AML and related precursor neoplasms, and acute leukemias of ambiguous lineage7
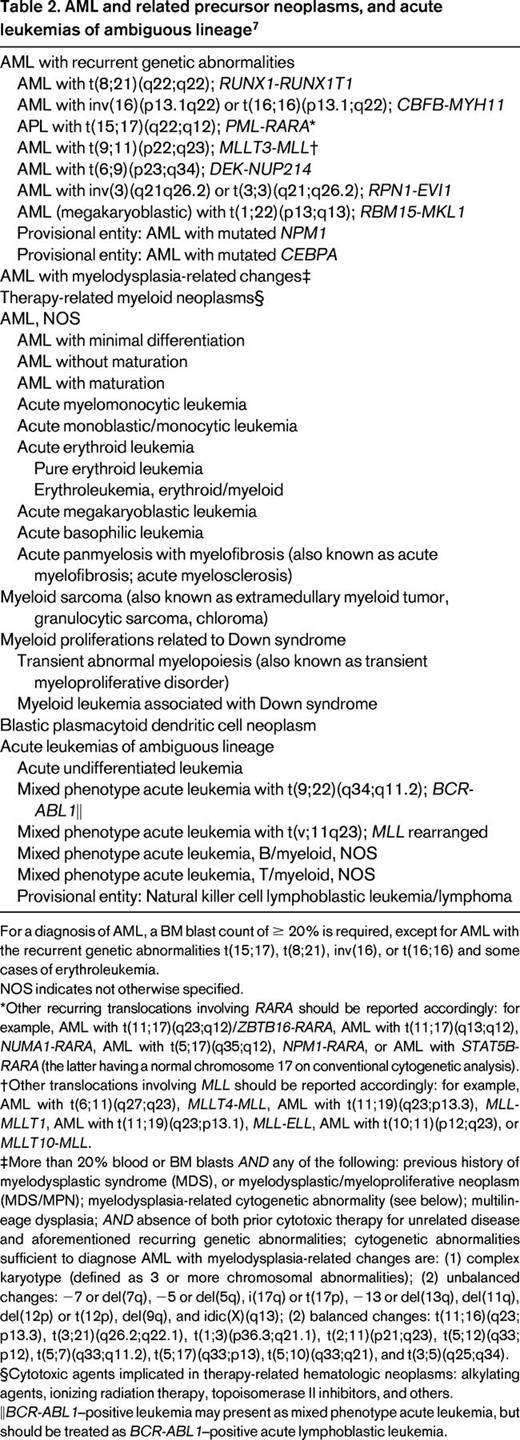
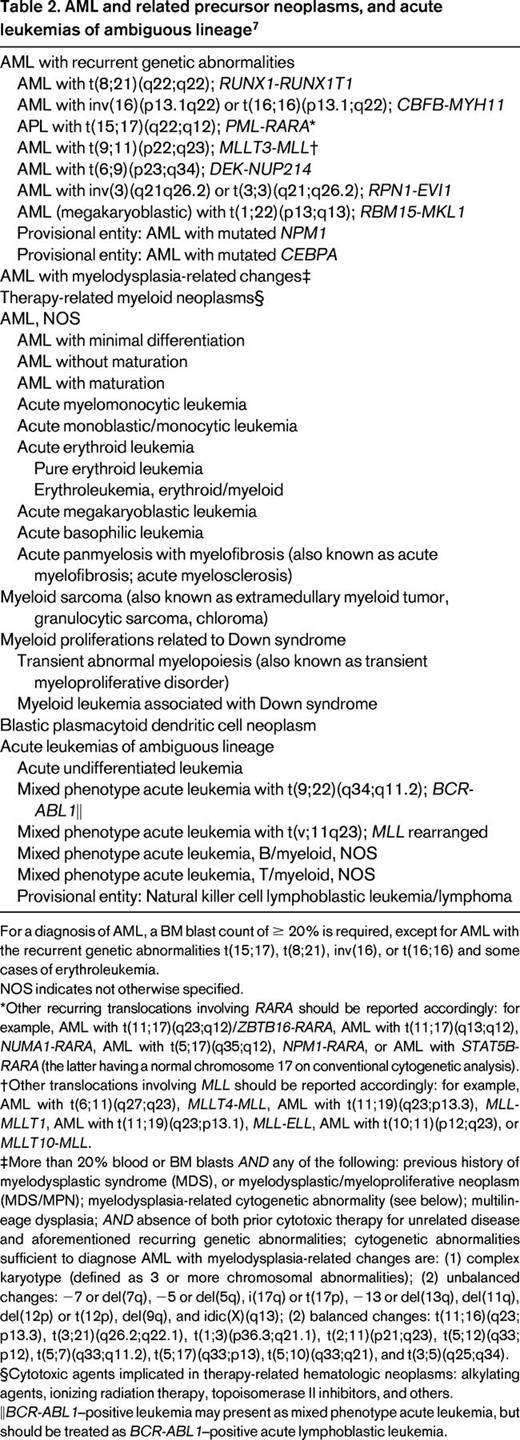
For a diagnosis of AML, a BM blast count of ≥ 20% is required, except for AML with the recurrent genetic abnormalities t(15;17), t(8;21), inv(16), or t(16;16) and some cases of erythroleukemia.
NOS indicates not otherwise specified.
*Other recurring translocations involving RARA should be reported accordingly: for example, AML with t(11;17)(q23;q12)/ZBTB16-RARA, AML with t(11;17)(q13;q12), NUMA1-RARA, AML with t(5;17)(q35;q12), NPM1-RARA, or AML with STAT5B-RARA (the latter having a normal chromosome 17 on conventional cytogenetic analysis).
†Other translocations involving MLL should be reported accordingly: for example, AML with t(6;11)(q27;q23), MLLT4-MLL, AML with t(11;19)(q23;p13.3), MLL-MLLT1, AML with t(11;19)(q23;p13.1), MLL-ELL, AML with t(10;11)(p12;q23), or MLLT10-MLL.
‡More than 20% blood or BM blasts AND any of the following: previous history of myelodysplastic syndrome (MDS), or myelodysplastic/myeloproliferative neoplasm (MDS/MPN); myelodysplasia-related cytogenetic abnormality (see below); multilineage dysplasia; AND absence of both prior cytotoxic therapy for unrelated disease and aforementioned recurring genetic abnormalities; cytogenetic abnormalities sufficient to diagnose AML with myelodysplasia-related changes are: (1) complex karyotype (defined as 3 or more chromosomal abnormalities); (2) unbalanced changes: −7 or del(7q), −5 or del(5q), i(17q) or t(17p), −13 or del(13q), del(11q), del(12p) or t(12p), del(9q), and idic(X)(q13); (2) balanced changes: t(11;16)(q23;p13.3), t(3;21)(q26.2;q22.1), t(1;3)(p36.3;q21.1), t(2;11)(p21;q23), t(5;12)(q33;p12), t(5;7)(q33;q11.2), t(5;17)(q33;p13), t(5;10)(q33;q21), and t(3;5)(q25;q34).
§Cytotoxic agents implicated in therapy-related hematologic neoplasms: alkylating agents, ionizing radiation therapy, topoisomerase II inhibitors, and others.
‖BCR-ABL1–positive leukemia may present as mixed phenotype acute leukemia, but should be treated as BCR-ABL1–positive acute lymphoblastic leukemia.