Abstract
Clinical hematologists are frequently consulted for the care of hospitalized patients with complicated coagulopathies. This chapter provides an update on the scientific and clinical advances noted in disseminated intravascular coagulation (DIC) and discusses the challenges in hemostasis consultation.
In Section I, Dr. Marcel Levi reviews advances in our understanding of the pathogenic mechanisms of DIC. Novel therapeutic strategies that have been developed and evaluated in patients with DIC are discussed, as are the clinical trials performed in patients with sepsis.
In Section II, Dr. Lawrence Leung provides an overview of the challenging problems in thrombosis encountered in the inpatient setting. Patients with deep vein thrombosis that is refractory to conventional anticoagulation and those with extensive mesenteric thrombosis as well as the evaluation of a positive PF4/heparin ELISA in a post-operative setting are discussed. Novel treatments for recurrent catheter thrombosis in dialysis patients is addressed as well.
In Section III, Dr. Julie Hambleton reviews the hemostatic complications of solid organ transplantation. Coagulopathy associated with liver transplantation, contribution of underlying thrombophilia to graft thrombosis, drug-induced microangiopathy, and the indication for postoperative prophylaxis are emphasized. Dr. Hambleton reviews the clinical trials evaluating hemostatic agents in patients undergoing liver transplantation.
I. Disseminated Intravascular Coagulation: New Concepts, New Controversies
Marcel Levi, MD*
Dept. Internal Medicine (F-4), Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands
A variety of disorders may lead to a systemic activation of coagulation. This may be mild and clinically insignificant, but in more severe forms it can dominate the clinical picture, such as in its most extreme manifestation as disseminated intravascular coagulation (DIC).1,2 DIC is characterized by a widespread and ongoing activation of coagulation, leading to possible vascular or microvascular fibrin deposition and thereby compromising an adequate blood supply to various organs, which may contribute to organ failure. Ongoing activation of the coagulation system, impaired synthesis, and increased degradation of coagulation factors frequently results in decreased levels of procoagulant proteins, protease inhibitors, and platelets. This situation may result in serious bleeding, in particular in patients who are at risk for major blood loss, such as perioperative patients or trauma patients. Hence, a clinical situation with simultaneously occurring thrombosis and bleeding may occur, which may pose a difficult problem for the clinician.
A rough search in the PubMed database from 1966 to 2002 using the search term “disseminated intravascular coagulation” and related keywords yielded 14,217 publications, for the most part case reports and papers related to the pathophysiology of DIC, which is indeed in its main features well understood now. Nevertheless, in the absence of sound clinical trials, an evidence-based approach to the appropriate diagnosis and treatment of patients with DIC remained difficult until recently. Interestingly, in the past 3-5 years a rapidly increasing proportion of the articles on DIC, including a number of articles reporting on randomized controlled trials, have addressed the diagnosis and management of DIC.
Disorders Associated with DIC and Clinical Relevance
It is important to emphasize that DIC is not a disease in itself but is always secondary to an underlying disorder. The underlying disorders most commonly known to be associated with DIC are listed in Table 1 .
Bacterial infection, in particular septicemia, is commonly associated with DIC.3,4 However, systemic infections with other microorganisms, such as viruses and parasites, may lead to DIC as well. Factors involved in the development of DIC in patients with infections may be specific cell membrane components of the microorganism (lipopolysaccharide or endotoxin) or bacterial exotoxins (e.g. staphylococcal alpha toxin). These components may cause a generalized inflammatory response, characterized by elevated levels of cytokines. Cytokines are mainly produced by activated mononuclear cells and endothelial cells and are partially responsible for the derangement of the coagulation system in DIC.5
Severe trauma is another clinical condition frequently associated with DIC.6 A combination of mechanisms—including release of tissue material (fat, phospholipids) into the circulation, hemolysis, and endothelial damage—may contribute to the systemic activation of coagulation. In addition, there is emerging evidence that cytokines play a pivotal role in the occurrence of DIC in trauma patients as well. In fact, systemic cytokine patterns have been shown to be virtually identical in trauma patients and septic patients.7
Both solid tumors and hematological malignancies may be complicated by DIC.8,9 The mechanism of the derangement of the coagulation system in this situation is poorly understood. Solid tumor cells can express procoagulant molecules, including tissue factor and a cancer procoagulant, a cysteine protease with factor X activating properties. Cancer procoagulant is found in extracts of neoplastic cells and in the plasma of patients with solid tumors.10 A distinct form of DIC is frequently encountered in acute promyelocytic leukemia, which is characterized by a severe hyperfibrinolytic state in addition to an activated coagulation system.11 Although clinically bleeding predominates in this situation, disseminated thrombosis is found in a considerable number of patients at autopsy.
Acute DIC occurs in obstetrical complications such as placental abruption and amniotic fluid emboli.12 Amniotic fluid has been shown to be able to activate coagulation in vitro, and the degree of placental separation correlates with the extent of DIC, suggesting that leakage of thromboplastin-like material from the placental system is responsible for DIC. Although the coagulation system may be activated in patients with preeclampsia and HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome, it is subclinical, and overt DIC only occurs in a small percentage of patients, usually in patients with an abruptio placentae or some other complication.
Vascular disorders, such as large aortic aneurysms or giant hemangiomas (Kasabach-Merritt syndrome), may result in local activation of coagulation.13 Activated coagulation factors can ultimately “overflow” to the systemic circulation and cause DIC, but more common is the systemic depletion of coagulation factors and platelets as a result of local consumption.
Microangiopathic hemolytic anemia represents a group of disorders comprising thrombocytopenic thrombotic purpura (TTP), hemolytic uremic syndrome, chemotherapy-induced microangiopathic hemolytic anemia, malignant hypertension, and the HELLP syndrome.14 Although some characteristics of microangiopathic hemolytic anemia and the resulting thrombotic occlusion of small and midsize vessels leading to organ failure may mimic the clinical picture of DIC, these disorders in fact represent a distinct group of diseases.
The clinical problem of DIC with severe thrombocytopenia and low levels of coagulation factors in patients with severe bleeding is indisputable. However, major bleeding occurs in only a minority of patients with DIC. Much more common is the occurrence of organ failure, but there is considerable debate about the extent to which vascular and microvascular fibrin deposition, as a consequence of DIC, contributes to this. However, there are several lines of evidence indicating that DIC has an important pathogenetic role in the development of organ failure. First, extensive data have been reported on postmortem findings of patients with DIC.15 These autopsy findings include diffuse bleeding at various sites, hemorrhagic necrosis of tissue, microthrombi in small blood vessels, and thrombi in midsize and larger arteries and veins. The demonstration of ischemia and necrosis was invariably due to decreased blood flow and fibrin deposition in small and midsize vessels of various organs. Importantly, the presence of these intravascular thrombi appears to be clearly and specifically related to the clinical dysfunction of the organ. Second, experimental animal studies of DIC show fibrin deposition in various organs. Experimental bacteremia or endotoxemia causes intra- and extravascular fibrin deposition in the kidneys, the lungs, the liver, the brain, and various other organs. Amelioration of the hemostatic defect by various interventions in these experimental models appears to improve organ failure and, in some but not all cases, to reduce mortality.16,17 Lastly, clinical studies support the concept of coagulation as an important denominator of clinical outcome. DIC has been shown to be an independent predictor of mortality in patients with sepsis and severe trauma.1,18
Pathogenesis
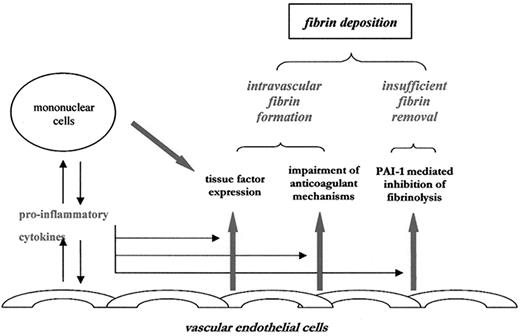
In recent years the mechanisms involved in pathological microvascular fibrin deposition in DIC have become increasingly clear. As outlined below, initiation of coagulation is tissue factor dependent; amplification of thrombin generation is due to defective physiological anticoagulant mechanisms; and propagation of fibrin deposition in the microvasculature is caused by insufficient fibrin degradation as a result of an inhibited fibrinolytic system (Figure 1 ).
Initiation of fibrin deposition: Predominance of tissue factor–dependent coagulation
Traditionally, DIC was thought to be the result of activation of both the extrinsic and the intrinsic (contact system–mediated) coagulation pathway. In the last 15 years it has become apparent that thrombin generation in DIC is exclusively mediated by the extrinsic (tissue factor/factor VIIa–driven) pathway. Tissue factor may be expressed on activated and inactivated mononuclear cells and endothelial cells and is capable of binding factor VIIa, which then activates downstream coagulation cascades. Several lines of evidence support the notion that tissue factor is the central mediator of coagulation activation in sepsis. First, analysis of molecular markers for activation of various coagulation factors in models of experimental sepsis or endotoxemia has shown that thrombin generation was tissue factor/factor VIIa–dependent, while there was no evidence for activation of other pathways of coagulation.3 Second, inhibition of the tissue factor/factor VIIa pathway in experimental sepsis models showed complete abrogation of thrombin generation and fibrin deposition, whereas blocking alternative pathways did not show any effect.19,20 Lastly, in vivo studies and observations in patients with sepsis have confirmed that endotoxin and proinflammatory cytokines induce tissue factor expression on circulating monocytes.21 While the tissue factor/factor VIIa pathway is crucial for activation of coagulation in DIC, the contact system is activated as well, but this seems not to be relevant for thrombin generation.22 Instead, this system may play a role in regulation and dysregulation of hemodynamics and fibrinolytic activation.22,23
Amplification of fibrin deposition: Defective physiological anticoagulant systems
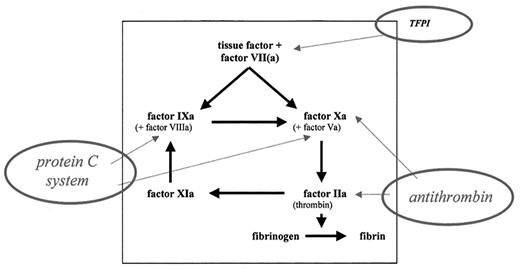
Regulation of thrombin generation normally occurs at three levels in the coagulation system: at the level of thrombin and factor Xa by antithrombin, at the level of the essential cofactors V and VIII by activated protein C, and at the level of the tissue factor/factor VIIa complex by tissue factor pathway inhibitor (TFPI) (Figure 2 ). In DIC, each of these three major physiological anticoagulant mechanisms is defective.
Antithrombin appears to be incapable of adequate regulation of thrombin activity in DIC, for several reasons. First, antithrombin levels are continuously consumed by the ongoing formation of thrombin and other activated proteases that are susceptible to antithrombin complex formation.24 Second, antithrombin is degraded by elastase released from activated neutrophils.25 Third, impaired synthesis of antithrombin because of hepatic dysfunction in sepsis and extravascular leakage of this protease inhibitor as a consequence of capillary leakage further contribute to low levels of antithrombin. Clinical studies show mean levels of antithrombin as low as 30% in patients with severe sepsis.26 Low levels of antithrombin have been shown to be associated with a higher mortality in septic patients in several prospective studies.18 Restoration of antithrombin levels in experimental DIC in animals has been demonstrated to adequately block the systemic activation of coagulation and improved outcome in terms of less organ failure and a reduction in mortality.17,27
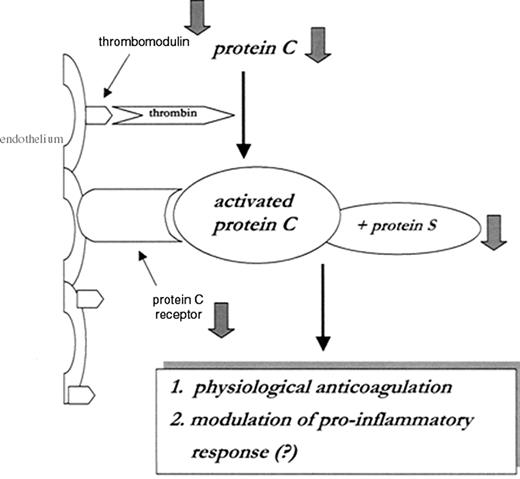
There are several reasons for the inadequacy of the protein C system in sepsis (Figure 3 ). First, enhanced consumption, impaired liver synthesis, and vascular leakage may result in low circulating levels of protein C.24 Second, activation of the cytokine network, in particular high levels of tumor necrosis factor-α (TNF-α), results in a marked downregulation of thrombomodulin on endothelial cells, thereby prohibiting adequate protein C activation.28 The downregulation of thrombomodulin in DIC was shown in skin biopsies from patients with meningococcal septicemia.29 Last, the anticoagulant capacity of activated protein C is reduced by low levels of the free fraction of protein S. In plasma, 60% of the cofactor protein S is complexed to a complement regulatory protein, C4b binding protein (C4bBP). Increased plasma levels of C4bBP, as a consequence of the acute phase reaction in sepsis, may result in a relative protein S deficiency. Although it has been shown that the β-chain of C4bBP (which is important in binding protein S) is not very much affected during the acute phase response,30 the infusion of C4bBP in combination with a sublethal dose of Escherichia coli into baboons resulted in a lethal response with severe organ damage due to DIC.31 Moreover, the important role of the protein C system in the pathogenesis of DIC is underscored by experimental studies showing that administration of activated protein C to these animals resulted in amelioration of DIC and improved survival.32
DIC is in general associated with only modestly reduced levels, or even increased concentrations, of TFPI plasma levels.33 Administration of high doses of (recombinant) TFPI resulted in the complete inhibition of experimental bacteremia- or endotoxin-induced coagulation activation.16,34 Based on these observations, it was hypothesized that the TFPI pathway is relatively insufficient during DIC.
Propagation of fibrin deposition: Inhibition of fibrinolysis
Experimental models indicate that at the time of maximal activation of coagulation, the fibrinolytic system is largely downregulated. Experimental bacteremia and endotoxemia result in a rapidly occurring increase in fibrinolytic activity, most probably due to the release of plasminogen activators from endothelial cells. This profibrinolytic response is almost immediately followed by a suppression of fibrinolytic activity because of a sustained increase in plasma levels of plasminogen activator inhibitor, type 1 (PAI-1).35,36 The dominant role of PAI-1 in the depression of fibrinolysis in DIC was illustrated by the lack of thrombi in the kidneys of PAI-1 knockout mice challenged with endotoxin.37 Recent studies have shown that a functional mutation in the PAI-1 gene, the 4G/5G polymorphism, not only influenced the plasma levels of PAI-1 but also was linked to clinical outcome of meningococcal septicemia. Patients with the 4G/4G genotype had significantly higher PAI-1 concentrations in plasma and an increased risk of death.38 In other clinical studies in patients with DIC, high plasma level of PAI-1 was one of the strongest predictors of mortality.3
Diagnosis of DIC
It is important to realize that no single laboratory test available today is sensitive enough or specific enough to allow a definite diagnosis of DIC. According to the current understanding of the disease, the determination of soluble fibrin in plasma appears to be crucial for the diagnosis of DIC. Most of the clinical studies show a sensitivity of 90-100% of increased soluble fibrin plasma levels in DIC but a very low specificity.39 Another problem is that a reliable test is not available for quantifying soluble fibrin in plasma. A recent study showed a wide discordance among various assays for soluble fibrin.40 Fibrin degradation products (such as FDPs) may be detected by specific enzyme-linked immunosorbent assays (ELISAs) or by latex agglutination assays, allowing rapid and bedside determination in emergency cases. However, some of the available assays for FDPs cross react with fibrinogen degradation products, which may cause spuriously high results.41 The specificity of high levels of FDPs is limited because many other conditions, such as inflammation or recent surgery, are associated with elevated FDPs. More recently, developed tests are specifically aimed at the detection of neoantigens on degraded cross-linked fibrin, such as D-dimer. D-dimer levels are elevated in patients with DIC but also poorly distinguish patients with DIC from patients with trauma or recent surgery.42 The dynamics of DIC can also be judged by measuring activation markers that are released upon the conversion of a coagulation factor zymogen to an active protease, such as prothrombin activation fragment F1+2.43 Indeed, these markers are markedly elevated in patients with DIC.
Most of the sensitive and sophisticated tests described above are not available to general hospital laboratories. Although these tests may be very helpful in clinical trials or other research, they can often not be used in a routine setting. However, in clinical practice a diagnosis of DIC can often be made by a combination of platelet count, measurement of global clotting times (aPTT and PT), measurement of 1 or 2 clotting factors and inhibitors (such as antithrombin), and a test for FDPs. It should be emphasized that serial coagulation tests are usually more helpful than single laboratory results in establishing the diagnosis of DIC. A reduction in the platelet count or a clear downward trend at subsequent measurements is a sensitive (though not specific) sign of DIC.44 The prolongation of global clotting times may reflect the consumption and depletion of various coagulation factors, which may be further substantiated by the measurement of selected coagulation factors, such as factor V and VII. Measurement of coagulation factors may also be helpful to detect additional hemostatic abnormalities (for example, those caused by vitamin K deficiency). Measurement of fibrinogen has been widely advocated as a useful tool for the diagnosis of DIC but in fact is not very helpful. Fibrinogen is an acute-phase reactant and is, for example, also increased in pregnancy. Despite ongoing consumption, plasma levels can remain well within the normal range. In a consecutive series of patients, the sensitivity of a low fibrinogen level for the diagnosis of DIC was only 28%, and hypofibrinogenemia was detected in very severe cases of DIC only.3 Tests for fibrin degradation products (such as FDPs or D-dimer) may be helpful in differentiating other conditions that may be associated with a low platelet count and prolonged clotting times, such as chronic liver disease. However, as noted above, most of these tests are not very specific, and high levels may be encountered in various clinical conditions.
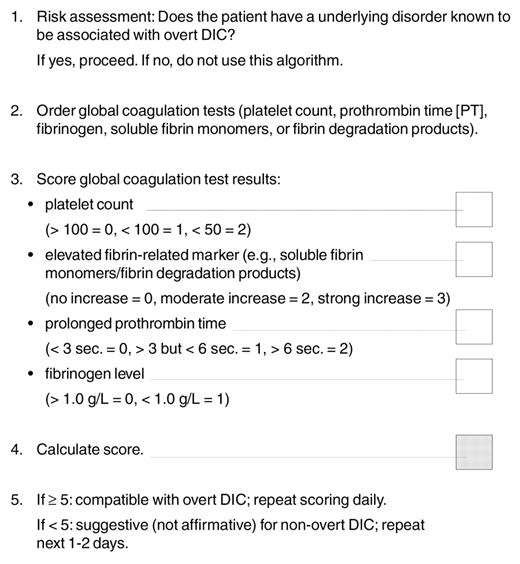
A scoring system that uses simple laboratory tests has recently been published by the subcommittee on DIC of the International Society on Thrombosis and Haemostasis (Table 2 ).45 The presence of an underlying disorder known to be associated with DIC, as listed in Table 2, is a conditio sine qua non for the use of the algorithm. Tentatively, a score of ≥ 5 is compatible with DIC, but a scoring system has not yet been validated by prospective studies.
Management of DIC
The fundament of DIC treatment is the specific and vigorous treatment of the underlying disorder. In some cases, the DIC will completely resolve within hours after resolution of the underlying condition (for example, in cases of DIC induced by abruptio placentae). However, in other cases, such as in patients with sepsis and a systemic inflammatory response syndrome, DIC may continue, even after appropriate treatment. In those cases, supportive measures to manage the DIC may be required and affect morbidity and mortality. The increase in the insight into pathogenetic mechanisms that play a role in DIC has indeed been helpful in developing new supportive management strategies, as outlined below.
Plasma and platelet substitution therapy
Low levels of platelets and coagulation factors may increase the risk of bleeding. However, plasma or platelet substitution therapy should not be instituted on the basis of laboratory results alone; it is indicated only in patients with active bleeding and in those requiring an invasive procedure or otherwise at risk for bleeding complications.46 The suggestion that administration of blood components might “add fuel to the fire” has in fact never been proven in clinical or experimental studies. The efficacy of treatment with plasma, fibrinogen, cryoprecipitate, or platelets is not based on randomized controlled trials but appears to be rational therapy in bleeding patients or in patients at risk for bleeding with a significant depletion of these hemostatic factors. It may be necessary to use large volumes of plasma to correct the coagulation defect.
Anticoagulants
Experimental studies have shown that heparin can at least partly inhibit the activation of coagulation in sepsis and other causes of DIC.47 Uncontrolled case series in patients with DIC have claimed to be successful. However, a beneficial effect of heparin on clinically important outcome events in patients with DIC has never been demonstrated in controlled clinical trials.48 Also, the safety of heparin treatment is debatable in DIC patients who are prone to bleeding. Therapeutic doses of heparin are indicated in patients with clinically overt thromboembolism or extensive fibrin deposition, like purpura fulminans or acral ischemia. Patients with DIC may benefit from prophylaxis to prevent venous thromboembolism, which may not be achieved with standard low-dose subcutaneous heparin.49 Theoretically, the most logical anticoagulant agent to use in DIC is directed against tissue factor activity. Potential agents include recombinant tissue factor pathway inhibitor, inactivated factor VIIa, and recombinant NAPc2, a potent and specific inhibitor of the ternary complex between tissue factor/factor VIIa and the factor derived from the family of nematode anticoagulant proteins (NAPs). At present, all these agents are being investigated in Phase II/III clinical studies.
Restoration of anticoagulant pathways
Since antithrombin is one of the most important physiological inhibitors of coagulation and based on successful preclinical results, the use of antithrombin III concentrates in patients with DIC has been studied relatively intensively. Most of the randomized controlled trials concern patients with sepsis, septic shock, or both. All trials show some beneficial effect in terms of improvement of laboratory parameters, shortening of the duration of DIC, or even improvement in organ function.3 In the more recent clinical trials, very high doses of antithrombin concentrate to attain supraphysiological plasma levels were used. A modest reduction in mortality was seen in antithrombin-treated patients; however, the effect did not reach statistical significance. A large-scale, multicenter, randomized controlled trial to directly address this issue showed no significant reduction in mortality of patients with sepsis who were treated with antithrombin concentrate.50 This trial included 2114 patients with severe sepsis and associated organ failure. Surprisingly, subgroup analyses indicated some benefit in patients who did not receive concomitant heparin, but this observation needs prospective validation.
Based on the notion that depression of the protein C system may significantly contribute to the pathophysiology of DIC, supplementation of activated protein C might be beneficial.24 Recently, a Phase III trial of activated protein C concentrate in patients with sepsis was prematurely stopped because of efficacy in reducing mortality in these patients.51 Mortality, from all causes, at 28 days after inclusion was 24.7% in the activated protein C group versus 30.8% in the control group (19.4% relative risk reduction). The administration of activated protein C ameliorated coagulation abnormalities. In addition, since interaction of activated protein C with the endothelial protein C receptor may also affect proinflammatory factors,52 part of the success may have been caused by a beneficial effect on inflammatory pathways. This hypothesis is supported by the fact that activated protein C seems to be more effective than antithrombin in patients with sepsis. However, minor differences between the trials, such as the use of a coordinating center for inclusion of patients in the activated protein C trial, probably leading to a more homogeneous patient population, may also have contributed to the difference in outcome between the trials. Since infusion of activated protein C is the first intervention shown to be effective in reducing mortality in septic patients, the results of this trial seem to emphasize the importance of the coagulation derangement in the pathogenesis of sepsis and the impact that restoration of microvascular anticoagulant pathways may provide in the treatment of DIC. Recombinant human-activated protein C has been approved by the U.S. Food and Drug Administration and (very recently) by the European Community for treatment of patients with severe sepsis.
Summary
DIC is a syndrome characterized by systemic intravascular activation of coagulation, leading to widespread deposition of fibrin in the circulation. There is good experimental and pathological evidence that the fibrin deposition contributes to multiple organ failure. The massive and ongoing activation of coagulation may result in depletion of platelets and coagulation factors, which may cause bleeding (consumption coagulopathy). DIC is not a disease in itself but is invariably seen as a complication of a variety of disorders, most commonly severe infection or inflammation, trauma, or cancer. A diagnosis of DIC can be made by a combination of routinely available laboratory tests, for which diagnostic algorithms have become available. Recent knowledge on important pathogenetic mechanisms that may lead to DIC has resulted in novel preventive and therapeutic approaches to patients with DIC. Strategies aimed at the inhibition of coagulation activation may theoretically be justified and have been found beneficial in experimental and initial clinical studies. These strategies comprise inhibition of tissue factor–mediated activation of coagulation or restoration of physiological anticoagulant pathways.
II. Challenging Problems in Thrombosis Consultation
Lawrence L. Leung, MD*
Department of Medicine, Stanford University School of Medicine, 269 Campus Drive, CCSR 1155, Stanford, CA 94305-5156
In a tertiary-care hospital setting, consultation requests on inpatient thrombosis cases are generally quite different from those encountered in an outpatient clinic. The latter usually involve patients with a suspected hypercoagulable state who require workup and a decision on the proper duration of anticoagulation. In the inpatient setting, the cases are more acute, requiring prompt evaluation and management decision. Four topics will be covered in this section: refractory deep vein thrombosis (DVT), evaluation of heparin-induced thrombocytopenia (HIT) following cardiovascular surgery, intraabdominal thrombosis, and thrombosis of arteriovenous grafts in hemodialysis patients.
Refractory DVT
A common request is to evaluate a patient with lower-extremity DVT that is deemed refractory to warfarin treatment. In these cases, it is important to document the progression of DVT objectively, usually by repeat ultrasound examination, and compare that to the initial study. In the case of iliofemoral DVT, if the initial diagnosis was based on only an ultrasound study, it is difficult to evaluate whether extension of the clot has occurred, and pelvic magnetic resonance imaging or venography should be considered. Assuming that the patient’s INR has been in the proper therapeutic range of 2–3, one should determine if sufficient overlap with heparin was carried out at the initiation of anticoagulation therapy, especially if the recurrence or extension of DVT occurs within days after switching to coumadin therapy. With the short half-life of factor VII (6 hr), the initial prolongation of prothrombin time and INR within the first 2–3 days of warfarin therapy is mainly due to factor VII depletion. Animal studies have shown that depression of both factor X (half-life ∼40 hr) and particularly prothrombin (half-life ∼60 hr) to approximately 15–25% is required for warfarin’s clinical antithrombotic efficacy.1 Further, since protein C is also vitamin K–dependent and has a short half-life comparable to that of factor VII, an acquired partial protein C deficiency invariably results from the initiation of warfarin therapy. Thus, an overlap of at least 5 days between heparin and warfarin is mandatory for both regular heparin and low–molecular weight heparin (LMWH). Premature cessation of heparin while continuing the patient on warfarin, despite a therapeutic INR, can account for the progression of DVT. In such cases, warfarin therapy has not failed, and additional intervention, such as placement of an inferior vena cava filter, is not indicated.
If the progression of DVT is not due to inadequate overlap between heparin and warfarin, one should check for the presence of antiphospholipid antibodies, such as lupus anticoagulant and anticardiolipin IgG and IgM antibodies. The antiphospholipid antibody syndrome (APS) is a heterogeneous disorder, and it is important that multiple tests utilizing various clotting assays and enzyme-linked immunosorbent assays (ELISAs) for antiphospholipid antibodies be used.2 The antiphospholipid antibodies can fluctuate in antibody titers, and a temporal disappearance of antiphospholipid antibodies during an acute thrombotic episode, perhaps due to their consumption, has also been described.3 Thus, an initial set of negative tests does not conclusively exclude the diagnosis, and one should repeat the tests at a later date, generally within 4-6 weeks. While it remains unclear whether all patients with APS need to be treated with high-intensity warfarin (INR 3–3.5),4 retrospective analysis has shown that some of these patients have increased recurrent thrombotic events while maintained on intermediate-intensity warfarin (INR 2–3).5 APS represents a spectrum of clinical thrombosis with different thrombogenic intensities. Therefore, if APS is documented and the patient has clearly not responded to intermediate-intensity warfarin, using a higher-intensity warfarin therapy or switching the patient to LMWH should be considered.
In this regard, one should also be aware of the so-called “catastrophic antiphospholipid syndrome.”6 This occurs in a small minority of APS patients and is characterized by multiorgan failure, involving the kidneys, lungs, heart, and central nervous system. It appears to involve the small vessels more than the large vessels and occasionally has features of microangiopathy. It can occur abruptly following minor surgical procedures or postpartum. Mortality is high (∼50%) despite aggressive treatment with a combination of therapies, including plasmapheresis, IVIg, high-dose steroids, and cyclophosphamide.
Patients who develop DVT associated with an underlying malignancy (Trousseau’s syndrome) frequently respond poorly to Coumadin, and long-term treatment with LMWH is generally effective.7 The pathophysiology of Trousseau’s syndrome is due to cancer cell-associated expression or release of tissue factor and/or procoagulants leading to chronic DIC. However, laboratory diagnosis of chronic DIC, such as elevation of D-dimer, is not feasible in the setting of acute DVT. The underlying cancer can be occult, and an extensive search is generally not cost-effective and not recommended.8 A thorough clinical evaluation should be performed and a limited search, such as chest X-ray, mammography and pelvic ultrasonography in women, and prostatespecific antigen testing in men, should be considered.9 The underlying cancer generally becomes manifest within one year after the initial diagnosis of DVT.
Evaluation of HIT Following Cardiovascular Surgery
HIT is a serious and life-threatening thrombotic complication of heparin therapy, one that is mediated mainly by the development of antibodies against the heparin/platelet factor 4 (PF4) complex. (A small number of patients have autoantibodies against interleukin-8 or neutrophil-activating pepetide-2, but not heparin-PF4, in HIT.10) Commercially available ELISA kits for the detection of antibodies against the heparin/PF4 complex in patient samples have become popular as a screening test for HIT. These are easy to set up in clinical coagulation laboratories; do not involve the use of radioactive isotope, as required for the platelet serotonin release assay (SRA); and are much less labor intensive than the heparin-induced platelet aggregation (HIPA) studies. The sensitivity and specificity for the heparin/PF4 ELISA assays are generally reported to be in the 85–95% range.11,12
However, the increasing popularity of the heparin/PF4 ELISA kits has posed a problem in the evaluation of thrombocytopenia after cardiac surgery. Mild to moderate thrombocytopenia commonly occurs after cardiopulmonary bypass surgery. In 1996, a high frequency of positive heparin/PF4 ELISA was reported in this group of patients.13 Twenty-two percent of patients were found to be positive preoperatively, following recent cardiac catheterization, and 50% were positive by day 6 post surgery. Both anti-heparin/PF4 IgG and IgM antibodies were found, with titers generally much lower than those associated with confirmed HIT found in other clinical settings. Of importance, the positive heparin/PF4 ELISA in these patients was not associated with the development of more severe thrombocytopenia or clinical thrombosis.
This high prevalence of positive heparin/PF4 ELISA following cardiac surgery and vascular surgery, in which the patients have been exposed to a large dose of heparin, has been confirmed by more recent prospective studies.14– 16 In one study, 5% of patients had a positive SRA and 19% had a positive ELISA before surgery. At day 5 post operatively, 13% of patients were positive by SRA, and 51% positive by ELISA. Of note, 21% of the positive ELISA were also positive by SRA and, conversely, 26% of the SRA positive patients were positive by ELISA. As in the previous study, the development of a positive heparin/PF4 ELISA and/or SRA was not associated with thrombocytopenia or thrombosis. Thus, while the prevalence of a positive heparin/PF4 ELISA is high, its diagnostic specificity is low in these patient populations.
So, when asked to see a patient with a positive ELISA in this setting, what should one do? It should be emphasized that HIT remains a clinical diagnosis. If the patient has a significant drop in platelet count (> 50% compared to the preoperative level) or has any signs of tissue ischemia, one should stop heparin promptly (if it has not already been discontinued) and treat aggressively with one of the alternative anticoagulants (hirudin, argatroban, or danaparoid). However, if the situation is less clear-cut, which is usually the case, there are two options. One is to follow the patient closely, recognizing the high prevalence and low specificity for the positive heparin/PF4 ELISA result in this situation. Another option is to order a functional platelet assay using either SRA or HIPA study. If either of these two functional assays is strongly positive, then one would treat the patient for presumed HIT. With blood samples from patients with suspected HIT, the combined use of heparin/PF4 ELISA in conjunction with SRA or HIPA gives a much better predictive result. If both tests are positive, the predictive value for HIT is excellent12,17 and one may treat the patient for presumed HIT. It is possible that in this particular group of patients, this may still represent overtreatment for some patients.14 However, if there is no major contraindication, the bleeding risk associated with a short course of anticoagulation with hirudin or argatroban should be acceptable. It should be emphasized that this consideration does not apply to non-cardiac surgery patients in whom the prevalence of positive heparin/PF4 ELISA is much lower and a positive ELISA should be taken as highly suggestive of HIT. Once the diagnosis of HIT is made, it is also important to start the anticoagulation with one of the alternative anticoagulants promptly. Heparin cessation alone is generally insufficient to prevent the development of subsequent serious thrombotic events.18,19
Mesenteric Venous Thrombosis
The clinical presentation and management of acute mesenteric ischemia due to arterial and venous thrombosis are quite different (Table 3 ). Acute mesenteric arterial thromboembolism is much more common than mesenteric venous thrombosis. It generally occurs in a more elderly group of patients with underlying atherosclerotic, vascular, and heart disease, presenting with an abrupt-onset abdominal pain.21,22 Acute mesenteric venous thrombosis occurs in younger patients, with a more insidious onset of abdominal pain, usually associated with nausea. Patients have often had symptoms for more than 2 weeks at presentation. An associated hypercoagulable state is reported in a substantial number of these patients;20,21 these include myeloproliferative diseases (polycythemia vera, essential thrombocythemia), protein C deficiency, protein S deficiency, antiphospholipid antibody syndrome, and paroxysmal nocturnal hemoglobinuria.
Acute mesenteric venous thrombosis should be managed with prompt anticoagulation with heparin. In this case, one may choose continuous intravenous regular heparin over LMWH since some of these patients may have concurrent gastrointestinal bleeding and regular heparin allows more rapid dose adjustments. However, unless the bleeding is brisk, anticoagulation should not be withheld.20 Surgical exploration is generally not required, unless there is evidence of peritonitis. The prognosis for patients with acute mesenteric venous thrombosis is better than that for those with acute mesenteric arterial ischemia, although the 30-day mortality is still substantial, reported to be in the range of 13–27% in more recent surgical series.21,23 Recurrence is substantial (36% in a recent series) and commonly occurs within 30 days of the initial event.23
Portal hypertension and varices occur as late sequelae in some patients with mesenteric venous thrombosis, especially when the initial thrombosis involves the portal vein or splenic vein. These patients should be monitored regularly by endoscopy; the benefits of long-term anticoagulation outweigh the risk of recurrent bleeding even in this group of patients.24
Chronic mesenteric venous thrombosis has a presentation distinct from that of acute mesenteric venous thrombosis.20,23 Patients usually have milder symptoms of long duration or are even asymptomatic, with the diagnosis made incidentally on abdominal computed tomography scan done for a different purpose. The presence of extensive collateral blood vessel formation supports the chronicity of the condition. An extensive hypercoagulable workup should be carried out and the patients considered for long-term anticoagulation if there are no contraindications.
Vascular Access Thrombosis in Hemodialysis Patients
Most chronic dialysis patients have an arteriovenous graft as their vascular access; polytetrafluoroethylene (PTFE) dialysis grafts are commonly used. PTFE grafts are prone to recurrent stenosis and thrombosis, which represent a major cause of morbidity, accounting for about 15% of dialysis patient hospitalizations, with an annual cost in the United States of approximately $1 billion.25 In a recent single-institution prospective study, the outcomes of 256 grafts were analyzed over a 2-year period. A salvage procedure (thrombectomy, angioplasty, or surgical revision) was required to maintain graft patency in 77% at 1 year and 96% at 2 years. Permanent graft failure was 35% at 1 year and 49% at 2 years. There is no significant correlation between graft survival and patient age, sex, diabetic status, body mass index, or graft site.26
The pathophysiology related to recurrent access thrombosis is complex. Myointimal hyperplasia is the primary pathophysiological event, leading to stenosis and finally thrombosis at the site of venous anastomosis.27 There is also a growing appreciation that an underlying hypercoagulable state may contribute to this problem. In a recent multicenter study, high-titer anticardiolipin antibodies were found in 19% of end-stage renal disease patients.28 Vascular access thrombosis has been reported to be significantly more common in patients with lupus anticoagulant than in those without lupus anticoagulant.29 In another study, an underlying hypercoagulable state, rather than an anatomical venous stenosis, was found to be the primary determinable cause for thrombosis in approximately 40% of patients.30 Antiphospholipid antibodies predominated, and a moderately high-intensity INR of 2.7–3.0 was effective in reducing the recurrent thrombosis rate in this group of patients.
Recently, intravascular radiation within the restenosed vascular segment (brachytherapy) and the use of sirolimus-coated stents have shown promising results in reducing coronary artery restenosis.31,32 It will be interesting to study the efficacy of these novel treatment strategies in vascular access thrombosis.
III. Hemostatic Complications of Solid Organ Transplantation
Julie Hambleton, MD*
Hemostasis and Thrombosis, Division of Hematology/Oncology, Department of Medicine, University of California, San Francisco, 505 Parnassus Avenue, M1286, San Francisco, CA 94143-1270
Dr. Hambleton has received an honorarium from NovoNordisk on the use of their product, recombinant VIIa.
Solid organ transplantations are being performed on an increasing number of patients at medical institutions throughout the world, and hematologists are frequently consulted to evaluate these patients. In this section, the hemostatic complications of solid organ transplantation, specifically perioperative hemorrhage, thromboembolic complications, and thrombocytopenia, will be discussed.
Perioperative Hemorrhage: Liver Disease and Transplantation
The most prominent hemostatic complication of solid organ transplantation is perioperative hemorrhage, which is most pronounced in patients undergoing liver transplantation. Each year, 4700 liver transplantations are performed in the United States, according to the United Network for Organ Sharing (UNOS).1 Excessive alcohol intake and the growing hepatitis C epidemic are resulting in an increased number of people being diagnosed with end-stage liver disease (ESLD). Currently, approximately 16,000 patients in the United States are on the UNOS waiting list for liver transplantation,1 a number that is expected to increase during the next decades.
Coagulopathy of Advanced Liver Disease
The acquired coagulopathy of liver disease contributes to the morbidity and blood loss encountered during liver transplantation. The liver synthesizes most of the coagulation proteins, both procoagulants and natural anticoagulants, and fibrinolytic proteins (Table 4 ). Perturbations in the hepatic synthesis or clearance of these proteins result in impaired thrombin generation and the formation of a less stable fibrin plug, which is easily degraded by the fibrinolytic system.
The degree of hemostatic defects in liver disease is proportional to the extent of liver parenchymal cell damage.2,3 Mild to moderate liver disease is associated with a slightly prolonged prothrombin time (PT) caused by a modest decrement in factor VII, a vitamin K–dependent coagulation factor with a short circulating half-life. More advanced liver disease is marked by additional factor decrements, including factors II, IX, and X. Fibrinogen and factor V levels fall below normal with more advanced liver disease. Factor VIII levels are often preserved in severe liver disease due to extra-hepatic synthesis. A dysfunctional fibrinogen molecule, or dysfibrinogenemia, has been described in patients with severe hepatitis.3 Elevations in the thrombin and reptilase times in the absence of fibrin(ogen) split products (FSPs) suggest the presence of a dysfibrinogenemia. The dysfunctional molecule is a result of abnormal modification of sialic acid residues that interfere with function and processing.
Fulminant hepatic failure is associated with activated fibrinolysis and impaired clot formation.3,4 Alpha 2-antiplasmin, the main natural inhibitor of plasmin, and plasminogen levels may be depressed with liver parenchymal damage. The activity of tissue plasminogen activator (t-PA), a fibrin-specific plasminogen activator synthesized and secreted by vascular endothelial cells, is inhibited by complex formation with plasminogen activator inhibitor (PAI-1), a protein synthesized by endothelial cells, hepatocytes, and platelets.5 Urokinase plasminogen activator (u-PA) is also synthesized by vascular endothelium and monocytes and excreted by the kidney.5 Normally, t-PA and the t-PA/PAI-1 complexes are rapidly cleared from circulation. However, activated hemostatic proteins are not well cleared by the diseased liver, and, as a result, plasma levels of u-PA and t-PA are elevated in patients with cirrhosis.6–,9 Moreover, PAI-1 levels may be lowered as a result of decreased production by the diseased liver and increased complex formation with t-PA. The net balance is one of a hyperfibrinolytic state, which is evident in some, but not all, patients with advanced liver disease. Shortened euglobulin clot lysis times, elevated FSP, and elevated D-dimers are seen in this hyperfibrinolytic state,3 as well as DIC.4 Differentiating advanced liver disease from primary fibrinolysis or DIC is difficult because of the overlap in laboratory findings with these 3 conditions. Elevation of fibrinopeptide A (FpA), thrombin/antithrombin complexes, plasmin/alpha 2-antiplasmin, and D-dimer levels suggests DIC is present.
Mild thrombocytopenia is typical in patients with liver disease as a result of consumptive splenomegaly. Decreased levels of thrombopoietin, a platelet growth factor made in the liver, are seen in patients with cirrhosis and advanced liver disease.10,11 This deficiency appears to correct with liver transplantation, resulting in a normal posttransplant platelet count despite little change in the degree of splenomegaly.11 Thrombocytopenia in the setting of cirrhosis may also be a result of folic acid deficiency, bone marrow alcohol toxicity, and consumption from subclinical DIC.4
Orthotopic Liver Transplantation and Coagulopathy
Orthotopic liver transplantation (OLT) is considered the only effective treatment for patients with acute or chronic end-stage liver disease.2 Improvements in immunosuppressive therapy, organ preservation, operative techniques, and anesthetic care have contributed to the marked reduction in morbidity and mortality associated with this procedure.2 However, massive bleeding and need for transfused blood products remain unpredictable problems in many cases.
The surgical procedure of liver transplantation is divided into three stages with respect to risk and cause of hemorrhage.12 During the preanhepatic stage, the host liver is surgically isolated. The extent of bleeding at this stage is related to preoperative patient characteristics, such as degree of hepatic dysfunction and cirrhosis, prior abdominal surgeries, surgical trauma, and amount of surgical dissection needed.12 Enhanced fibrinolysis during this first stage is encountered in 10–20% of patients with cirrhosis.12 The anhepatic phase begins with the surgical removal of the host liver. At this point, there is no hepatic function, and a venovenous bypass is used to decompress the portal circulation and maintain venous return.12 During this second stage, most major vessels are clamped, and there is minimal surgical bleeding. The etiology of blood loss at this stage is considered hemostatic due to DIC and hyperfibrinolysis.12–,14 The postanhepatic stage begins when the donor liver is reperfused by the host’s circulation and ends at the close of the operation. During this third stage, excessive bleeding is often encountered due to a heparin-like effect, hyperfibrinolysis, metabolic acidosis, hypothermia, electrolyte disturbances, and poor cardiac function.12,15
Perioperative Hemostatic Support in Liver Transplantation
A significant relationship between large transfusion requirements and postoperative morbidity and mortality has been recognized.2,16,17 Unfortunately, few modifiable variables predict operative blood loss other than surgical technique and control of coagulation abnormalities encountered pre- and intraoperatively.17–,22 Researchers are still trying to find the optimal combination of hemostatic agents to control the coagulopathy encountered intraoperatively. The majority of patients undergoing OLT receive packed red blood cells, whole blood, platelets, fresh frozen plasma, and vitamin K. Some patients receive cryoprecipitate if the presence of DIC, hypofibrinogenemia of any cause, or dysfibrinogenemia is suspected or confirmed. Polycythemia has been associated with an increased risk of hepatic artery thrombosis; therefore, the target postoperative hemoglobin is 8 to 9 g/L.15
In addition to blood products, the use of other hemostatic agents such as desmopressin (DDAVP), conjugated estrogen, fibrin sealants, amicar, aprotinin, and activated recombinant factor VII have been evaluated. Amicar may be administered to patients with evidence of hyperfibrinolysis.23 Caution should be exercised for patients with evidence of DIC.
Perioperative use of aprotinin has gained acceptance for patients undergoing coronary artery bypass. Its hemostatic utility in patients undergoing orthotopic liver transplantation has also been recognized. In a prospective, randomized, placebo-controlled study, intraoperative use of aprotinin was associated with a significant reduction in intraoperative blood loss and need for blood product administration.24 Patients who received 2 million units of aprotinin as a bolus followed by 1 million units/hour continuous infusion had a 60% reduction in intraoperative blood loss, while those who received a 50% lower continuous infusion rate had a 44% reduction in intraoperative blood loss. No significant increase in thromboembolic complications was reported.
NovoSeven® (rFVIIa) has been studied in patients with liver disease, and pilot studies have been completed in patients undergoing liver transplantation. Activated factor VII is the initiator of coagulation when tissue factor has been exposed at the site of injury. Activation of factor VII in this manner leads to activation of factor X and generation of thrombin, which, in turn, leads to generation of an insoluble fibrin clot. A pilot study to evaluate the hemostatic efficacy and safety of a single preoperative dose, 80 μg/kg, of rFVIIa during OLT suggested a decreased need for blood product transfusion in patients who received rFVIIa.25 A larger multicenter trial has been completed, but the results have not yet been presented. To date, no thrombotic or other safety concerns have been raised, although surveillance is prudent given the prior experience with the prothrombin complex concentrates. The cost of rFVIIa is approximately $972 for a 1.2 mg vial. The costs associated with rFVIIa use in patients with factor inhibitors and acute hemorrhagic events can be very high, particularly given the drug’s short half-life and need for frequent dosing over days to weeks. In the setting of fulminant hepatic failure and OLT, the cost:benefit ratio for rFVIIa use has not been established. If larger prospective studies confirm that one or several perioperative doses of rFVIIa are associated with a significant decrease in blood product usage, length of operation, and time of intensive care unit stay, then the cost:benefit ratio may favor rFVIIa.
Despite the well-described uremic coagulopathy of renal failure, renal transplantation is not associated with excessive intraoperative blood loss. Prior to the surgical procedure, the patient’s hemostatic function is optimized by performing dialysis. DDAVP may be administered as well. The main cause for perioperative hemorrhage during cardiac transplantation is the effect on platelet function due to hypothermia and prolonged bypass time, but hemorrhage is not a major factor in determining clinical outcome in this setting.
Posttransplant Hemostatic Complications
Polycythemia
Posttransplant erythrocytosis occurs in up to 17% of renal transplant recipients.15 The pathophysiology of posttransplant erythrocytosis is not fully understood, tends to be self-limited, and is more common in patients receiving cyclosporine-based immunosuppressive regimens than in those receiving azathioprine-based immunosuppressive regimens.26,27 While the risk of thromboembolic complications is increased in post–renal transplant patients with erythrocytosis, the hemoglobin level per se does not appear to correlate with the risk.27,28 Hematocrits that surpass the 50% threshold often result in the institution of phlebotomy. Treatment with angiotensin-converting enzyme (ACE) inhibitors may abrogate or lessen the erythrocytosis as well.29– 31
Thromboembolic Complications
Venous thromboembolic disease
Vascular complications of both large and small vessels can have devastating effects on the clinical outcome after organ transplant, whether the complication is thrombosis of a deep vein in the lower extremity with a pulmonary embolus (PE) or thrombosis of a surgical vessel or graft. In a retrospective study spanning 10 years, renal transplant patients were found to have an 8.3% incidence of venous thromboembolic disease, such as DVT or PE.15,32 Interestingly, the risk of postoperative DVT appeared to be greatest 4 months after the surgical procedure,32 implicating a mechanism other than the direct surgical trauma itself. Age, prolonged immobilization, use of steroids, and need for repeat surgery have been associated with an increased risk of developing a posttransplant DVT. In the 480 consecutive renal transplant patients reported by Allen et al, polycythemia did not appear to increase this risk.32 In a large retrospective review of 1833 renal transplant recipients and 276 patients who had undergone simultaneous kidney-pancreas transplantation, the incidence of DVT was 6.2% overall and 18.1% in patients who underwent simultaneous kidney-pancreas transplant.33 Risk factors for DVT identified by multivariate analysis included age > 40 years, diabetes mellitus, history of a prior DVT, and a combined transplant. In liver transplant recipients, the postoperative rate for DVT is 2.7% and for PE, 1%.34
The use of immunosuppressive agents has been linked to the development of postoperative DVT in the solid organ transplantation population. Renal transplant recipients receiving cyclosporine-based regimens are more likely to develop thromboembolic complications in the postoperative period than are recipients receiving azathioprine-based regimens.35
Classic thrombophilia risk factors may increase the risk of postoperative DVT in organ transplant recipients. Antiphospholipid antibodies36 and the factor V Leiden mutation37 appear to increase the risk in renal transplant recipients. However, in a retrospective review of 276 recipients of liver transplantation, factor V Leiden was not associated with hepatic artery thrombosis, portal vein thrombosis, or DVT.38 Interestingly, discordant postoperative findings of activated protein C resistance in the factor V Leiden mutation–negative recipients tested by peripheral blood have revealed that factor V Leiden heterozygote liver donors pass on the phenotype via liver transplantation.38– 41 This discrepancy can be demonstrated by positive testing of activated protein C resistance in the recipient, negative factor V Leiden testing of the recipient’s peripheral blood, and positive factor V Leiden testing in the donor’s liver (or donor’s peripheral blood, if available).
Graft thrombosis
Graft rejection and vessel thrombosis, two conditions that target the endothelium, remain major causes of early graft failure in those who have undergone solid organ transplantation. A surgically perturbed endothelium results in release of a number of hemostatic proteins into the circulation, including t-PA, PAI-1, and von Willebrand factor (VWF).42 An increase in the VWF-antigen-to-ristocetin cofactor ratio and in thrombin-antithrombin complex generation has been noted as a potential marker of the prothrombotic state in patients whose liver transplantation was complicated by graft thrombosis.42 In children undergoing liver transplantation, vascular complications may be as high as 21% and include hepatic artery thrombosis, portal vein thrombosis, and venous outflow tract obstruction.43 Early graft thrombosis after renal transplantation is an infrequent but devastating complication. While the incidence of graft thrombosis in this setting is estimated at 2%,44 salvage is rare.45 Risk factors for thrombosis include recipient age < 18 years, recipient vascular disease, and donor age > 55 years.46
Traditional thrombophilic risk factors, such as factor V Leiden and the lupus anticoagulant, which cause DVT and PE, have been associated with early graft thrombosis in transplant recipients.47,48 Because early graft thrombosis is associated with a high rate of morbidity, many of these patients undergo retransplantation. In a retrospective review of 16 patients who underwent retransplantation because of arterial or venous thrombosis and graft loss, 12 lost their primary kidney transplant because of renal vein thrombosis and 4 because of renal artery thrombosis.45 The thrombotic events occurred on average 3.6 days posttransplant. In the 5 patients who underwent a hypercoagulable evaluation, the antiphospholipid antibody was found in 3, and 1 had an elevated homocysteine level. While only these 5 patients underwent retransplant with postoperative DVT prophylaxis, none of the 16 patients who underwent retransplantation had a recurrent thrombotic complication.45
Graft rejection
Early and late graft rejection is strongly associated with the humoral and cellular immune response, yet vascular thrombotic complications are noted as well. Traditional thrombophilic risk factors such as factor V Leiden have been associated with early graft loss and rejection.49,50 Thrombotic risk and chronic graft rejection have been postulated as untoward complications of the immunosuppressive regimen, although conflicting reports on the role of cyclosporine have been described.27,51 The purported mechanism is abnormal coagulation and fibrinolysis.52 Depressed fibrinolysis has been associated with steroid therapy as well.53,54
Microangiopathy
Hemolytic uremic syndrome (HUS) developing de novo in recipients of organ transplantation is frequently attributed to the calcineurin inhibitors, cyclosporine and tacrolimus.55–,57 Decreased prostacyclin activity has been implicated in the pathogenesis of this disorder, and reduced production of prostacyclin by vascular endothelium has been postulated as a consequence of cyclosporine therapy. Interestingly, renal thrombotic microangiopathy has been noted in hepatitis C–positive renal allograft recipients in conjunction with anticardiolipin antibodies.58 HUS presents with a normocytic normochromic anemia, reticulocytosis with schistocytes seen on peripheral blood smear (Figure 4, see Color Figures, 520), elevation in lactate dehydrogenase, thrombocytopenia, and deteriorating renal function. Renal biopsy typically reveals fibrin deposition and glomerular thrombosis (Figure 5, see Color Figures, 520); small vessel thrombi are rarely found in other organs. The initial approach to treatment of posttransplant HUS includes a reduction in the dose of the calcineurin inhibitor. Transfusion of fresh frozen plasma and plasma exchange may be necessary for more advanced HUS. If HUS persists after reduction in the dose of calcineurin inhibitor, the drug and any others in its class should be avoided.
Thrombocytopenia
Thrombocytopenia in the hospitalized patient is very common and often drug induced (Table 5 ). Specific to recipients of organ transplants, many immunosuppressive agents—calcineurin inhibitors (cyclosporine, tacrolimus) and thiopurine analogs such as azathioprine—and other agents (such as antimicrobial, antifungal, and antiviral agents, heparin, and other miscellaneous drugs) cause thrombocytopenia and myelosuppression to varying degrees. Management of these patients is often difficult because alternative effective agents may be lacking.
One rare but devastating complication of liver transplantation with hemostatic implications is posttransplant aplastic anemia.59 The reported etiologies of posttransplant aplastic anemia include virally induced fulminant hepatic failure, graft-versus-host disease, parvovirus, and idiopathic aplasia.59 Management of patients with this complication includes reduction of calcineurin inhibitor therapy, administration of growth factors, antithymocyte globulin, steroids, blood product support, and occasionally bone marrow transplantation. Despite aggressive therapy, the mortality of this disorder is high, especially for those patients without fulminant hepatic failure, and the cause of death is often hemorrhagic.
Summary
Hemostatic complications of solid organ transplantation are common. Surgical hemorrhage due to underlying disease, postoperative large and small vessel thrombosis, chronic graft rejection, and thrombocytopenia all contribute to the morbidity and mortality of patients receiving solid organ transplants. In defining these hemostatic disorders’ etiology, deciding how best to manage them, and identifying ways to prevent them, hematologists play a critical role in helping transplantation teams improve clinical outcomes for these patients.
Clinical conditions that may be associated with disseminated intravascular coagulation (DIC).
| Sepsis/severe infection (any microorganism) |
| Trauma (e.g., polytrauma, neurotrauma, fat embolism) |
| Organ destruction (e.g., severe pancreatitis) |
| Malignancy |
| –solid tumors |
| –myeloproliferative/lymphoproliferative malignancies |
| Obstetrical calamities |
| –amniotic fluid embolism |
| –abruptio placentae |
| Vascular abnormalities |
| –Kasabach-Merritt syndrome |
| –large vascular aneurysms |
| Severe hepatic failure |
| Severe toxic or immunologic reactions |
| –snake bites |
| –recreational drugs |
| –transfusion reactions |
| –transplant rejection |
| Sepsis/severe infection (any microorganism) |
| Trauma (e.g., polytrauma, neurotrauma, fat embolism) |
| Organ destruction (e.g., severe pancreatitis) |
| Malignancy |
| –solid tumors |
| –myeloproliferative/lymphoproliferative malignancies |
| Obstetrical calamities |
| –amniotic fluid embolism |
| –abruptio placentae |
| Vascular abnormalities |
| –Kasabach-Merritt syndrome |
| –large vascular aneurysms |
| Severe hepatic failure |
| Severe toxic or immunologic reactions |
| –snake bites |
| –recreational drugs |
| –transfusion reactions |
| –transplant rejection |
Comparison of acute mesenteric arterial thromboembolism and mesenteric venous thrombosis.
| . | Arterial Thromboembolism . | Venous Thrombosis . |
|---|---|---|
| *Adapted from Kumar et al.2020 | ||
| Risk factors | Atherosclerotic vascular disease | Hypercoagulable states |
| Hypertension | Inflammatory bowel disease | |
| Smoking | Abdominal cancer | |
| Valvular heart disease | ||
| Atrial fibrillation | ||
| Clinical features | ||
| Age of patient | Older patients (60s-70s) | Younger patients (40s-50s) |
| Abdominal pain | Abrupt onset | Insidious onset |
| Diagnostic tests | Mesenteric angiography usually required | Abdominal computed tomography scan |
| Anatomic involvement | Superior and inferior mesenteric arteries | Superior mesenteric veins |
| Therapy | ||
| Surgery | Revascularization +/– bowel resection | Observation; surgery generally not required |
| Thrombolysis | Sometimes useful | Generally not useful |
| Long-term anticoagulation | Indicated | Indicated |
| Prognosis | High acute mortality rate | Better prognosis |
| Long-term sequelae | Short bowel | Short bowel |
| Varices | ||
| . | Arterial Thromboembolism . | Venous Thrombosis . |
|---|---|---|
| *Adapted from Kumar et al.2020 | ||
| Risk factors | Atherosclerotic vascular disease | Hypercoagulable states |
| Hypertension | Inflammatory bowel disease | |
| Smoking | Abdominal cancer | |
| Valvular heart disease | ||
| Atrial fibrillation | ||
| Clinical features | ||
| Age of patient | Older patients (60s-70s) | Younger patients (40s-50s) |
| Abdominal pain | Abrupt onset | Insidious onset |
| Diagnostic tests | Mesenteric angiography usually required | Abdominal computed tomography scan |
| Anatomic involvement | Superior and inferior mesenteric arteries | Superior mesenteric veins |
| Therapy | ||
| Surgery | Revascularization +/– bowel resection | Observation; surgery generally not required |
| Thrombolysis | Sometimes useful | Generally not useful |
| Long-term anticoagulation | Indicated | Indicated |
| Prognosis | High acute mortality rate | Better prognosis |
| Long-term sequelae | Short bowel | Short bowel |
| Varices | ||
Factors synthesized by the liver.
| Procoagulant proteins | Vitamin K-dependent: II, VII, IX, X |
| Factors V, VIII, XI, fibrinogen | |
| Anticoagulant proteins | Antithrombin, protein C, protein S |
| Fibrinolytic proteins | Plasminogen, plasminogen activator inhibitor 1 (PAI-1), alpha 2-antiplasmin |
| Miscellaneous | Thrombopoietin, protein Z |
| Procoagulant proteins | Vitamin K-dependent: II, VII, IX, X |
| Factors V, VIII, XI, fibrinogen | |
| Anticoagulant proteins | Antithrombin, protein C, protein S |
| Fibrinolytic proteins | Plasminogen, plasminogen activator inhibitor 1 (PAI-1), alpha 2-antiplasmin |
| Miscellaneous | Thrombopoietin, protein Z |
Drugs commonly used in solid organ transplantation that are associated with thrombocytopenia.
|
|
Schematic representation of pathogenetic pathways in DIC.
During systemic inflammatory response syndromes, both perturbed endothelial cells and activated mononuclear cells may produce proinflammatory cytokines that mediate coagulation activation. Activation of coagulation is initiated by tissue factor expression on activated mononuclear cells and endothelial cells. In addition, downregulation of physiological anticoagulant mechanisms and inhibition of fibrinolysis by endothelial cells will further promote intravascular fibrin deposition. PAI-1 indicates plasminogen activator inhibitor, type 1.
Schematic representation of pathogenetic pathways in DIC.
During systemic inflammatory response syndromes, both perturbed endothelial cells and activated mononuclear cells may produce proinflammatory cytokines that mediate coagulation activation. Activation of coagulation is initiated by tissue factor expression on activated mononuclear cells and endothelial cells. In addition, downregulation of physiological anticoagulant mechanisms and inhibition of fibrinolysis by endothelial cells will further promote intravascular fibrin deposition. PAI-1 indicates plasminogen activator inhibitor, type 1.
Point of impact of the three major physiological anticoagulant pathways.
Antithrombin is the most important inhibitor of thrombin and factor Xa, activated protein C is able to degrade the essential cofactors Va and VIIIa, and tissue factor pathway inhibitor (TFPI) inhibits the tissue factor/factor VIIa complex.
Point of impact of the three major physiological anticoagulant pathways.
Antithrombin is the most important inhibitor of thrombin and factor Xa, activated protein C is able to degrade the essential cofactors Va and VIIIa, and tissue factor pathway inhibitor (TFPI) inhibits the tissue factor/factor VIIa complex.
Dysfunction of the protein C system in disseminated intravascular coagulation (DIC) is due to low levels of zymogen protein C, downregulation of thrombomodulin and the endothelial protein C receptor, and low levels of free protein S due to acute phase-induced high levels of its binding protein (i.e., C4b-binding protein).
Dysfunction of the protein C system in disseminated intravascular coagulation (DIC) is due to low levels of zymogen protein C, downregulation of thrombomodulin and the endothelial protein C receptor, and low levels of free protein S due to acute phase-induced high levels of its binding protein (i.e., C4b-binding protein).