TO THE EDITOR:
Sickle cell trait (SCT) results from the inheritance of the HBB gene variant (hemoglobin S [HbS]) from 1 parent, whereas the other HBB gene is normal that results in HbA (normal hemoglobin). In the United States, ∼7% of African Americans have SCT, and it is less frequent in other ethnic populations in the United States. Among individuals with SCT, HbA typically accounts for 55% to 65% and HbS for 35% to 45% of total hemoglobin (Hb), which is determined by high-performance liquid chromatography or other methods. SCT does not cause chronic hemolysis.1 Individuals with SCT have a normal life span compared to Black individuals without SCT.2 Despite these medical facts, significant confusion exists regarding the role of SCT and morbidity.
Since at least 1977, pathologists have recognized that the presence of sickled red blood cells in individuals with SCT during postmortem examinations is an artifact resulting from hypoxemia and acidosis. Both hypoxemia and acidosis, often occurring immediately before and after death, are 2 physiologic conditions known to cause Hb polymerization in individuals with SCT, resulting in sickle-shaped blood cells.3,4 Thus, postmortem presence of sickle red blood cells in an individual with SCT is expected to occur. In an expert testimony before a grand jury in Illinois, Bowman, Professor of Pathology at the University of Chicago, was clairvoyant when he expressed concern that the postmortem artifact of sickle red blood cells being identified “could lead to an unfortunate precedent for persons with SCT.”5 Bowman explains the basis for his prescient concern:
A man who had sickle cell trait was allegedly beaten and strangled and suffocated with a blanket by guards in a prison hospital during the process of subduing violent acts of the prisoner. Merely because sickle cells were found intravascularly at postmortem examination, the Cook County coroner and a consultant medical examiner from another state claimed that death was the result of a sickle cell crisis after pressure on the neck, which led to hypoxia. The forensic pathologists also stated that the slight nature of some external injuries on the neck led them to believe that if the prisoner had normal hemoglobin, he would not have died.
My testimony was that the postmortem findings were compatible with asphyxia and that the presence of intravascular sickle cells had no pathological significance. I also challenged the opinion that severe neck bruises must be present for death from suffocation or strangulation and offered to demonstrate that I could render the expert medical examiner unconscious without leaving bruises on his neck. I later learned that the guards were not indicted. Thus, the dangerous precedent for legalized murder of persons with sickle cell trait could become established because intravascular sickling is found post mortem in the tissues of most persons with sickle cell trait. A defense lawyer may use the evidence of intravascular sickling in a victim to obtain a reduction in the severity of a murder charge of his client.
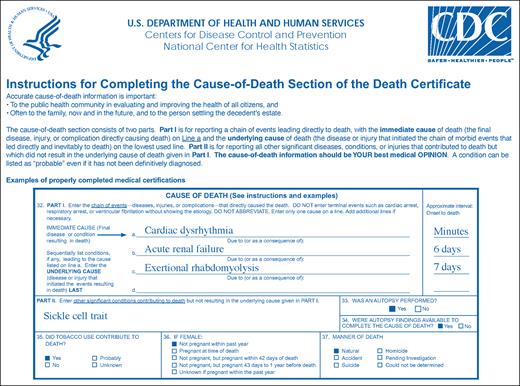
Why might there be mislabeling of sickle cell crises or SCT listed as a cause of death on the death certificate? The most straightforward answer is that, as the clinical history of sickle cell disease (SCD) and SCT evolved over the last 40 years, there have been limited educational campaigns to educate the community at large and the medical-legal community about medical myths and medical facts concerning SCD vs SCT. In 1970, one of the earliest case series was published in the New England Journal of Medicine, attributing SCT and sickle cell acute pain crises to sudden death; 4 men who died had the following features: (1) physical exertion during military training at an altitude of 4060 ft; (2) laboratory findings associated with acute kidney injury; (3) death occurred in 1 individual in <1 hour; and (4) the presence of intravascular sickled cells were identified post mortem in all 4 cases.6 The authors characterized the deaths as sudden and attributable to sickle trait. The American Heart Association describes natural death due to cardiac causes, heralded by abrupt loss of consciousness within 1 hour of the onset of acute symptoms; preexisting heart disease may have been known to be present, but the time and mode of death are unexpected.7 Based on current medical knowledge, the deaths of 3 individuals would not be classified as sudden, and none of the deaths were from SCT. The literature is replete with similar case reports or case series describing sudden death due to SCT, with manuscripts that include titles combining SCT and sudden death based on postmortem findings. The most cited article attributing sudden death to SCT is from the US Army.8 Another possibility is that the death certificate is completed incorrectly, when SCT is put in as a primary or secondary cause of death and not a contributing cause of death (appropriate example provided in Figure 1).9
The Centers for Disease Control death certificate instructions with an example for an adult with SCT, who died of exertional rhabdomylosis temporally related to death.
The Centers for Disease Control death certificate instructions with an example for an adult with SCT, who died of exertional rhabdomylosis temporally related to death.
To critically assess the medical validity of listing SCT, acute sickle cell crises, or both on the autopsy report as a cause of death in individuals with SCT, the American Society of Hematology (ASH) convened an expert panel of hematologists and forensic pathologists to systematically review the literature to determine the validity of sickle cell crises and exertion-related mortality in individuals with SCT.10 After systematically reviewing 1474 citations, the panel found no studies comparing uncomplicated acute sickle cell pain crises in individuals with SCT to those with SCD. Given that sickle cell crisis is not identified as a clinical entity in individuals with SCT, there can be no evidence that sickle cell crisis is responsible for death in individuals with SCT. The US Army conducted the most rigorous study to assess the established increased risk of exertional rhabdomyolysis and its sequelae, including death. After introducing universal precautions, exertional rhabdomyolysis continued to occur at higher rates in Black individuals with SCT compared to Black individuals without SCT. However, the rate of death was no higher in those with SCT.11
The ASH panel did not address other rare events that may occur at a higher rate in individuals with SCT, such as splenic infarction, particularly in hypoxic environmental conditions, hematuria,12 renal medullary carcinoma,13 pulmonary embolism, proteinuria, and chronic kidney disease.14,15 The ASH panel also did not discuss a crush injury that may result in rhabdomyolysis in individuals with or without SCT.16,17 The history of an individual's clinical demise is not attributable to SCT but rather the crush injury that may result from a physical altercation that directly leads to rhabdomyolysis and its sequelae, a distinct clinical entity compared to exertional rhabdomyolysis.18-20 A genetic predisposition plus the presence of SCT may increase the likelihood of exertional rhabdomyolysis; however, the evidence for a genetic predisposition is currently limited to case reports and case series.21-25
In summary, if a person with SCT has unremitting or episodic severe pain, a thorough history, examination, and laboratory evaluation should be undertaken to find a cause other than SCT. Similarly, if SCT is listed as a cause of death, other causes should be considered, such as exertional rhabdomyolysis, sudden cardiac death, or asphyxia. Neither SCT nor sickle crises are medically credible causes of death and should not be listed on the death certificate of individuals with SCT. A multidisciplinary campaign is needed to educate the public, as well as the hematology, pathology, and legal communities, about the distinct medical implications of SCT and the differences between SCT and SCD. Lastly, with a focus on individuals with SCT, hematology and pathology academic communities have an opportunity to investigate the interactions and outcomes of SCT in relation to symptoms, morbidity, and causes of death.
Contribution: M.R.D. conceived of the summary, wrote the initial draft, and approved the final draft; and C.J.H. and Y.M.M. reviewed each draft and made changes to the final draft.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Michael R. DeBaun, Department of Pediatrics, Vanderbilt-Meharry Sickle Cell Disease Center of Excellence, Vanderbilt University Medical Center, 2525 West End Ave, Ste 750, Nashville, TN 37203; email: m.debaun@vumc.org.