel, Abkowitz et al, using the same parabiotic model, revealed only low levels of reengrafted stem cells with secondary recipient repopulation potential (1%–2.5%) in the partner BM as opposed to high levels of progenitors in the spleen. These investigators suggest the release of stem cells into the circulation functions also as an apoptotic pathway for the BM to regulate excess amounts of progenitors because of limited numbers of stem cell niches.16 Of interest, these investigators also applied G-CSF- and SCF-induced mobilization to the parabiotic mice pairs, documenting a dramatic 4- to 10-fold increase (from 1%–2.5% to 10.1%) in the levels of reengrafted stem cells with secondary repopulation potential in the partner BM. These results demonstrate that inducing the release of stem cells in response to stress signals also increases their homing back and reengraftment of the stimulated/stressed BM, confirming the repopulation potential of mobilized progenitors harvested for clinical protocols. These results also support the hypothesis that tissue repair of damaged BM can be supported by intensified homing and reengraftment of circulating hematopoietic stem cells, in response to stress signals, which is similar to migration of mature leukocytes to sites of inflammation as part of the immune system host defense. The concept of BM niches occupied by stationary, quiescent stem cells may be an oversimplification of a more dynamic situation. Higher proliferative and migratory turnover of definitive, repopulating stem cells involves their release into the circulation, migration, homing, and reengraftment of the BM as part of their physiological development. Bradford et al revealed that even the most primitive murine stem cells in the BM must cycle at least once every 30 days.17
Bone and BM Remodeling Processes Are Mutually Regulated
Proliferation and release of hematopoietic stem and progenitor cells require dynamic cycles of BM destruction/restructuring, which seem to be linked to bone remodeling by osteoclast/osteoblast interactions. Moreover, both processes are likely to be orchestrated by the same factors. For example, continuous G-CSF treatment to prevent neutropenia has also been shown to induce osteoporosis in some juvenile patients with severe congenital neutropenia18 and in transgenic mice that overexpress this cytokine.19 More important, there is a dramatic increase in the number of murine osteoclasts in response to repetitive G-CSF stimulation, leading to osteoclast-mediated bone resorption during stem cell mobilization and calcium release, which can induce detachment of hematopoietic progenitors from fibronectin in vitro.20 Unexpectedly, treatment of mice with pamidronate, an inhibitor of osteoclast-mediated bone resorption, together with G-CSF increased the levels of mobilized progenitors in the murine circulation.20 Osteoclasts secrete high levels of IL-8, a mobilization-inducing chemokine.21,22 Another chemokine, SDF-1, which also participates in G-CSF–mediated mobilization, induces osteoclasts to secrete the metalloproteinase MMP-9.23 This enzyme is involved in stem cell mobilization by shedding the membrane-bound cytokine SCF within the BM and releasing this cytokine into the circulation.24 MMP-9 also induces migration of osteoclasts to the cortical bone, adjacent to the SDF-1 and stem cell–rich endosteum region, to form resorption pits.23,25 These results suggest that the role of osteoclasts in mobilization could be related to the rapid increase in their numbers and to the secretion of chemokines and proteolytic enzymes. Activation and secretion of proteolytic enzymes lead to cleavage and degradation of the BM extracellular matrix, adhesion molecules, cytokines, and chemokines and therefore facilitate transendothelial migration and stem cell release from the BM.7 These processes mediate both peripheral bone and medullar BM remodeling as well as stem cell proliferation and release by inactivating the BM microenvironment. Subsequently, stem cells migrate via the circulation, home back to the BM, and repopulate the damaged/destructured sites in this organ as part of tissue repair and the continuous replenishment of the blood with new immature and maturing hematopoietic cells of all lineages, while maintaining a small pool of undifferentiated stem and progenitor cells within their renewed BM niches. In support of this hypothesis, by applying complementary DNA array technology, 2 recent studies revealed high expression of the proteolytic enzyme proteinase 3 and low expression of a proteinase 3 inhibitor in isolated human BM CD34 cells compared with enriched mobilized CD34 cells isolated from G-CSF-treated healthy donors.26,27 These results suggest that proteinase 3, with its ability to cleave connective tissue in the BM, is needed for maintaining a niche for hematopoietic stem and progenitor cells. Recent findings document that proteinase 3 also cleaves the cell cycle checkpoint p21, inducing cells to enter the cell cycle.28 This could explain the higher levels of cycling BM CD34 cells compared with the more quiescent mobilized PBL CD34 cells.26,27 Immature mesenchymal bone-forming osteoblasts lining the stem cell–rich endosteum region secrete high levels of SDF-1.25 In response to stimulation with this ligand, hematopoietic stem cell–derived osteoclasts secrete MMP-9.23,24 Thus, peripheral periosteal bone and medullar BM destruction and remodeling are sequential events mediated by the same factors, i.e. MMP-9, G-CSF, SCF, IL-8, and SDF-1, which regulate both new bone formation and stem cell self-renewal, migration, and development.
Stress-Induced Mobilization of Stem and Progenitor Cells
Applying single or multiple stress signals interferes with steady-state homeostasis, creating an alarm situation leading to increased release of immature and maturing hematopoietic cells from the BM into the blood circulation, which occurs naturally during inflammation and injury. For example, increased levels of G-CSF and other cytokines secreted by long-distance runners during marathons cause blood leukocytosis, in particular higher levels of CD34/CD38-positive committed progenitor cells, but not more primitive CD38-negative stem cells compared with control individuals, reflecting adaptation of BM activity to stress induced by extensive exercise.29 Increased cell release from the BM reservoir is part of the immune system host defense during inflammation as a result of infection- or injury-mediated release of stress signals. This release is induced clinically or in animal models by a wide range of molecules and/or treatments: DNA damaging, single chemotherapeutic drugs such as cyclophosphamide (Cy), or combined chemotherapy regimens such as iphosphamide, carboplatin and etoposide (ICE) and etoposide, methylprednisolone, ara-c and cisplatin (ESHAP); cytokines such as G-CSF, granulocyte-macrophage colony-stimulating factor (GM-CSF), SCF, and flt-3 ligand; and chemokines such as IL-8, Mip-1α, Groβ, and SDF-1.7 These molecules differ in their mode of administration, the time frame needed to achieve mobilization, the type of cells mobilized, and the efficiency. G-CSF, the most commonly used mobilization agent, is usually administered daily at a dose of 5–10 μg/kg for 5–10 days, alone or after chemotherapy.2 However, a substantial number of patients, especially patients having extensive chemotherapy that leads to BM aplasia, older patients, and a minority of healthy individuals, are poor mobilizers.7 For example, increasing age and longer intensive chemotherapy treatment in old multiple myeloma patients inversely correlate with successful mobilization.30 These patients are usually treated with higher doses of G-CSF, GM-CSF followed by G-CSF, or a combination of G-CSF and SCF. Recently, it was reported that some chronic myeloid leukemia (CML) patients treated with high doses of imatinib (Glivec, STI 571) suffer hematological toxicity and can develop drug-induced neutropenia.31 In addition, some treated patients failed to mobilize well, requiring discontinuation of the drug during the mobilization process and the addition of SCF to G-CSF, to successfully overcome the poor mobilization.32 However, while SCF stimulation increases the levels of mobilized CD34 progenitors, this treatment also has side effects such as allergic reaction due to activation of mast cells. These studies stress the need to identify and characterize the mechanisms of stem cell mobilization in order to develop better strategies for poor mobilizers. Chemotherapy followed by repetitive G-CSF–induced mobilization is a multistep process. Anchorage of stem and progenitor cells to the BM microenvironment by activation of adhesion interactions, which are facilitated by membrane-bound SCF or SDF-1, needs to be disrupted.33 Papayannopoulou elegantly demonstrated that the integrin VLA-4 plays a critical role in stem cell mobilization since anti-VLA-4 antibodies prevent adhesion molecules expressed on the surface of hematopoietic progenitors from binding their ligand VCAM-1 expressed by stromal cells. This induces rapid mobilization of primate and murine stem cells, which also involves signaling via the c-kit receptor.33 Moreover, as a result of inactivation during the mobilization process, mobilized CD34 cells have lower levels of VLA-4 and c-kit expression compared with BM progenitors.26,27 In addition, sulfated polysaccharides such as Fucoidan lead to rapid mobilization of progenitors34 since they compete for adhesion interactions with selectins and for SDF-1 binding to the BM endothelium via its nonsignaling C-terminus, inducing inactivation of selectin interactions as well as release of SDF-1 into the circulation. Levesque et al revealed increased release of elastase and cathepsin G within murine BM during Cy- and G-CSF–induced mobilization; peak levels were reached during stem cell egress.35 These enzymes cleaved VCAM-1 expressed by stromal cells, preventing adhesion of progenitors via VLA-4 as part of the mobilization process.
In addition to their distinctive adhesive properties, mobilized CD34 progenitors differ from their BM counterparts in several ways. Besides reduced VLA-4, c-kit, and CXCR4 expression, a significantly higher percentage of mobilized progenitors are noncycling quiescent cells.26,27 Prior to mobilization, hematopoietic progenitors proliferate within the BM, and this feature could involve proteinase 3–mediated cleavage of p21 in response to neutrophil stimulation.28 Mobilized progenitors have higher levels of the proapoptotic genes caspase 3, 4, and 8 and reduction in inhibitors of apoptosis such as antiproteinase 2, compared with human BM CD34 cells,26 supporting the hypothesis of Abkowitz et al that release into the circulation may also serve as an apoptotic pathway for stem cells.16 Enhanced repopulation documented with mobilized progenitors is due to significantly higher cell doses, in particular committed progenitors, which lead to faster neutrophil and platelet recovery.7 However, better leukemia-free survival and overall survival were recently documented in acute myeloid leukemia (AML) patients transplanted with increased cell doses of matched BM cells compared with lower doses of BM cells and more important, also compared with high cell doses of matched mobilized PBL, suggesting BM as a superior source of stem cells for HLA-identical allogeneic transplantations.36 New protocols aimed at increasing the levels of long-term repopulating stem cells as the major source while maintaining short-term repopulating cells need to be developed.
SDF-1/CXCR4—Key Regulators of Stem Cell Homing and Mobilization
Mobilized human CD34 progenitors express reduced levels of the SDF-1 receptor CXCR4, which correlates with improved mobilization,11,37 suggesting involvement of SDF-1/CXCR4 interactions in the mobilization process. Overexpression of SDF-1 in the murine circulation leads to stem cell mobilization.38 In functional preclinical animal models for human stem cells such as preimmune sheep and immune-deficient NOD/SCID mice, mobilized CD34 cells are inferior in their repopulating potential compared with similar cell doses of CD34 cells obtained from human BM. This is most probably due to their reduced levels of surface CXCR4, which is needed for SDF-1–mediated directional homing and repopulation in transplanted mice and increased levels of short-term repopulating cells.7 These results should be interpreted with caution, since short-term stimulation with human SCF upregulated surface CXCR4 expression on human CD34 cells and murine SCF is much less potent in stimulating human progenitors.8,39 In addition, other factors such as complement C3a improve SDF-1–mediated directional migration of human progenitors and the in vivo homing of murine progenitors. However, some of these factors can be species-specific or absent in immune-deficient mice.40 Of interest, priming of mobilized human progenitors by several inflammatory molecules improves their chemotactic responses to SDF-1.41 We have demonstrated increased levels of SDF-1 production in the murine BM in response to DNA-damaging chemotherapy drugs, including Cy and 5-fluorouracil (5-FU), most probably to prevent cell death since this chemokine is also a survival factor for stem cells.25,42,43 Rafii and Hattori et al demonstrated that the increased levels of SDF-1 in response to stress-mediated 5-FU mobilization in mice induce release of MMP-9, which cleaves and releases membrane-bound SCF, leading quiescent stem cells to proliferate in the BM prior to their mobilization into the circulation.24 SDF-1 mediates secretion of MMP-2 and MMP-9 from human CD34 cells,44 and these proteolytic enzymes inactivate SDF-1 by cleaving a few amino acids in the N terminus.45 We demonstrated that each injection of G-CSF stimulates mesenchymal cells such as immature osteoblasts to secrete SDF-1, leading to a transient increase in SDF-1 levels within the BM. This oscillating increase is followed by a profound decrease due to inactivation by proteolytic enzymes, mostly by neutrophil elastase, with the lowest levels of this ligand released during cell mobilization.46 Levesque et al reported that in addition to inactivation of BM SDF-1 by elastase and cathepsin G, these proteolytic enzymes can also cleave part of the CXCR4 receptor N terminus in the BM,47 partially inactivating SDF-1 signaling and directional migration. Of interest, neutrophils secrete the proteolytic enzymes elastase, cathepsin G, and proteinase 3 in response to G-CSF, and neutrophil elastase also inactivates G-CSF,48 which is essential for regulating release of neutrophils from the BM. However, expression of G-CSF receptors by neutrophils is not required because of an indirect mechanism that involves proteolytic reduction of SDF-1 within the murine BM.49 Of interest, the central role of elastase in regulating release of BM leukocytes is suggested by inherited genetic mutations in the elastase gene, leading to 2 forms of neutropenia in juvenile patients (severe congenital neutropenia, or Kostmann disease, and cyclic neutropenia) that require continuous treatment with G-CSF.7 CD26, another proteolytic enzyme that inactivates SDF-1, is expressed by human CD34 progenitors and is involved in G-CSF–induced mobilization in mice.50
A role for CXCR4 signaling in cell egress from the BM to the circulation emerges from several studies. We found that in parallel to gradual reduction of BM SDF-1 during G-SCF administration, CXCR4 expression is elevated within the human and murine BM, reaching peak levels at the time of mobilization.46 While some CXCR4 inhibitors also lead to release of human progenitors,51 and treatment with pertussis toxin, which blocks Gαi-mediated signaling in 7 transmembrane G coupled receptors such as CXCR4, induced mobilization in mice,52 SDF-1/CXCR4 interactions are also needed for cell egress. Treatment of mice with G-CSF and neutralizing anti-CXCR4, anti-SDF-1 Ab, or inhibitors of CD26 reduced the mobilization levels.46,50 Finally, warts, hypogammaglobulinemia, immunodeficiency and myelokathexis (WHIM) syndrome, a rare inherited immunodeficiency disease associated with mutations in CXCR4, is characterized by neutropenia and B-cell lymphopenia. In one case, an affected individual was born with cardiac malformation, resembling the murine model in which knocking out CXCR4 or SDF-1 results in a lethal phenotype associated with lack of BM seeding, B-cell development, and cardiac septum formation.53 Thus, SDF-1/CXCR4 interactions may have a role in the regulation of the routine and active egress of progenitor and maturing cells from the BM into the circulation.
Taken together, these results decipher key mechanistic insights into stress-induced mobilization that mimic and amplify naturally occurring recruitment of progenitors during alarm situations. We suggest the BM as a reservoir for immature and maturing hematopoietic cells to be released into the circulation upon stress signals, to migrate to injured sites, and to contribute to host defense and tissue repair. The steady-state balance in the BM is disrupted, leading to transient increased production of SDF-1, and proliferation and activation of neutrophils and osteoclasts. Release of proteolytic enzymes is followed by shedding of membrane-bound SCF, proliferation of hematopoietic progenitors, increasing surface CXCR4 expression and inactivation of SDF-1, G-CSF, the BM adhesion machinery, and extra cellular matrix (ECM). These events are intensified in each cycle of stimulation by G-CSF, eventually leading to release of progenitors into the circulation (Figure 1 contains a model of the process; see Appendix, page602). A better understanding of the process by which progenitors egress from the BM will eventually lead to the development of improved mobilization protocols, in particular for patients who are poor mobilizers.
Note
Because of the complexity of stem cell mobilization and the wide range of agents inducing this process, we could not discuss many interesting studies, and we apologize to those whose excellent work could not be cited given the space limitations.
II. Mobilizing the Older Patient with Myeloma
Michele H. Cottler-Fox, MD*
Department of Pathology and Myeloma Institute for Research and Therapy, University of Arkansas for Medical Sciences, 4301 W Markham Street, MS 517, Little Rock AR 72205
Individually Optimized Collection of HPCs
Enumeration of HPCs
Variables having an impact on the ability to collect hematopoietic progenitor cells (HPCs) may be donor related or procedure related. Donor-related variables include age, previous chemotherapy, mobilization regimen, and platelet count at the time of mobilization. Procedure-related variables include central access devices as well as variables inherent to the different cell separation devices used. Nonetheless, at present, the basis for optimizing HPC collection is the ability to determine when to start collection, based on the ability to enumerate CD34+ cells in the peripheral blood of a donor/patient on a daily basis. It has been demonstrated repeatedly that the best currently available predictor of an adequate collection is the number of CD34+ cell/μL in the blood on the morning of collection, both for good mobilizers and for poor mobilizers.1–,5 A number of authors have recommended starting collection when a particular number of CD34+ cells/μL is present (usually a number between 8 and 20) in order to increase the likelihood of collecting at least 2–4 × 106 CD34+ cells/kg in a single apheresis, i.e., an acceptable number of HPCs for either one or two autologous transplants or a single allogeneic transplant.6,7
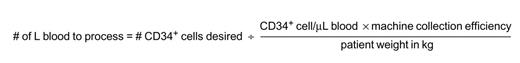
In the past it was important that each center determine a number of its own as the starting point for apheresis, given the historic difficulty in comparing flow cytometry results from center to center.8 At present, however, there are two commercially available single platform tests available for measuring CD34+ cells in blood (ProCount from Becton-Dickinson, Mt View, CA, and StemKit from Beckman-Coulter, Fullerton, CA), so that any center using the same technology should have a reasonable chance of success using the same numbers. More importantly, it is possible to use the number of CD34+ cells/μL obtained using single platform technology in a predictive formula which allows the clinician to know when to start apheresis in order to optimize collection and how many liters of blood need to be processed in order to collect a given number of CD34+ cells9 using the formula in Figure 3 . While results of collection using this formula have only been reported for the COBE Spectra cell separators, it seems likely that it would work with any continuous flow apheresis device if the appropriate value for machine collection efficiency is used.
Sadly, despite the consensus that daily CD34+ cell numbers in the blood are the best currently available predictor for achieving an acceptable HPC collection,8 the practice has not been universally adopted because it is both time consuming and relatively expensive. Alternatives that have been reported to be useful include measuring the number of CD34+ cells in the blood the day before starting collection, with or without the total white cell count, or change in white cell count from the day before apheresis to the day of apheresis,4 and the rapidity of rise in white cell count and platelet count. More recently, the Food and Drug Administration (FDA) has approved the use of an HPC window on an automated cell counter (Sysmex, Kobe, Japan) and this number may be used to predict when to start apheresis.10 The HPC number measured by the Sysmex does not correlate well with CD34+ cell number in the blood (nor does CD133, an antigen expressed by the more primitive CD34+ cells11 [Cottler-Fox et al, in preparation]), but since it is now recognized that not all HPCs express measurable CD3412 it has been presumed that the HPCs measured by the Sysmex include some that are CD34−. Thus, the HPCs measured by Sysmex are available rapidly and less expensively, and may serve as a guide for starting apheresis, but they are difficult to use in the above predictive formula.
HPCs expressing high levels of the enzyme aldehyde dehydrogenase (ALDH) are believed to be pluripotent and generally express CD34 on their surface.13 A commercial assay has now been developed for this intracellular enzyme (Aldecount, Stemco Biomedical, Durham, NC). As this assay detects both CD34+ and CD34− cells, and appears to differentiate viable from non-viable cells,14 its use may eventually lead to a major change in how HPCs are enumerated in transplant grafts.
Timing of apheresis
There is a fall in circulating leukocytes immediately after granulocyte colony-stimulating factor (G-CSF) has been given, with the peak of CD34+ cell mobilization approximately 3–6 hours after each dose is given subcutaneously, paralleling its half-life.15–,17 To optimize collection, it seems reasonable therefore, to wait at least 1 hour after giving the injection, trying to time the duration of the collection for the period which includes the rise in leukocytes and as much of the peak as possible. For example, at least one center routinely waits for 2 hours after the injection, since their average collection lasts about 2–3 hours.5 It is possible that the apparent ability of large volume leukapheresis lasting 4–5 hours to “recruit” CD34+ cells into the blood, reported by several groups but not others,18,19 in fact simply reflects the timing of the apheresis collection relative to the dose of G-CSF. With the arrival of pegylated filgrastim (Neulasta, Amgen, Thousand Oaks, CA) it is possible that the relationship of collection yields relative to the time of dosage will cease to be a factor in collection.
Predicting Who Will Mobilize Poorly
The effect of age has been shown to be a continuous, incremental variable in the myeloma population, with no threshold past which there is an accelerated decline in mobilization of CD34+ cells.20 That is, the older the patient, the fewer stem cells are likely to be collected, but there is no fixed age past which it is impossible to collect HPCs. Over and above age, however, two other variables are statistically significant: number of months of previous chemotherapy and platelet count at the time of mobilization.20 In 85% of myeloma patients over age 70 who had < 12 months of therapy and a platelet count > 200 × 109/L, it was possible to obtain ≥ 4 × 106 CD34+ cells/kg in a single apheresis using individually optimized collection conditions after combined chemotherapy and growth factors. Those patient over 70 years of age with > 12 months of prior therapy and platelets < 200 × 109/L, however, were poor mobilizers.
Choosing a Mobilization Regimen
Mobilization with chemotherapy and growth factors has been shown in a number of settings to be significantly more effective than growth factors alone. Nonetheless, it is often the case that the toxicity of chemotherapy makes this combination less attractive in the fragile older patient. It is therefore important to know that in the subgroup of myeloma patients over the age of 70 who were predicted to be poor mobilizers (> 12 months prior therapy and platelets < 200 × 109/L), as many stem cells were collected with growth factors alone as with chemotherapy and growth factors together. Thus, for this group of patients it seems worthwhile trying to mobilize with growth factors alone in order to avoid toxicity, assuming the disease itself does not require chemotherapy at the time of attempted mobilization.
Current standard agents
G-CSF (filgrastim, Amgen) has become the standard against which all other mobilization agents are measured. This is because it has been shown to both mobilize more CD34+ cells and have less toxicity than any other single agent against which it has been tested to date. It is not completely without toxicity, however, given that there have been deaths attributed to thrombosis (acute myocardial infarction and stroke) in sibling donors,21 possibly related to receptors on platelets for G-CSF.22 Also, a recent study of serial ultrasounds in donors receiving G-CSF prompted by 4 reports of splenic rupture related to G-CSF demonstrated universal enlargement of the spleen during mobilization, with regression of size after discontinuing the growth factor.23,24 Other effects of G-CSF which are shared with granulocyte-macrophage colony-stimulating factor (GM-CSF) include pain, nausea, vomiting, diarrhea, insomnia, chills, fevers, and nightsweats.25,26
GM-CSF (sargramostim, Berlex, Richmond, CA) as a single agent is used less often today for mobilization than G-CSF, because it mobilizes somewhat less well than G-CSF27 and because of a relatively higher incidence of both mild and severe side effects.28 However, the fact that it can be more cost effective, and that there are reports of improved immune reconstitution with GM-CSF relative to G-CSF,29–,32 has caused some clinicians to reconsider its use. Further, for the patient, or normal donor who has failed to mobilize adequately on G-CSF alone, the combination of GM-CSF with or followed by G-CSF has been shown to be efficacious.33– 36
Erythropoietin, now commonly used among cancer patients undergoing chemotherapy to maintain hemoglobin in the near normal range, also has some ability to mobilize CD34+ cells.37 In the hard to mobilize patient, its use may therefore be doubly beneficial.
Alternative agents
Stem cell factor (SCF) has been shown to be an excellent mobilizing agent, particularly when used in combination with G-CSF.38 Unfortunately, the high incidence of allergic reactions to this agent and the need for observation after it is given have made it difficult to move into standard clinical practice. It is not currently available commercially in the US.
Newer agents
Longer lasting variants of G-CSF (pegfilgrastim, Amgen) and erythropoietin (darbopoietin, Amgen) are now available and are in clinical trials as mobilizing agents. They have the benefit of very long half-lives and so add an important measure of patient convenience and the probability that timing of collection may be more flexible without sacrificing optimal collections.
A new factor (AMD3100, AnorMed, Vancouver, Canada), which is a reversible inhibitor of the binding of stromal derived factor (SDF-1a) to its cognate receptor CXCR4, is currently in clinical trials as a mobilizing agent. It is the first agent to be tried for mobilization based on a rational understanding of its mechanism of action relative to HPC-stromal cell interactions (see Section I). While it mobilizes CD34+ cells adequately on its own, it significantly improves the mobilization capacity of G-CSF when used in combination with G-CSF in mice. Clinical trials in humans with various diseases are in progress, including myeloma.
Remobilization
For the patient who fails to mobilize the necessary number of cells for transplant on the first attempt, but for whom it is clear that transplant is the best option, two decisions need to be made simultaneously: when to remobilize, and with what? When to remobilize is still a subject of debate, and depends to some extent on whether the failed mobilization was with chemotherapy plus growth factor or growth factor alone. Although at least one set of authors recommend immediate remobilization with growth factors for a patient who has not mobilized adequately after chemotherapy plus growth factor,39 others feel that at least 2–3 weeks off growth factor prior to remobilization offers the best chance of success.40–,42 If adequate cells are given for an autologous transplant, it is even possible to collect enough for a second transplant during the period of white blood cell recovery following the first transplant.43 It is also possible to collect HPCs at least one year after a prior transplant: of 38 myeloma patients who attempted such a collection, 36 achieved an adequate number of cells for transplant (Cottler-Fox et al, in preparation).
What to use for a repeat mobilization attempt for a specific patient and disease may be a complex decision. However, some general guidelines may be found in the literature. First, mobilization with chemotherapy plus growth factor will generally yield more CD34+ cells than growth factor alone (for the single exception see #2 in the Algorithm for Mobilizing Myeloma Patients below).44,45 Second, chemotherapy plus G-CSF and SCF is more effective than chemotherapy plus G-CSF alone.38 Further, chemotherapy with either sequential or concurrent GM-CSF plus G-CSF may be more effective than G-CSF alone,45 as erythropoietin may improve the response to G-CSF.46 Finally, retrospective analysis of data in myeloma patients from a single institution has shown that for patients who have undergone as many as 4 attempts at mobilization, only 1 of the 4 may yield an adequate collection (Cottler-Fox et al, in preparation). It is possible that AMD3100 will find a niche in this hard to mobilize population: in an ongoing trial at the University of Arkansas for Medical Sciences in myeloma patients who have previously failed to collect at least 5 × 106 CD34+ cells/kg, it provides adequate mobilization in a significant number of patients (Tricot et al, in preparation).
An Algorithm for Mobilizing Myeloma Patients
Although many variables may affect the decision of how and when to mobilize a myeloma patient, the following is a generally useful approach.
Attempt first collection relatively early, i.e., with < 12 months prior therapy.
Attempt collection first with chemotherapy plus growth factor (except for patients over 70 with > 12 months prior therapy and platelets < 200 × 109/L, for whom growth factors alone may be tried first). The choice of growth factor (G-CSF versus GM-CSF) may depend on data under development regarding the importance of early immune reconstitution on time to progression and long-term disease-free survival. Pegylated filgrastim may replace standard G-CSF if studies show it to be equivalent or better than standard G-CSF.
If mobilization is inadequate and
patient is in CR or near-CR: wait at least 3 weeks, then remobilize with combination growth factors. In the future, AMD3100 may be a possibility.
patient is not in CR or near-CR: give planned chemotherapy and combine it with sequential GM-CSF and G-CSF. Consider adding erythropoietin. In the future, AMD3100 may be a possibility.
If patient is not progressing, 3a and/or 3b may be repeated until adequate cells are collected.
If patient is progressing, and adequate cells are available for autologous transplant (≥ 3 × 106 CD34+ cells/kg), monitor CD34+ cells in the blood at the time of leukocyte recovery, and consider collecting HPCs if there is adequate mobilization.
If patient achieves a CR with transplant but does not mobilize adequately to collect during the leukocyte recovery phase post-transplant, consider attempting collection with combination growth factors at least 1 year after transplant.
III. Mobilization of Allogeneic Stem Cells
John F. DiPersio, MD, PhD,* Dan Link, MD, and Steven Devine, MD
Washington University School of Medicine, 660 S Euclid, Box 8007, St Louis MO 63110
General Principles
Although early attempts to use unmobilized peripheral blood stem cells (PBSCs) for autologous stem cell transplantation were problematic, the use of cytokines such as G-CSF to enhance the peripheralization of CD34+ cells and the collection of these stem cells using leukapheresis procedures has become the standard for autologous stem cell transplantation around the world.1 IBMTR and EBMT data suggest that over 80–90% of all autologous stem cell transplants in the world are performed using cytokine or chemotherapy/cytokine mobilized PBSCs as a source of stem cells.2 In addition to reducing patient morbidity, the use of mobilized PBSCs has resulted in higher CD34 content of grafts, shorter hospital stays, and reduced engraftment times for both neutrophils and platelets as well as improved lymphocyte recovery resulting in enhanced immunologic reconstitution when compared to patients receiving autologous BM.3–,6 These beneficial effects of mobilized PBSCs as a source of stem cells for autologous stem cell transplantation have been confirmed in a number of randomized trials.7– 11
Based on the sustained success of using mobilized PBSCs for autologous stem cell transplantation, investigators began to pilot the use of PBSCs for allogeneic stem cell transplantation. Initial concerns focused on the possibility of increased risk of acute and chronic GVHD due to the presence of 10- to 50-fold increased numbers of T cells present in mobilized PBSC products. It was not clear if the function of mobilized allogeneic T cells might be qualitatively altered resulting in even greater risk of GVHD or relapse. In addition, the risk of infusing increased numbers of cytomegalovirus (CMV)-positive granulocytes, dendritic cells, and monocytes into both CMV− and CMV+ recipients remained unknown and potentially posed an increased risk to the recipient. On the other hand, mobilized PBSCs contain 3- to 4-fold more CD34+ cells, which might result in faster engraftment and more efficient transformation to complete donor chimersim.
Early Phase 2 studies demonstrated that G-CSF had a generalized effect on the peripheralization of many different types of allogeneic peripheral blood cells, not just CD34+ cells. These data are consistent with the notion that G-CSF has a generalized effect on remodeling the BM microenvironment, which results in the egress of many types of cells including T cells and monocytes. Activation of neutrophils by cytokines such as G-CSF results in the release of proteases that facilitate the egress of HSCs from the BM microenvironment. Interruption of the G-CSF signal through genetically “knocking out” the G-CSF receptor results in not only the expected elimination of G-CSF-induced mobilization of HSCs but also IL-8- and chemotherapy-induced HSC mobilization in these G-CSF receptor knock-out mice.12,13 Although it is not completely clear which is the most important tether binding HSCs to the microenvironment, LFA-1, VLA-4, CXCR4, and c-kit have all been implicated as critical stem cell adhesion molecules.14–,17 Likewise, a number of neutrophil-specific enzymes have been implicated in mediating critical cleavages that result in stem cell egress from the microenvironment. These include neutrophil elastase, cathepsin G, proteinase 3, gelatinase B (MMP-9), and other metalloproteinases.18–,21 Recent evidence has strongly implicated CD26, a CD34-associated protease, as the prime protease that may cleave SDF-1 off the marrow microenvironment resulting in the release of CD34+ HSCs into the periphery.22 Of interest, a collaborative effort of the Link, Simmons and Levesque laboratories have shown that mice deficient in MMPq, neturophil elastase and cathepsin-G and mice deficient in dipeptidyl peptidase I (CD26) all mobilized hematopietic precursors in response to G-CSF normally. These data question the role of neutrophil specific proteins in stem cell egress (Daniel Link, personal communication).
Effects of G-CSF Mobilization on Allograft Content
Although a number of cytokines and cytokine combinations have been used to mobilize autologous HSCs, only G-CSF and GM-CSF have been approved by the Food and Durg Administration (FDA) for use as autologous stem cell mobilizing agents. Thus, these have been the only cytokines used to mobilize allogeneic PBSCs. The majority of the initial Phase 2 studies using mobilized PBSCs in an allogeneic setting utilized G-CSF (10–16 μg/kg/day for 5 days). Leukapheresis was performed on day 4 or day 5 after G-CSF treatment. Fischmeister et al23 followed CD34+ in the peripheral blood after either G-CSF or GM-CSF treatment and showed that CD34+ cells peaked in the blood between days +4 and +5 for G-CSF and days +5 and +6 after GM-CSF treatment. Data from Seattle suggested that larger doses of G-CSF (16 μg/kg/day) may result in even higher CD34 yields at the time of pheresis on day 5.24 We have assessed the effect of 5 days of of G-CSF (10 μg/kg) on the numbers of leukocyte subsets in the peripheral blood of 100 consecutive normal allogeneic PBSC donors (Figure 3 ; see Appendix, page602). It is clear from these data that G-CSF has a pleiotropic effect of increasing the numbers of circulating neutrophils and monocytes (WBC) as well as T cells (both CD4 and CD8), NK cells and B cells. Korbling and Anderlini compared the allograft content after G-CSF mobilization to cellular contents of BM harvests. These data suggest a 3- to 4-fold enhancement of CD34+ cells and a 10- to 20-fold increase in the number of CD3+ T cells in PBSC products compared to BM harvests.25
Factors Determining Mobilization and Outcomes
It is well known that certain factors may help predict those autologous stem cell recipients who might be expected to be “poor mobilizers.” These include extent of previous treatment, treatment with certain drugs such as nitrosoureas and certain diseases such as Hodgkin’s disease, non-Hodgkin’s lymphomas and preleukemic syndromes. No such data exist for allogeneic donors. We have examined stem cell mobilization from over 400 HLA-matched sibling donors since 1995. Using G-CSF as the sole mobilizing agent, only 2.0% of normal donors mobilized with G-CSF (10 μg/kg/day; 20 L exchange on day 5) did not achieve > 2 × 106 CD34/kg and 25% did not achieve > 5 × 106 CD34/kg after a single collection. These data have been recapitulated by other groups. We have studied the few normal donors who did not achieve > 1 × 106 CD34/kg after 3 collections (1.0% of all normal donors in our data set). All of these donors underwent BM harvests as well but these all yielded < 1.0 × 106 CD34 cells consistent with the notion that these poor allogeneic PBSC mobilizers were not defective in cytokine induced mobization per se but had low levels of BM stem cell reserves. Brown et al26 correlated premobilization PB CD34/mL with G-CSF-induced mobilization. None of the normal allogeneic donors who had < 2000 CD34/mL prior to mobilization yielded > 5 × 106 CD34+ cells/kg while 95% of those normal donors with > 4000 CD34/mL PB yielded > 5 × 106 CD34/kg after G-CSF mobilization. Although provocative, this has not been widely accepted as a method of identifying poor autologous or allogeneic PBSC donors.
In the mid- and late-1990s, a large number of small Phase 2 studies were performed using mobilized PBSCs as a source of HSCs for allogeneic stem cell transplantation. All of these studies yielded similar results. Although neutrophil and platelet recovery was enhanced using cytokine mobilized allogeneic PBSCs, rates of acute GVHD were similar or less than that documented for BM as a source of allogeneic HSCs. The majority, but not all of these early studies, demonstrated increased actuarial rates of limited and extensive26– 28 chronic GVHD (cGVHD). Cost and hospitalization appeared to be reduced compared to patients transplanted using allogeneic BM in these small Phase 2 studies.
Similar to many autologous PBSC studies, the number of allogeneic CD34 cells infused correlated well with both neutrophil and platelet engraftment. Brown demonstrated that those allogeneic PBSC recipients who had > 5 × 106 CD34/kg infused had a 95% chance of both neutrophil and platelet engraftment by day +15.26 In this study, no correlation could be found between GVHD or survival and the number of CD3+ cells infused. In one retrospective study by the MD Anderson group, infusion of > 8 × 106/kg CD34 resulted in decreased survival presumably due to increased rates of cGVHD associated complications.29 These data have not been corroborated by other groups. Therefore, the infusion of high numbers (> 8 × 106 CD34/kg) of allogeneic stem cells remains a controversial negative predictor for outcomes after allogeneic PBSC transplantation.
Effects on Donors
A major question is whether allogeneic stem cell harvesting results in less morbidity than BM harvesting for allogeneic stem cell donors. Anderlini et al30 reviewed 1448 mobilized allogeneic PBSC collections from the IBMTR and EBMT registries. G-CSF was used in > 99% of donors. Similar to multiple Phase 2 studies, 20% of normal donors required placement of a central line for apheresis. Eleven percent required more than 2 leukapheresis procedures and “serious complications” occurred in 1.1% of allogeneic PBSC collection versus 0.5% after BM harvest. Rowley et al31 utilized an 11-point scale (0 = minimum and 10 = maximum) for 23 different symptoms occurring during the first 14 days after either BM or PBSC collection. There were no statistical differences between the PBSC and BM groups for any of the symptom complexes or for the severity of any symptoms.
Randomized Studies
Many of the Phase 2 studies assessing the role of mobilized allogeneic PBSCs on GVHD, relapse and overall survival are limited by design (Phase 2), paucity of patients, short-term follow-up, and heterogeneity of diseases for which allogeneic PBSC transplantation was performed. Several trials have provided insight into the relative effect of PBSC versus BM on GVHD, relapse, and survival. These include randomized studies, case control retrospective studies, and meta-analyses. Table 1 summarizes the results of all randomized trials comparing BM and PB as a source of stem cells for allogeneic stem cell transplantation.32–,38 Half of these trials suffer from low numbers of patients. The 3 largest studies36– 38 demonstrate no significant difference in overall survival when peripheral blood is compared to BM as a source of allogeneic stem cells. These studies, similar to the smaller randomized trials, did demonstrate a significant enhancement in both neutrophil and platelet recovery consistent with the significantly increased numbers of CD34 cells that are harvested in mobilized allogeneic PBSC products compared with BM.
In one of the largest and best-designed studies, Bensinger et al,38 using identical conditioning regimens, GVHD prophylaxis (cyclosporine and methotrexate), and post-transplant growth factor support (no G-CSF), found a slight advantage in both disease-free and overall survival in those patients receiving mobilized allogeneic stem cells versus BM (P = .03 and P = .06, respectively). Although there was no difference in probability of 2-year overall survival in the subgroup of patients with less advanced disease (75% for PB and 72% for BM), those patients with more advanced disease demonstrated a significantly enhanced overall survival when mobilized allogeneic PBSCs were used as a source of stem cells (57% for PB and 33% for BM; P = .04). With a median follow-up for all surviving patients of 26 months (9–47 months), the cumulative incidence of grade III–IV acute GVHD at 100 days was 64% in the PB group and 57% in the BM group (P = .35). The cumulative incidence of grade II–IV acute GVHD was 15% in the PB group and 12% in the BM group (P = NS). Although the follow-up was relatively short, the cumulative incidence of extensive cGVHD was 46% in the PB group and 35% in the BM group (P = .54). These results were inconsistent with many of the other smaller Phase 2 and Phase 3 studies, which all showed no difference in rates of acute GVHD and increased rates of cGVHD in recipients of allogeneic PBSC.
A recent meta-analysis was performed by Cutler et al39 summarizing 15 Phase 2 and Phase 3 trials assessing the risk of GVHD in recipients of allogeneic PBSC and BM. This analysis demonstrated a modest increased relative risk of acute GVHD (relative risk 1.2) and a significant increased risk of developing cGVHD (relative risk 1.8) in recipients of allogeneic PBSCs. It also demonstrated a modest reduction in relative risk of relapse in recipients of allogeneic PBSCs compared to BM (relative risk 0.8).
Champlin et al and the IBMTR40 performed a retrospective case controlled study comparing the outcomes of recipients of allogeneic PBSCs and BM. Median follow-up was 1 year, and this study focused on 1-year outcomes. A total of 288 HLA-identical sibling PBSC recipients was compared with 536 case control allogeneic BM recipients. All patients received T-replete stem cell products. There was no significant difference in the incidence of grades II–IV acute GVHD (40% for PB and 35% for BM; P = NS) or grades III–IV acute GVHD (13% for PB and 19% for BM; P = NS). There was less variability in recovery times of both platelets and neutrophils after allogeneic PBSC compared to BM and statistically faster neutrophil and platelet recovery after allogeneic PBSC compared to allogeneic BM. Treatment-related mortality (TRM), disease-free survival, and overall survival were similar for patients with acute leukemia in first remission. In contrast, acute leukemia patients in second remission and patients with CML in accelerated phase experienced lower TRM, improved DFS and overall survival when allogeneic PBSCs were used as a source of stem cells. There was no apparent difference in the risk of relapse after allogeneic PBSC versus BM transplantation. There was a trend toward lower relapse rates in patients with high-risk leukemia (acute leukemia in second remission and CML in accelerated phase). The relative risk of both limited and extensive cGVHD was increased in recipients of allogeneic PBSCs (relative risk 1.3).
Mohty et al41 have performed the only long-term follow-up of allogeneic PBSC and BM recipients focusing specifically on the rates of cGVHD. At a median follow-up of 45 months (range 31–57 months), the 3-year cumulative incidence of cGVHD was 65% in the PBSC group (n = 53) and 36% in the BM group (n = 48) (P = .004). Extensive chronic GVHD was also more frequent in the PBSC group (44% versus 17%; P = .004).
These data suggest that although hematopoietic recovery is increased in recipients of allogeneic PBSC, there appears to be no increased risk of acute GVHD and a modest increase risk of cGVHD including extensive cGVHD. Overall survival in recipients of allogeneic PBSCs may be improved modestly but only in those patients with more advanced hematologic malignancies. Although no study has correlated rates of either acute or chronic GVHD with the number of CD3 cells/kg in the stem cell products, several studies have suggested that CD34 cells in excess of 8 × 106/kg found in allogeneic PBSC products are associated with a greater risk of both acute GVHD and GVHD.
Impact of G-CSF Mobilization on Graft Content and Immune Reconstitution
Very little data exist on the relative impact of allogeneic PBSCs versus BM on immunologic reconstitution after allogeneic stem cell transplantation. Storek et al42 analyzed the incidence of documented and suspected infections after transplantation of mobilized allogeneic PBSCs and BM in the randomized trial carried out by Bensinger et al.38 The cumulative incidence of infections was higher in the allogeneic BM group (120 versus 90 at 1 year). Since rates of acute GVHD after allogeneic PBSC infusions are similar to BM in spite of these products having 10- to 50-fold increased CD3 cells/kg over allogeneic BM products, a number of investigators have tried to understand the reason for this. To date, no studies have clearly shown a difference in either B-cell or T-cell recovery after allogeneic PBSC transplantation compared to BM transplantation.
A number of reports have emphasized the role of cytokines as mediators of GVHD. Cytokines produced by both CD4 and CD8 T cells can be segregated into two patterns: type I cytokines such as interferon-γ and IL-2 and type 2 cytokines, such as IL-4 and IL-10. Type 1 cytokines are proinflammatory and type 2 cytokines are considered anti-inflammatory. Multiple studies have shown that T cells that elaborate type 1 cytokines (Th1 cells) mediate GVHD whereas those T cells that elaborate type 2 cytokines (Th2 cells) inhibit GVHD. Pan et al43 demonstrated that splenocytes from mice mobilized with G-CSF were polarized toward the Th2 phenotype. Those mice who received splenocytes from G-CSF-mobilized donor mice demonstrated significantly longer survival and less GVHD that those allogeneic transplant recipient mice who were infused with splenocytes from naïve unmobilized donor mice. T cells from G-CSF treated mice showed a significant increase in IL-4 production with a simultaneous decrease in IL-2 and interferon-γ production. This polarization persisted in secondary mixed lymphocyte reactions (MLR) despite the absence of G-CSF during in vitro MLR.
Arpinati et al hypothesized that G-CSF-mobilized PBSC contained antigen-presenting cells which prime T cells to produce Th2 cytokines.44 Two distinct lineages of dendritic cells (DC) have been described in humans. DC1 cells or myeloid DCs express HLA-DR, CD11c, CD13, and CD33 and require GM-CSF for their survival. These cells are negative for both myeloid and lymphoid specific markers (Lin−), produce high levels of IL-12 when stimulated with tumor necrosis factor (TNF) or CD40 ligand and drive the differentiation of naïve T cells into the Th1 phenotype. DC2 or lymphoid DC are HLA-DR+/CD11c−/CD4+/IL-3Ra+ express high levels of T-cell receptor α chain and depend on IL-3, and not GM-CSF, for their survival and differentiation. After appropriate activation, they can induce T-cell differentiation into Th2 cells. These investigators studied the effects of G-CSF mobilization (10–16 μg/kg/day for 5 days) on DC content in the peripheral blood in these allogeneic donors. G-CSF treatment was found to mobilize DC2 but not DC1. Although the numbers of donors and controls studied were very small, the median number of DC1 per liter in the G-CSF group was not different (11 versus 10 × 106/liter; P = .52) than in the control premobilization group. In contrast, the numbers of DC2 were significantly increased in the G-CSF mobilization group compared with control (median 24.8 versus 4.9 × 106/liter; P = .0009). As expected, a proliferative response of naïve allogeneic T cells could be detected in vitro to fresh DC1 but not to fresh DC2. Activation of DC2 in vitro with TNF, GM-CSF, and IL-3 resulted in the rapid maturation of these precursors to mature DC2 cells overexpressing costimulatory molecules such as CD80 and CD86 restoring their ability to induce a proliferative response to naïve CD4+/CD45RA allogeneic T cells. Incubation of naïve allogeneic T cells with DC1 resulted in polarization of these T cells toward the Th1 phenotype as measured by restimulation of these T cells with PMA and ionomycin and detecting primarily IL-2 and interferon-γ as the major intracellular cytokines produced after restimulation. In contrast, incubation of naïve T cells with DC2 cells results in the polarization of these T cells toward the Th2 phenotype as noted by the intracellular accumulation of IL-4 and IL-10 after restimulation in vitro with PMA and ionomycin. In conclusion, G-CSF mobilization results in stem cell products with 10- to 50-fold more T cells and 4- to 6-fold more DC2 cells. The increased numbers of DC2 in G-mobilized products may reduce the relative risk of acute GVHD as seen in preclinical murine allogeneic transplant studies described above and observed in the initial Phase 2 and 3 clinical trials in humans comparing BM versus mobilized PBSCs as sources of allogeneic stem cells. It is of interest that cord blood stem cell products, which are associated with a low risk of severe acute GVHD, contain primarily DC2 and negligible DC1.45 Consistent with this notion, Waller found a strong inverse correlation with the number of precursor DC2 infused in allogeneic bone marrow and the incidence of both cGVHD and, more importantly, relapse.46
Alternative Allogeneic PBSC Mobilization Regimens
Although other cytokines, in addition to G-CSF, have been used to mobilized autologous PBSCs from humans including GM-CSF, Flt-3 ligand, stem cell factor (SCF), Daniplestim (IL-3 agonist), thrombopoietin agonists, chimeric cytokines including Leridistim (IL-3 agonist-G-CSF chimeric molecule) and Progenipoietin-1 (Flt-3 ligand-G-CSF chimeric molecule), peg-filgrastim (Neulasta™) and SDF-1 antagonist (AMD 3100), only G-CSF and GM-CSF have been approved by the FDA and only G-CSF has been studied extensively for the mobilization of allogeneic PBSCs in humans.
We have performed several sequential nonrandomized trials to determine the comparative effects of allogeneic PBSCs mobilized with G-CSF at 10 μg/kg/day (n = 96), G-CSF (10 μg/kg/day) combined with GM-CSF at 5 μg/kg/day (n = 102) or GM-CSF alone (10 or 15 μg/kg/day (n = 32). A comparison of the various allogeneic PBSC mobilization regimens is shown in Table 2 . All donors underwent leukapheresis (20 liter) on the fifth day of cytokine administration. The target CD34+ content was 5.0 × 106 CD34/kg with a minimum of 2 × 106/kg. The data shown in Table 2 are expressed as mean +/− SD. PBSCs mobilized with G/GM resulted in collection of grafts with similar CD34 content compared with G alone. Grafts obtained following mobilization with GM alone contained significantly fewer CD34+ cells, but sufficient numbers for rapid engraftment. Grafts mobilized with GM or G/GM contained significantly fewer T and NK cells. There were no obvious differences in donor toxicities including bone pain. All recipients of GM mobilized cells engrafted with kinetics similar to recipients of G and G/GM, although neutrophil recovery was delayed about 1 day. Rates of neutrophil and platelet recovery and cGVHD for the G and GM groups are shown in Table 3 . In 30 evaluable recipients of peripheral blood grafts mobilized with GM alone, the actuarial risk of grades 2–4 acute GVHD was only 0.13 ± 0.05 and 0.00 (0/31) for grades 3–4 acute GVHD. In a multivariate analysis including patient and donor age, sex mismatching, conditioning regimen received, CD3+ cell dose and CD34+ cell dose, only the receipt of PBSCs mobilized with GM-CSF alone correlated with a lower risk of grades 2–4 acute GVHD. These data suggest that altering the mobilization regimen and cytokines used may alter the functional aspects of the graft thereby modifying outcomes such as GVHD. Randomized Phase 3 studies will need to be performed to more accurately dissect the phenotypic differences in grafts mobilized by different cytokines/chemokines or combinations and to more accurately assess the impact on important endpoints such as multilineage engraftment, disease-free survival, overall survival, GVHD, and relapse.
Chemokines such as IL-8 have been used to induce the egress of hematopoietic stem cells into the peripheral blood of mice and nonhuman primates. This effect is rapid (30 minutes-4 hours) and may result from the ability of these chemokines to induce the release of a protease from mature myeloid cells resulting in a decrease in the intramedullary concentration of SDF-1, the ligand for the receptor CXCR4, which is expressed in many cells including hematopoietic stem cells.47,48 Increasing evidence points to the critical role of the CXCR4/SDF-1 axis in both murine and human stem cell mobilization. The bicyclam molecular AMD 3100 was first clinically developed for its potent and selective inhibition of HIV type 1 and 2 replication through binding to the chemokine receptor, CXCR4. Initial clinical trials in AIDS patients demonstrated that AMD-3100 induced a rapid (within 1 hour) increase in both WBC and circulating progenitor cells. Broxmeyer and colleagues demonstrated a 40-fold increase in the mobilization of hematopoietic progenitors within 1 hour of AMD-3100 injection in mice.49,50 Studies in human volunteers and the first Phase 1 and 2 clinical trials in patients undergoing autologous stem cell transplantation are currently underway.51 These studies have shown a consistent and rapid impact on stem cell mobilization when given alone and a synergistic effect on CD34+ mobilization when coadministered with G-CSF. Since CXCR4 is expressed on different types of cells including CD34+ progenitor and T cells, the impact of AMD-3100 on both multilineage engraftment and GVHD will need to be appropriately explored in preclinical animal models before it can be safely used as a rapid mobilizing agent for allogeneic PBSC transplantation in humans.
Randomized trials comparing allogeneic peripheral blood to bone marrow.
| . | . | ANCa . | PLTb . | TRM . | aGVHD . | cGVHD . | Overall Survival . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study . | n . | PB . | BM . | PB . | BM . | PB, % . | BM, % . | PB, % . | BM, % . | PB, % . | BM, % . | PB, % . | BM, % . |
| a Engraftment (days) ANC > 500/mm3 | |||||||||||||
| b Engraftment (days) Plt > 25000/mm3 | |||||||||||||
| Abbreviations: ANC, absolute neutrophil count; PLT, platelets; TRM, treatment-related mortality; aGVHD, acute graft-versus-host disease; cGVHD, chronic GVHD; PB, peripheral blood; BM, bone marrow. | |||||||||||||
| Vigorito32 | 37 | 16 | 18 | 12 | 17 | 78 | 63 | 27 | 19 | 100 | 50 | 47 | 51 |
| Blaise33 | 101 | 15 | 21 | 13 | 21 | 23 | 21 | 44 | 42 | 50 | 28 | 61 | 61 |
| Powles34 | 39 | 17.5 | 23 | 11 | 18 | 31 | 35 | 68 | 58 | 44 | 40 | 70 | 68 |
| Heldal35 | 61 | 17 | 23 | 13 | 21 | 17 | 10 | 21 | 10 | 56 | 27 | 80 | 73 |
| Schmitz36 | 350 | 12 | 15 | 15 | 20 | ND | ND | 52 | 39 | 74 | 53 | ND | ND |
| Couban37 | 228 | 19 | 22 | 16 | 22 | 7.5 | 16 | 40 | 40 | 71 | 55 | 68 | 55 |
| Bensinger38 | 172 | 16 | 21 | 13 | 19 | 21 | 30 | 64 | 57 | 46 | 35 | 66 | 54 |
| . | . | ANCa . | PLTb . | TRM . | aGVHD . | cGVHD . | Overall Survival . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study . | n . | PB . | BM . | PB . | BM . | PB, % . | BM, % . | PB, % . | BM, % . | PB, % . | BM, % . | PB, % . | BM, % . |
| a Engraftment (days) ANC > 500/mm3 | |||||||||||||
| b Engraftment (days) Plt > 25000/mm3 | |||||||||||||
| Abbreviations: ANC, absolute neutrophil count; PLT, platelets; TRM, treatment-related mortality; aGVHD, acute graft-versus-host disease; cGVHD, chronic GVHD; PB, peripheral blood; BM, bone marrow. | |||||||||||||
| Vigorito32 | 37 | 16 | 18 | 12 | 17 | 78 | 63 | 27 | 19 | 100 | 50 | 47 | 51 |
| Blaise33 | 101 | 15 | 21 | 13 | 21 | 23 | 21 | 44 | 42 | 50 | 28 | 61 | 61 |
| Powles34 | 39 | 17.5 | 23 | 11 | 18 | 31 | 35 | 68 | 58 | 44 | 40 | 70 | 68 |
| Heldal35 | 61 | 17 | 23 | 13 | 21 | 17 | 10 | 21 | 10 | 56 | 27 | 80 | 73 |
| Schmitz36 | 350 | 12 | 15 | 15 | 20 | ND | ND | 52 | 39 | 74 | 53 | ND | ND |
| Couban37 | 228 | 19 | 22 | 16 | 22 | 7.5 | 16 | 40 | 40 | 71 | 55 | 68 | 55 |
| Bensinger38 | 172 | 16 | 21 | 13 | 19 | 21 | 30 | 64 | 57 | 46 | 35 | 66 | 54 |
Comparison of G versus G/GM versus GM mobilization on allograft content.
| Parameter . | G Alone . | G/GM . | GM Alone . | P value . |
|---|---|---|---|---|
| # donors | 96 | 102 | 32 | |
| Total # LP procedures required | 1.26 ± 0.5 | 1.20 ± 0.5 | 1.6 ± 0.7 | G vs G/GM: .5; G vs GM: .002 |
| CD34 (× 106/kg) | 9.8 ± 7.2 | 10.9 ± 7.9 | 3.7 ± 2.0 | G vs G/GM: .28; G vs GM: < .001 |
| CD3 (× 108/kg) | 3.5 ± 2.4 | 1.8 ± 1.5 | 1.8 ± 1.8 | G vs G/GM: < .0001; G vs GM: < .001 |
| CD4 (× 108/kg) | 2.3 ± 1.4 | 1.3 ± 1.0 | 0.9 ± 0.8 | G vs G/GM: < .0001; G vs GM: < .001 |
| CD8 (× 108/kg) | 1.1 ± 0.7 | 0.4 ± 0.4 | 0.3 ± 0.26 | G vs G/GM: .56; G vs GM: .002 |
| CD19 (× 108/kg) | 0.97 ± 0.9 | 0.89 ± 0.63 | 0.45 ± 0.4 | G vs G/GM: .56; G vs GM: .002 |
| CD16/56 (× 107/kg) | 4.63 ± 3.7 | 2.98 ± 2.36 | 1.66 ± 1.18 | G vs G/GM: < .001; G vs GM: < .0001 |
| Parameter . | G Alone . | G/GM . | GM Alone . | P value . |
|---|---|---|---|---|
| # donors | 96 | 102 | 32 | |
| Total # LP procedures required | 1.26 ± 0.5 | 1.20 ± 0.5 | 1.6 ± 0.7 | G vs G/GM: .5; G vs GM: .002 |
| CD34 (× 106/kg) | 9.8 ± 7.2 | 10.9 ± 7.9 | 3.7 ± 2.0 | G vs G/GM: .28; G vs GM: < .001 |
| CD3 (× 108/kg) | 3.5 ± 2.4 | 1.8 ± 1.5 | 1.8 ± 1.8 | G vs G/GM: < .0001; G vs GM: < .001 |
| CD4 (× 108/kg) | 2.3 ± 1.4 | 1.3 ± 1.0 | 0.9 ± 0.8 | G vs G/GM: < .0001; G vs GM: < .001 |
| CD8 (× 108/kg) | 1.1 ± 0.7 | 0.4 ± 0.4 | 0.3 ± 0.26 | G vs G/GM: .56; G vs GM: .002 |
| CD19 (× 108/kg) | 0.97 ± 0.9 | 0.89 ± 0.63 | 0.45 ± 0.4 | G vs G/GM: .56; G vs GM: .002 |
| CD16/56 (× 107/kg) | 4.63 ± 3.7 | 2.98 ± 2.36 | 1.66 ± 1.18 | G vs G/GM: < .001; G vs GM: < .0001 |
Effect of cytokine mobilization regimen on graft-versus-host disease (GVHD)/survival.
| . | G-CSF, % n = 40 . | G-CSF and GM-CSF, % n = 66 . | GM-CSF, % n = 30 . | P Value . |
|---|---|---|---|---|
| Abbreviations: G-CSF, granulocyte colony-stimulating factor; GM-CSF, granulocyte-macrophage colony-stimulating factor; NS, not significant | ||||
| Acute grade 2–4 | 51 | 65 | 13 | G vs GM: .003 |
| GM vs G/GM: < .0001 | ||||
| G vs G/GM: .11 | ||||
| Acute grade 3–4 | 11 | 13 | 0 | .07 |
| Chronic GVHD | 86 | 88 | 65 | NS |
| Survival (2 years) | 62 | 56 | 59 | NS |
| * High 38 | High 28 | High 35 | ||
| * Low 88 | Low 75 | Low 69 | ||
| . | G-CSF, % n = 40 . | G-CSF and GM-CSF, % n = 66 . | GM-CSF, % n = 30 . | P Value . |
|---|---|---|---|---|
| Abbreviations: G-CSF, granulocyte colony-stimulating factor; GM-CSF, granulocyte-macrophage colony-stimulating factor; NS, not significant | ||||
| Acute grade 2–4 | 51 | 65 | 13 | G vs GM: .003 |
| GM vs G/GM: < .0001 | ||||
| G vs G/GM: .11 | ||||
| Acute grade 3–4 | 11 | 13 | 0 | .07 |
| Chronic GVHD | 86 | 88 | 65 | NS |
| Survival (2 years) | 62 | 56 | 59 | NS |
| * High 38 | High 28 | High 35 | ||
| * Low 88 | Low 75 | Low 69 | ||
Predictive formula that allows the clinician to know when to start apheresis in order to optimize collection and how many liters of blood need to be processed in order to collect a given number of CD34+cells.
Predictive formula that allows the clinician to know when to start apheresis in order to optimize collection and how many liters of blood need to be processed in order to collect a given number of CD34+cells.